EXTRACT OF ORTHOSIPHON STAMINEUS, FORMULATIONS, AND USES THEREOF CROSS-REFERENCE TO RELATED APPLICATIONS
[0001] This application claims the benefit of Malaysian Patent Application No.
PI2017704167 filed November 2, 2017; Malasian Patent Application No. P2018702101 filed May 31, 2018; and U.S. Patent Application No. 62/723,637 filed August 28, 2018. BACKGROUND
[0002] Medicinal plants are the oldest known health care products. History reveals that all medical systems were once botanical based. The earliest written evidence of recipes utilizing plants for medicinal purposes can be found on 5,000-year-old Sumerian clay slabs in Nagpur, India, which documented 12 recipes for the preparation of compositions comprising well over 250 various plants, some of which include plants still in use today, such as henbane and poppy (1). The use of plants as medicines was not restricted, however, to certain civilizations or geographies. In c. 2500 B.C. China, Emperor Shen Nung documented the use of 365 drugs comprising dried parts of medicinal plants, in "Pen T'Sao", the Chinese compendium of medicinal plants. Plants, such as Rhei rhizoma, camphor, Theae folium,
Podophyllum, the great yellow gentian, ginseng, jimson weed, cinnamon bark, and ephedra, documented in the compendium, are still in use in traditional Chinese medicine (1), which has its own unique methods of diagnosis and treatment, and incorporates >7000 species of medicinal plants into clinical practice (2) (3). This is similarly true for Ayurvedic Medicine - one of the world's oldest medical systems originating in India almost 3,000 years ago, which incorporates the use of herbals and spices in its system of medicine. Ancient Egypt relied on the Ebers Papyrus, an Egyptian medical papyrus of herbal knowledge dating back to c.1550 B.C. The Ebers Papyrus is, to date, the most detailed record of ancient Egyptian medicine known and refers to about 700 plant species such as pomegranate, castor oil plant, aloe, senna, garlic, onion, fig, willow, coriander, juniper, and common centaury, for use as therapy in the treatment of a variety of ailments (1). In ancient Greece, Hippocrates catalogued the use of 300 medicinal plants by physiological function (1). In the United States, it is believed that the use of "conventional or Western medicine" began in c.1620 A.D., when the Pilgrims brought with them botanicals for use as food and medicines (3).
[0003] The reliance on natural products, such as botanicals, as sources of therapeutics has maintained its significance even in today's modern pharmaceutical industry. Plant based medicines continue to play a central role in the health care systems of many countries. This is particularly true in the developing countries, where the World Health Organization (WHO) estimates that about 80% of the population depends on medicinal plants as their primary and only affordable source of health care (3).
[0004] Over time, however, focus from the use of medicines comprising
multicomponent pharmacologically active molecules, such as plant derived medicines, shifted to mono-therapeutics. This was primarily due to the advent of organic chemistry and improved pharmaceutical manufacturing techniques at the turn of the 19th century, and the assumption that a single molecule in a plant, usually the molecule at the highest concentration, determined pharmacological activity. This assumption has been further
substantiated by the observation that single molecules purified from such plants allowed for thorough safety and careful dose assessments, which enhanced their therapeutic effectiveness. A comprehensive review of all drugs introduced into clinical practice shows that 73% of 155 anti-cancer drugs developed since the 1940s are natural compounds or derivatives thereof, and of the 877 small molecule drugs introduced between 1981 and 2002 almost 50% are either natural compounds or analogs thereof (4) (5). There are currently at least 120 single molecule compounds directly or indirectly derived from plants in use around the world (6). Examples of such molecules include morphine, scopolamine, codeine, digitoxin, quinine, galanthamine, taxol, emetine, atropine, forskolin, and artemisinin, to name a few.
