Abstract
Pechuel-loeschea leubnitziae is an aromatic and unpalatable shrub traditionally used to treat malaria and related symptoms in some regions of Namibia. Despite the importance of P. leubnitziae in the management of malaria, no studies have evaluated the antiplasmodial activities of this putative antimalarial plant. In this study, antiplasmodial activity was measured using parasite lactate dehydrogenase assay. The dichloromethane crude extract of the plant showed marginal antiplasmodial activity with an IC50 of 7.24 µg/ml against Plasmodium falciparum 3D7 strain. Two fractions, Npk1 F70-77 and Npk1 F78-90, isolated from the extract exhibited enhanced antiplasmodial activity with IC50 values of 2.42 ± 0.48 µg/ml and 2.29 ± 0.32 µg/ml, respectively. The fractions were cytotoxic to Chinese hamster ovary mammalian cells (IC50 = 2.75 µg/ml and 2.22 µg/ml for NPk1 F78 and Npk1 F70, respectively). Gas chromatography–mass spectrometry, Fourier transform infrared and nuclear magnetic resonance spectroscopy confirmed that the antiplasmodial fractions of P. leubnitziae contain xerantholide (246 g/mol). This is the first report linking xerantholide to antiplasmodial and cytotoxic fractions of P. leubnitziae. Results of this study may contribute to the discovery of new drugs from this indigenous Namibian plant.
Similar content being viewed by others
1 Introduction
Pechuel-loeschea leubnitziae, commonly known as wild sage, bitterbush and stinkbush in English; bitterbos in Afrikaans; and Oshizimba in the Oshiwambo language of Namibia, is a multi-stemmed and aromatic plant indigenous to Southern Africa [28]. The vernacular names connote the very bitter taste and the aromatic nature of the plant extracts. The only species in the genus, P. leubnitziae occurs in some parts of southern Angola, Botswana, Eswatini, Namibia, northern regions of South Africa and Zimbabwe [28]. In Namibia, the plant is dominant near the Olushandja Dam of north-central Namibia [2]. According to Theron et al. [29], P. leubnitziae occurs on the flood plains between the Klipneus area and Rooibank. The plant is found throughout Namibia except in the far north-eastern part of the country [19].
Pechuel-loeschea leubnitziae has a chamaephyte growth form. It is a shrub with silver–grey felt-like pubescence on stems and leaves, with leaves tapering petiole-like towards the base, lanceolate, entire and up to about 3 cm long [32]. Since it is a woody species with perennating buds close to the ground, P. leubnitziae is fairly resistant to burning and it sprouts from the base after the above-ground biomass is burnt. Pechuel-loeschea leubnitziae produces a large number of small and wind-dispersed seeds which dominate the soil seed bank particularly in regions where the plant has extensive above-ground cover.
Pechuel-loeschea leubnitziae is often used in folk medicine to treat various diseases. An initial report by Van Damme et al. [31] and recent accounts by Chinsembu et al. [8] and Mumbengegwi et al. [21] aver that an extract of this plant’s leaves is taken orally to treat gonorrhoea, fever, colds, and chest as well as stomach pains. The plant’s vapour is inhaled by the patient during body steaming for the treatment of colds and coughs. Topical applications of fresh leaf extracts of P. leubnitziae are used to treat measles and as disinfectant for wounds. When the leaves are warmed, they can be used as a poultice to relieve painful feet and headaches. An extract of the root is also taken orally as a remedy for tuberculosis.
In Namibia, many tribes traditionally use P. leubnitziae for different medicinal purposes. The Herero people of use boiled leaves as a steam bath to delay menstruation [32]. The Ovahimba people in the Kunene Region near Angola use finely ground roots mixed with fat as cosmetics [10]. Regardless of the plant’s bitter taste, cold water root extracts are used as a remedy for cough, and boiled leaves are used as steam to alleviate malaria symptoms such as higher fever and headaches among the Owambo people [16, 22]. Pechuel-loeschea leubnitziae is also used and regarded as an effective mosquito repellent [24].