[0005] Modern computational, combinatorial chemistry, and drug screening techniques, have provided the pharmaceutical industry with ways to discover new drug entities en mass that interact with single well defined molecular targets or pathways without knowingly interfering with other cellular functions at the beginning of the drug discovery process. It is hoped that this strategy would lead to druggable targets that are highly effective and safe with a low level of undesirable and potentially toxic side effects (7). While it is undeniable that this strategy has produced many successful therapies, there is growing concern over the observation that there has been a marked decline in the number of new drugs introduced into clinical practice over the past few decades. It is particularly concerning that these new drug candidates fail in late stages of clinical trials. Kola and Landis have studied the success rates for new single molecule drugs making it through development and final approval for a ten-year period from 1991-2000 by the European Medicines Agency (EMA) and/or the US Food and Drug Administration (FDA) (8). Their analysis shows that the average success rate for all therapeutic areas was only 11% (individual success rates for specific therapeutic areas varied - Arthritis and pain: ~16%, Cardiovascular: ~20%, CNS: ~8%, Infectious disease: ~16%, Oncology: ~5%, Ophthalmology: ~15%, Metabolic disease: ~11%, Urology: ~9%, and Women's health: ~4%).
[0006] One possible reason for this low success rate is the increasing realization that the etiology of many diseases is wide ranging and complex, and not caused by the dysregulation of a single molecular target or pathway (4) (7) (9) (10). Diseases such as cancer and chronic inflammation, for example, are the result of multiple events, which unfold over an extended period and demonstrate a wide range of pathophysiological manifestations. The highly selective nature of single molecule drugs may have unpredictable effects on other non-specific cellular pathways resulting in unexpected adverse events that are often only discovered in much larger patient populations during the later stages of clinical trials. Mono- compound therapies have the additional disadvantage of often acquiring resistance to the disease being treated over time due to built-in redundant cellular pathways or drug mitigating mechanisms that allow transformed cells or infectious microbes to become refractory to the therapy (11). Thus, while mono-therapeutics may be able to treat complex diseases such as cancer in the short term, by targeting a single well defined pathway, single molecule drugs do not always maintain their efficacy over the long term due to redundant mechanisms that eventually kick-in to compensate for loss or inactivation of the primary target. It has been proposed that treatment of complex multifactorial diseases, such as cancer, could benefit from a simultaneous attack, by a variety of pharmacologically active molecules within a multicomponent cocktail on their respective different molecular targets
(4) (7) (9) (10). Accordingly, there is a need for safe multicomponent therapeutics that can treat complex multifactorial diseases effectively.
[0007] Given the shortcomings of single molecular therapies, there is increasing interest in multi-target therapy to provide the needed "one-two punch" to treat complex multifactorial diseases. Plants are well suited for this purpose as they have evolved their own "immune system" by generating a wide variety of secondary metabolites to protect themselves against adverse environmental events, herbivores and pathogens (4).
Accordingly, suitable plant extracts, comprising a mixture of pharmaceutically active primary and secondary metabolites may function as effective multi-target therapy for the treatment of complex multifactorial diseases or physiological disorders. The most important classes of pharmaceutically active secondary metabolites, in plant extracts, include phytochemicals such as nitrogen containing compounds (e.g., alkaloids, cyanogenic glycosides, and glucosinolates), terpenoids and steroids (e.g., monoterpenes, sesquiterpenes, diterpenes, triterpenes, tetraterpenes, saponins and steroids), and the phenols, phenylpropanoids and polyketides (e.g., catechins, flavones, isoflavones, stilbenes, coumarins, lignans and polyketides) (5). While these compounds are present in extracts at low molar concentrations and individually have a weak impact on their respective cellular targets, in combination these phytochemicals act synergistically to promote a positive therapeutic outcome by simultaneously attacking a variety of cellular targets (4) (9). Multicomponent therapeutics, such as plant extracts, have an additional advantage - unlike mono-compound therapies, which have been specifically designed to target a single molecule or molecular pathway in a specific disease, a plant extract may be used to treat a variety of physiological disorders. This is because the diverse repertoire of primary and secondary metabolites present in plant extracts allow for the targeting of several molecules or cellular pathways shared between different disease states (12). Thus, there is a need for suitable plant derived therapeutics, such as plant extracts, comprising a therapeutically effective amount of a wide variety of phytochemicals for the treatment of complex diseases, providing such extracts also have an acceptable safety profile.