The highest incidence of malaria in Namibia (56.3%) is in Rundu [8], with 10,501 reported cases in the Kavango East and West regions [3]. Despite the use of P. leubnitziae in the relief of malaria in Namibia, no studies have evaluated the in vitro antiplasmodial activities of this putative antimalarial plant. Using a bio-assay guided fractionation approach, the aims of the current study were to: test the in vitro activity of P. leubnitziae extracts against Plasmodium falciparum, elucidate antiplasmodial fractions and active compounds, and to determine their cytotoxicity.
2 Materials and methods
2.1 Extract preparation and in vitro screening for antiplasmodial activity
The plant materials used were collected on 25 March 2016 near Rundu town (geographical coordinates 17.64940 S, 015.95758 E) in Kavango East region of Namibia. The plant’s voucher number is NPK13 and its documentation, identification, and authentication was done by the curator Leevi Nanyeni of the National Herbarium at the National Botanical Research Institute of Namibia.
The plant aerial materials were dried and ground to fine powder. Twenty grams were extracted sequentially with 200 ml of each of the following organic solvents in their increasing order of polarity: hexane, dichloromethane (DCM) and methanol. The samples were left on a shaker for 48 h and filtered through Whatman no. 4 filter paper. The extraction process was repeated sequentially with organic solvents: hexane, DCM, ethyl acetate and methanol, in their increasing order of polarity. The filtrates subsequently evaporated using a rotary evaporator (Heidolph GI, Germany) at 60 °C. The extracts were dried in the fume hood, weighed, placed in sterile sample bottles and stored in a refrigerator until required for use. The DCM extract which shows antiplasmodial activity had a yield of 3.70 percentage per 20 grams.
2.2 Cultivation of malaria parasites
The P. falciparum parasites (3D7 chloroquine (CQ)-sensitive strain) acquired from the Council for Scientific and Industrial Research (CSIR), Pretoria, South Africa. The parasites were cultured as described by Trager and Jensen [30] with minor modifications. The parasites were maintained in RPMI 1640 (BioWhittaker) culture medium supplemented with phenol red, albumax II (bovine serum albumin) (Gibco) (25 g/L), HEPES (N-[2-hydroxyethyl]-piperazine-N’-[2-ethansulphonic acid]) (6 g/L), 4.25% of sodium bicarbonate and gentamycin (50 mg/L). The parasites were cultured in sealed flat bottom flasks and maintained in washed O+ human red blood cells (RBC) at 37 °C in an atmosphere of 93% N2, 4% CO2 and 3% O2. The haematocrit and parasitaemia were kept between 2 and 4% by diluting with red blood cells. The parasitaemia was determined microscopically using a Giemsa stained thin blood smear of culture on the slide.
2.3 Antiplasmodial activity
Stock solutions of 20 mg/ml were made in 100% dimethyl sulfoxide (DMSO) and the samples were screened at 100–5.13 × 10−3 µg/ml for concentration–response (threefold dilution). The solvent control, DMSO, was also screened at corresponding concentrations of the test samples with the starting concentration of 1% DMSO at 100 µg/ml. The extracts were screened for in vitro antiplasmodial activity at full dose concentrations against the parasites.
The 50% inhibitory activity (IC50 values) was determined using the parasite lactate dehydrogenase (pLDH) assay [20]. Threefold dilutions were carried out in complete RPMI 1640 culture media in a 96-well plate at a starting concentration of 200 µg/ml. The parasite at trophozite stage (2% parasitemia) was then added and incubated for 48 h at 37 °C in an atmosphere of 93% N2, 4% CO2, and 3% O2. After incubation, parasite viability relative to the untreated controls was measured by pLDH assay, whereby the density of the parasite is indicated by production of quantifiable purple crystals of formazan salt. Concentration–response curves were obtained by plotting percentage parasite survival against the logarithm of the concentration using the GraphPad Prism software (GraphPad software, Inc., California, USA). The 50% inhibitory activities (IC50 values) were derived from concentration–response curves. Chloroquine (1000–0.051 ng/ml) was used as a positive control, and its IC50 against the sensitive strain ranges between 7 and 15 ng/ml.
2.4 Fractionation of antiplasmodial extracts by column chromatography
The DCM extract, which exhibited highest antiplasmodial activity, was fractionated using column chromatography. Silica (0.063–0.200 mm) was mixed with hexane to make a slurry, which was poured into a glass column (60 × 4 cm) and left to settle. The extract was dissolved (20 mg/ml) in 5 ml DCM/Hexane (9:1) and added onto the column, then washed with 50 ml hexane to wash out the DCM. The wash was collected in 20 ml in the first 2 glass tubes. The wash was followed by a slow and constant drop by drop flow of 200 ml of mobile phase: DCM/Hexane (60:40) at flow rate of ~ 65 drops per minute. The polarity of the mobile phase was then increased to DCM/MeOH (9:1). A total of 117 fractions of 10 ml each were collected.
Thin layer chromatography (TLC) was performed on Whatman aluminium sheets coated with a 0.2 mm layer of silica (Si gel 60). TLC was used to determine the profiles of the eluted fractions generated from column chromatography. Fractions were spotted on the TLC sheets using 10 μl capillary tubes. TLC plates were developed in TLC Tank in the mobile phase DCM/Hexane/EtOAc (6:3:1). The polarity of the mobile phase was increased to a DCM/Hexane/MeOH (6:2:2) solvent system for the more non-polar fractions generated. The TLC plates were viewed under 254 nm and 365 nm UV light. Fractions with similar TLC profile were pooled together, which then yielded a total of 91 fractions including the wash, which was the last fraction.
2.5 Cytotoxicity assay
Determination of cytotoxicity for antiplasmodial active compounds was done using Chinese hamster ovary (CHO) cell lines which were procured from Cellonex, South Africa. The cells were cultivated in Dulbecco’s modified Eagle medium (DMEM) and F-12 HAMS medium (1:1), supplemented with 10% foetal bovine serum and 0.6% streptomycin. Cells were plated at a concentration of 1 × 10-5 cells/ml and incubated in a 5% CO2 incubator for 24 h to adhere. Medium was aspirated and cells were incubated with tenfold serial dilutions (0.001–100 µg/ml) of test samples for further 48 h. After the incubation, cell viability relative to untreated controls was determined using a colorimetric MTT assay, and the IC50 (50% inhibition of cell viability) value was derived from concentration–response curves. Emetine was used as positive control. IC50 of emetine ranges between 0.04 and 0.06 ug/ml. Fractions were 100-fold less toxic than emetine against CHO cells.
2.6 Structure elucidation
Structure elucidation of antiplasmodial active compounds was done using standard procedures for gas chromatography–mass spectrometry (GC–MS), Fourier transform infrared (FTIR) and nuclear magnetic resonance (NMR) spectroscopy. For GC–MS analysis, the sample was dissolved in DCM. Following the method of Karpagasundari and Kulothungan [17], GC–MS analysis was carried out on Shimadzu 2010 plus comprising AOC-20i auto sampler. The operating conditions used for GC–MS spectrometry are shown in the supplementary material Appendix A1. For the NMR, the sample was dissolved in deuterated chloroform (CDCl3). Varian 400 MHz spectrometer at 300 K was used; coupling constant is given in Hertz (Hz). Chemical shift values are given as δ (ppm) relative to TMS (1H and 13C) as internal standard. Parameters used for Fourier transform infrared (FTIR) spectroscopy are provided in supplementary material Appendix A2.