[0008] Orthosiphon stamineus Benth is a popular perennial medicinal herb grown and cultivated in Southeast Asian countries like Malaysia, Vietnam, China, Indonesia and Thailand (13). The leaves and stems are used for medicinal purposes and are harvested during the flowering season. In Malaysia, O. stamineus is locally known as Misai Kucing ("Cat's Whiskers"), Kumis Kucing or emujung in Indonesia, Yaa Nuat Maeo, Rau Meo or Cay Bac in Thailand, Moustaches de Chat in France and Java Tea and Kidney Tea in Europe (14) (15) (16) (17). The herb grows in temperate and tropical areas such as China, India,
Indonesia, Vietnam, Thailand, Malaysia, Australia, and the Pacific region.
[0009] In Southeast Asia, crude extracts of O. stamineus are widely-used as a traditional herbal tea. In Malaysia, the herb is used to treat arteriosclerosis and urinary system disorders such as, bladder inflammation, nephritis, kidney stones, and
hydronephrosis. It is also used as an antipyretic, diuretic, and for the treatment of rheumatism (18) (19). In addition, the tea prepared from O. stamineus leaves is also consumed to improve overall health and to treat gout, hypertension, diabetic edema, eruptive fever, influenza, hepatitis, and jaundice (20) (21). In Vietnam, the aerial part of O. stamineus known as "Raumeo" is used for treating urinary lithiasis, eruptive fever, influenza, edema, rheumatism, biliary lithiasis, hepatitis and jaundice (22). In Indonesia, tea steeped
with leaves of the plant are used to treat diabetes, hypertension, rheumatism, and as a diuretic. Crude extracts of the plant are also used for the treatment of a variety of angiogenesis-related diseases, including diabetic blindness and psoriasis. In Europe, O.
stamineus leaves are made into a tonic for the treatment of bladder ailments and kidney stones, urinary tract infections, liver and gallbladder problems. The crude extracts of the plant also lower cholesterol and blood pressure. In Myanmar, crude extracts of the leaves are used for treating diabetes, urinary tract and renal diseases. In Okinawa Prefecture, Japan, tea made from O. stamineus leaves is consumed to facilitate body detoxification (14).
[00010] O. stamineus is rich in pharmacologically active secondary metabolite phytochemicals comprising high amounts of flavones, polyphenols, bioactive proteins, glycosides, volatile oils, and vast quantities of potassium. These phytochemicals include, for example, polymethoxylated flavonoids (23), phenylpropanoids (caffeic acid derivatives) (22)
(24) , and terpenoids (diterpenes and triterpenes), as well as saponins, hexoses, organic acids
(25) . Other flavonoids isolated from O. stamineus leaves, include SIN, EUP, TMF, tetramethyl scutellarein (26) (27), salvigenin, ladanein, vomifoliol, 7,3,4-tri-O-methyl luteolin, and scutellarin tetramethyl-ether (23) (28) (29). Caffeic acid derivatives, such as A, caffeic acid, cichoric acid, and 2, 3-dicaffeoyltartaric have also been identified in extracts of O. stamineus (22) (24). Other compounds such as aldehyde, hydrocarbons, ketones, fatty acids, esters, and aromatic sesquiterpenes such as acetic acid (3-hydroxy-7-isopropenyl-l, 4a-dimethyl- octahydronaphthalen-2-yl) ester, dimethyl-4-(l-methylethylidene)-2,4,6,7,8,8a-hexahydro- 5(lH)-azulenone, anthracene, 9-(2-propenyl), 2-propen-l-one, 1,3-diphenyl, and 2-amino-2- oxo-acetic acid N-(3,4-dimethylphenyl) ethyl ester were identified in SC-CO2 extracts of the leaves of O. stamineus. Further investigation reported that more than 69 chemical compounds were detected in the essential oil of O. stamineus leaves. These include β- Elemene, l-Octen-3-ol, β-Carryophyllene, a-Humulene, β-Bourbene, Caryophyllene oxide, β- Pinene, Phenylacetaldehyde, Decanal, δ-Elemene, 1,8-Cineol, 4-Heptenal, Isomenthone, Camphene, cis-2-Octenal, 3-Octanol, Limonene, 2-Pentenyl furane, Hexanal, Naphtalene, Benzaldehyde, trans 2-Hexanal, Heptenal, trans cis-Octa-3-5- dien-2-one, Methyl Chavicol, a- Pinene, Tridecan, p-Cymene, Camphor, 1- Methylnaphtalene, a-Muniolene, trans trans-Octa- 3-5-dien-2-one, 2-Amylfurane, Menthone, Carvone, Cittonellol, δ-Cadipene, trans-2-(cis)-6- Nonadienale, Methyleugenol, a-Gubebene, Geranylacetane, δ-Terpineol, Acetophenone, trans- Anethol, Germacrene D, β-Cyclocitral, cis-Linalooloxide, Undecan, Bornyl Acetate, 2- Methylnapthalene, β-lonone, a-Copaene, Damascenone, Dehydroionone, Borneol,
Dodecane, Eugenol, Linalool, trans-Linalooloxide, Perillen, Safranal,
Hexahydrofamesylacetone, Hexan-l-ol,2,6,6-Trimethyl-2-cyclohexe-l,4-dione,
Isobornylacetate, trans-Deca-2,4-dienal, cis-Caryophylene, Germacrene, and cis-3-Hexen-l-o (30).
[0010] There is currently no standardized, pharmaceutical grade extract or
formulations comprising an extract of O. stamineus approved as a medicinal product. While crude extracts of O. stamineus have been used to treat a variety of ailments throughout South East Asia, Europe and the Pacific region, these extracts have not undergone rigorous scientific and clinical analysis. The rich and complex phytochemical profile of O. stamineus would satisfy it as a multicomponent pharmaceutical drug able to act on several cellular pathways, thus making the plant an effective source for a pharmaceutical drug product for the effective treatment of a variety of physiological disorders. Thus, there is a need for
standardized, effective, and safe pharmaceutical grade extracts and formulations comprising such extracts of O. stamineus leaves.
ABBREVIATIONS
[0011] Αβ: Amyloid beta; AE: Adverse event; AD: Alzheimer's Disease; ABC: ATP binding cassette; ABTS: 2,2'-azino-bis(3-ethylbenzothiazoline-6-sulphonic acid); BCRP: Breast cancer resistance protein; ACE: Angiotensin Converting Enzyme; AChE: Acetylcholinesterase; ALP: Alkaline phosphatase; ALT: Alanine aminotransferase; ALS: amyotrophic lateral sclerosis; AMD: Age Related Macular Degeneration; AST: aspartate aminotransferase; BSA: Bovine serum albumin; CA: Carbonic anhydrase; CAM: chick chorioallantoic membrane; CEA: Carcinoembryonic antigen; CCE: Countercurrent exchange; CCEe: Countercurrent exchange extract; CMC: carboxymethylcellulose; COX: Cyclooxygenase; COMT: Catechol-O- methyltransferase; DDW: Deuterium Depleted Water; DNA: Deoxyribonucleic acid; DEPC: diethyl pyrocarbonate; DLB: Dementia with Lewy Bodies; DMSO: dimethyl sulfoxide; DPP: Dipeptidyl peptidase; DPPH: l,l-diphenyl-2-picrylhydrazyl; DTNB: 5,5'-dithiobis-(2- nitrobenzoic acid); EC: ethylcellulose; ECM: Endothelial cell medium; ECGS: Endothelial cell growth supplements; EDTA: Ethylenediaminetetraacetic acid; EGF: Epidermal growth factor; EGFR: Epidermal growth factor receptor; EUP: Eupatorin; ELISA: Enzyme-linked