3 Results and discussion
The DMSO solvent control had no effect on the parasites When P. leubnitziae extract (Npk-1D) was screened against the 3D7 strain of P. falciparum, it showed marginal activity with an IC50 = 7.24 µg/ml (Fig. 1). Two compounds (Npk1 F70-77 and Npk1 F78-90) isolated from P. leubnitziae extract (Npk-1D). showed in vitro antiplasmodial activity against the 3D7 strain (Fig. 2). The two compounds were isolated in crystal form, and their TLC profiles is shown in (Fig. 3). Chloroquine showed IC50 of 8.09 ng/ml; thus, the purified compounds were less active by 3000-fold compared to CQ against the sensitive strain. Cytotoxicity assays revealed that the isolated compounds are toxic to the mammalian CHO cells, with IC50 values of 2.747 µg/ml for Npk1 F78-90 and IC50 2.524 µg/ml for Npk1 F70-77 (Fig. 4). Stated differently, the compounds were not selective for the P. falciparum; the desirable selectivity being 10 and above and the selectivity index = IC50 plasmodial activity/IC50 cell activity. The IC50 and Z’-factors of test Npk-1D fractionated samples and two compounds against 3D7 strain of P. falciparum are found on (Table 1).
The functional groups within the chemical structure are defined as Vmax (KBr)/cm-1 2967(C–15 and C-14 2 X CH3) 2892(C–13 C = CH2), 1755(C–12 O–C = O), 1688(C–3 C = O), 1632(C–5 C = C).
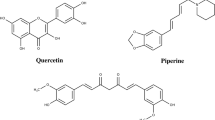
GC–MS revealed that the two compounds (Npk1 F70-77 and Npk1 F78-90) were actually one compound which was identified as xerantholide (Fig. 5), with a molecular weight of 246.3042 g/mol. Table 2 shows the 1H NMR and 13C NMR data of xerantholide (400 MHz, CDCl3). Due to the chiral centres at position 1, 7, 8 and 10, it means the compound has diasteromers. There is, however, a mixture of similar compounds with different conformations or orientations of the groups attached. FTIR spectra revealed five functional groups within the chemical structure and are identified as (C–15 and C–14 2 X CH3), (C–13 C = CH2), (C–3 C = O) and (C–5 C = C) which are resonating at 2967, 2892, 1755, 1688 and 1632, respectively. Xerantholide is a sesquiterpenic lactone found in the aerial parts of P. leubnitziae [1]. It was first isolated from the aerial parts of the Xeranthemum cylindraceum in 1977 [26]. The 1H NMR spectral data for the compound elucidated by Bohlmann and Borthakur [1] are not much different from the result of this study (Table 2). The difference in the data might be due to the presence of enantiomers on the elucidated compound in this study.
In 1982, xerantholide was also isolated from Anthemis austriaca [14]. The probable precursor of xerantholide is a 11,13-dihydro derivative methyl pechueloate and two norsesquiterpenes, probably formed by degradation of the corresponding sesquiterpene acid [1, 11]. A mixture of diasteromers with different conformations and orientations due to the various functional groups attached to it; xerantholide is difficult to separate completely [1]. During chemical transformation of xerantholide, two members of a diastereomic pair exhibited different chemical and physical properties [34]. Good single crystals of the hydroxyl derivatives could not be prepared and molecular models did not provide a definitive rationalization; hence, structural analysis was suggested [34].
A number of sesquiterpene lactones have been shown to possess in vitro activity against protozoans including P. falciparum, Trypanosoma brucei rhodesiense, Trypanosoma cruzi and Leishmania donovani [27, 35]. The most active sesquiterpene lactones had IC50 values between 0.1 and 0.4 μM, and their activity significantly correlated with cytotoxicity against L6 cells [35]. The major determinant for activity was α,β-unsaturated carbonyl groups which are known to act as Michael acceptors for biological nucleophiles [18].
Xerantholide is listed among the 96 natural product fragments that have different chemotypes. It is one of the sesquiterpene lactones which share the same carbon backbone as the antimalarial drug artemisinin [33]. Malaria is common in persons living with HIV [4], and plants traditionally used to treat malaria are also important in the management of HIV/AIDS [5, 6, 9]. Given that artemisinin is an inhibitor of HIV-1 reverse transcriptase [7], P. leubnitziae extracts containing xerantholide may be useful in the management of HIV/AIDS.
Although xerantholide is reported as a biologically active sesquiterpene lactone from the Asteraceae family [15], no previous reports have linked this compound for the in vitro antiplasmodial activity. In Namibia, P. leubnitziae has been studied for its in vitro antibacterial and antioxidant activities and it was found to have antioxidant function and activity against five laboratory bacterial strains [24]. These benefits might be due to the presence of anthraquinones, saponins, terpenoids, coumarins, alkaloids and flavonoids. Bohlmann and Borthakur [1] also reported that aerial parts of P. leubnitziae contain thymohydroquinone dimethyl ether, sitosterol, stigmasterol and xerantholide.
A new sesquiterpene lactone geigerianoloide is present in Geigeria alata, a plant traditionally used to control diabetes [12]. Many sesquiterpene lactones isolated from the family Asteraceae are known to have antiplasmodial and cytotoxic activities, but the antiplasmodial activity of xerantholide has not been reported before. This is the first study to show direct empirical evidence that P. leubnitziae exerts antiplasmodial activity in vitro. This is also the first study to demonstrate that the antiplasmodial and cytotoxic fractions of P. leubnitziae contain xerantholide.
Previous studies have shown that xerantholide has pleiotropic effects. In Namibia, P. leubnitziae is also used as a mosquito repellent [24]. The use of P. leubnitziae to repel mosquitoes is warranted because Nawrot et al. [23] also showed that xerantholide isolated from Xeranthemum cylindraceum acts as a good deterrent and an antifeedant to beetles that infest stored grain. Sesquiterpene lactones are known to have cytotoxic and anti-inflammatory activities [25]. Xerantholide exhibits cytostatic activity against HeLa and KB tumour cells as reported by [11, 13]. This is consistent with our findings that fractions imbued with xerantholide are cytotoxic to CHO cells in addition to the use of P. leubnitziae to treat inflammatory diseases in Namibia [16]. Overall, we postulate that xerantholide is the main antiplasmodial principle in P. leubnitziae. We also suggest that the antiplasmodial fractions are cytotoxic to cells due to the presence of xerantholide. This is the first chemical description related to the antiplasmodial activity of P. leubnitziae (family Asteraceae), a plant traditionally used to treat malaria in Namibia.
4 Conclusions
The study showed that P. leubnitziae extracts and fractions have in vitro activity against P. falciparum. However, the antiplasmodial fractions were cytotoxic, most likely due to the presence of xerantholide. This is the first study to show that antiplasmodial and cytotoxic fractions of P. leubnitiziae contain xerantholide. While the results of this study support the putative use of this plant as a remedy for malaria in Namibia, the lack of selectivity and cellular safety exhibited by the antiplasmodial principles would urge caution in the consumption of the plant. Further studies on the plant’s genotoxicity and chronic toxicity are needed to balance its safety when used as an oral remedy for malaria. It is recommended that pharmacomodulation studies should be carried out on xerantholide in order to decrease the compound’s toxicity while maintaining or improving its activity. Modification of xerantholide’s chemical structure may also open new possibilities in its use as an anti-cancer agent.
References
Bohlmann F, Borthakur N (1982) Sesquiterpenes and norsesquiterpenes from Pechuel-loeschea leibnitziae. Phytochemistry 21(5):1160–1162
Burke A (2000) Plant diversity of a man-made wetland–the Olushandja Dam in north central Namibia. Dinteria 26:25–44
Chinsembu KC (2015) Plants as antimalarial agents in Sub-Saharan Africa. Acta Trop 152:32–48
Chinsembu KC (2016) Green medicines: pharmacy of natural products for HIV and five AIDS-related infections. Canada, Africa in Canada Press, Toronto
Chinsembu KC (2016) Ethnobotanical study of plants used in the management of HIV/AIDS-related diseases in Livingstone, Southern Province, Zambia. Evid-Based Complement Altern Med. https://doi.org/10.1155/2016/4238625
Chinsembu KC (2016) Ethnobotanical study of medicinal flora utilized by traditional healers in the management of sexually transmitted infections in Sesheke District, Western Province, Zambia. Rev Bras Farmacogn 26:268–274
Chinsembu KC (2019) Chemical diversity and activity profiles of HIV-1 reverse transcriptase inhibitors from plants. Rev Bras Farmacogn. https://doi.org/10.1016/j.bjp.2018.10.006
Chinsembu KC, Hijarunguru A, Mbangu A (2015) Ethnomedicinal plants used by traditional healers in the management of HIV/AIDS opportunistic diseases in Rundu, Kavango East Region, Namibia. S Afr J Bot 100:33–42
Chinsembu KC, Syakalima M, Semenya SS (2019) Ethnomedicinal plants used by traditional healers in the management of HIV/AIDS opportunistic diseases in Lusaka, Zambia. S Afr J Bot 122:369–384
Curtis BA, Mannheimer CA (2005) Tree Atlas of Namibia. National Botanical Research Institute, Windhoek
Dekić MS, Radulović NS, Ranđelović VN, Stojanović-Radić ZZ, Veljković BP (2015) Essential oils and diethyl ether extracts of Serbian Xeranthemum cylindraceum and X. annum: chemical composition, antimicrobial activity, and chemotaxonomic implications. Chem Biodivers 12(9):1378–1397
Fadul E, Nizamani A, Rasheed S, Adhikari A, Yousuf S, Parveen S, Khalid A (2019) Anti-glycating and anti-oxidant compounds from traditionally used anti-diabetic plant Geigeria alata (DC) Oliv. & Hiern. Nat Prod Res. https://doi.org/10.1080/14786419.2018.1542388
Gasymova SA, Novruzov EN, Mekhtieva NP (2018) Chemical composition of fatty oil from Xeranthemum cylindraceum seeds. Chem Nat Compd 54(4):760–761
Holub M, Buděšínský M, Samek Z, Drożdż B, Grabarczyk H, Ulubelen A, Rychłewska U (1982) Absolute configuration of xerantholide, a sesquiterpenic lactone from Anthemis austriaca JACQ. Collect Czech Chem Commun 47(2):670–675
Ivanescu B, Miron A, Corciova A (2015) Sesquiterpene lactones from Artemisia genus: biological activities and methods of analysis. J Anal Methods Chem 247685:21. https://doi.org/10.1155/2015/247685
Kadhila NP (2018) Evaluation of indigenous Namibian mushrooms and plants for antimalarial properties. Dissertation, University of Namibia
Karpagasundari C, Kulothungan S (2014) Analysis of bioactive compounds in Physalis minima leaves using GC MS, HPLC, UV–VIS and FTIR techniques. J Pharmacog Phytochem 3:196–201
Kupchan SM, Fessler DC, Eakin MA, Giacobbe TJ (1970) Reactions of alpha methylene lactone tumor inhibitors with model biological nucelophiles. Science 168:376–380
Le Roux PJ, Müller MAN, Curtis B, Mannheimer C (2009) Le Roux and Müller’s field guide to the trees and shrubs of Namibia. Macmillan Education Namibia, Namibia
Makler MT, Ries JM, Williams JA, Bancroft JE, Piper RC, Gibbins BL, Hinrichs DJ (1993) Parasite lactate dehydrogenase as an assay for Plasmodium falciparum drug sensitivity. Am J Trop Med Hyg 48:739–741
Mumbengegwi DR, Du Preez IC, Dushimemaria F, Auala JR, Nafuka S (2015) The use of traditional medicinal plants as antimicrobial treatments. In: Chinsembu KC et al (eds) Indigenous Knowledge of Namibia. University of Namibia Press, Windhoek, pp 89–114
Nafuka S (2014) In vitro antiplasmodial activity and phytochemicals screening of ethnomedicinal plants used to treat malaria-associated symptoms. University of Namibia, Macmillan Education Namibia, Windhoek
Nawrot J, Bloszyk E, Harmatha JURA, Novotny L, Drozdz B (1986) Action of antifeedants of plant origin on beetles infesting stored products. Acta Entomol Bohemoslov 83:327–335
Ndongo D (2017) Antibacterial, antioxidant and phytochemical investigation of Acacia arenaria, Aloe esculenta and Pechuel-loeschea leubnitziae. Master’s Thesis, University of Namibia
Ríos E, León A, Chávez MI, Torres Y, Ramírez-Apan MT, Toscano RA, Delgado G (2014) Sesquiterpene lactones from Mikania micrantha and Mikania cordifolia and their cytotoxic and anti-inflammatory evaluation. Fitoterapia 94:155–163
Samek Z, Holub M, Drożdż B, Grabarczyk H, Hładoń B (1977) Xerantholide-A new cytotoxically active sesquiterpenic lactone from Xeranthemum cylindraceum SIBTH. et SMITH. Collect Czech Chem Commun 42(8):2441–2447
Schmidt T, Nour A, Khalid S, Kaiser M, Brun R (2009) Quantitative structure-antiprotozoal activity relationships of sesquiterpene lactones. Molecules 14:2062–2076
Tedder MJ, Kirkman KP, Morris CD, Trollope WSW, Bonyongo MC (2012) The influence of Pechuel-loeschea leubnitziae (wild sage) on grass sward and soil seed bank composition. Afr J Range Forage Sci 29:101–107
Theron MW, van Rooyen N, van Rooyen MW (1980) Vegetation of the lower Kuiseb River. Modoqua 11(4):327–345
Trager W, Jensen JB (1976) Human malaria parasites in continuous culture. Science 193(4254):673–675
Van Damme P, Van Den Eynden V, Vernemmen P (1922) Plant uses by the Topnaar of the Kuiseb Valley Namib desert. Afr Focus 8(3–4):223–252
Von Koenen E (2001) Medicinal, poisonous, and edible plants in Namibia. Klaus Hess Publishers, Windhoek
Vu H, Pedro L, Mak T, McCormick B, Rowley J, Liu M, Di Capua A et al (2018) Fragment-based screening of a natural product library against 62 potential malaria drug targets employing native mass spectrometry. ACS Infect Dis 4(4):431–444
Watson WH, Miski M, Mabry TJ (1987) The absolute configuration of an iodo derivative of xerantholide. Acta Crystallogr Sect C Cryst Struct Commun 43(11):2180–2182
Zimmermann S, Kaiser M, Brun R, Hamburger M, Adams M (2012) Cynaropicrin: the first plant natural product with in vivo activity against Trypanosoma brucei. Planta Med 78:553–556
Acknowledgements
We thank South Africa’s National Research Foundation (NRF), Namibia’s National Commission on Research Science and Technology (NCRST), Ministry of Higher Education, the Namibia Government Scholarship and Training Program (NGSTP), the University of Namibia (UNAM) for supporting the study and the Protechnik Laboratories for using their Instruments to analyse the data that allowed confirmation of the compound structure. The study was funded through the third call joint research collaboration grant from NRF/NCRST under the title “Screening of indigenous Namibian mushrooms for their antimalarial activities against sensitive and resistant strains of the malaria parasites”. Prof. K.C. Chinsembu and Dr. M. Sekhoacha were the co-principal investigators for the NRF/NCRST funded project.
Author information
Authors and Affiliations
Contributions
The study is part of the doctoral thesis of NPK; KCC was the main supervisor, MS and MT were the co-supervisors; and all the mentors revised the manuscript. KCC and MS conceptualized the study, wrote the original research proposal and received the financial grant to conduct this study. All the authors made important contributions in the accomplishment of the work, read the final manuscript and approved its submission.
Corresponding author
Ethics declarations
Conflicts of interest
The authors declare no conflicts of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Kadhila, N.P., Sekhoacha, M., Tselanyane, M. et al. Determination of the antiplasmodial activity, cytotoxicity and active compound of Pechuel-loeschea leubnitziae O. Hoffm. (Asteraceae) of Namibia. SN Appl. Sci. 2, 1328 (2020). https://doi.org/10.1007/s42452-020-2926-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s42452-020-2926-6