immunosorbent assay; EtOH: Ethanol; FBS: Fetal bovine serum; FBG : Fasting blood glucose; bFGF: b-Fibroblast growth factor; bFGFR: b-Fibroblast growth factor receptor; FMT:
fluorescence molecular tomography; FRAP: ferric reducing antioxidant power; FTIR: Fourier Transform Infrared Spectroscopy; GAPDH: Glyceraldehyde 3-phosphate dehydrogenase; GEM: Gemcitabine; GGT: Gamma-glutamyl transferase; GLUT: glucose transporter; G-CSF: Granulocyte-colony stimulating factor; GM-CSF: Granulocyte macrophage-colony stimulating factor; GM-CSFR: Granulocyte macrophage-stimulating factor receptor; GLP: Glucagon-like peptide; HEC: hydroxyethylcellulose; HIF: Hypoxia-Inducible Factor; HPC:
hydroxypropylcellulose; HEMA: hydroxyethyl methacrylic acid; HPLC: High performance liquid chromatography; HPMC: Hydroxypropylmethylcellulose; HMMA: hydroxymethyl methacrylic acid; HUVEC: Human Umbilical Vein Endothelial Cells; HMVEC-D: human dermal microvascular endothelial cells; HMVEC-L: human lung microvascular endothelial cells; HMVEC-C: human cardiac microvascular endothelial cells; HK1 and 2: hexokinase 1 and 2; IC5o: Half maximal inhibitory concentration; IL: Interleukin; IL-2R: lnterleukin-2 receptor; IL- 7R: lnterleukin-7 receptor; INF: Interferon; IFN-a: Interferon-a receptor; IFNAR: lnterferon-β receptor; l-TAC: Interferon-inducible T-cell alpha chemoattractant; KDR: Kinase Insert Domain Receptor; LDH: lactate dehydrogenase; MAO: Monoamine oxidase; MCP: Monocyte chemotactic protein; MCT: monocarboxylate transporter; MCTS: M ulticellular tumor spheroids; MDR: Multidrug resistance; MMP: Matrix metalopeptidase/metalloproteinase; MRP: Multidrug resistance protein; MS: Mass Spectroscopy; MTT: 3-(4,5-dimethylthiazol-2- yl)-2,5-diphenyltetrazolium bromide) tetrazolium; OS-W: Macerated O. stamineus leaves water extract; OS-E: Macerated O. stamineus leaves 100% EtOH extract; OS-M: Macerated O. stamineus leaves 100% methanol extract; OS-EW: Macerated O. stamineus leaves 1:1 (vol/vol) EtOH to water extract; OS-MW: Macerated O. stamineus leaves 1:1 (vol/vol) methanohwater extract; NO: Nitric oxide; NGF: Nerve Growth Factor; NGFR: Nerve growth factor receptor; NMR: Nuclear Magnetic Resonance; NSAID: Non-steroidal anti- inflammatory drug; PD: Parkinson's Disease; PS: Penicillin/streptomycin; PBS: Phosphate
buffered saline; PECAM: Platelet and endothelial cell adhesion molecule; PCR: Polymerase chain reaction; PDK: pyruvate dehydrogenase kinase; PEG: polyethylene glycol; PEO:
polyethylene oxide; PVP: polyvinylpyrrolidone; Pgp: P-glycoprotein; RA: osmarinic acid; RAAS: Renin-Angiotensin-Aldosterone System; RT: Room temperature; RNA: Ribonucleic acid; ROS: Reactive Oxygen Species; SIN: Sinensetin; SGLT: Sodium glucose linked transporter; STZ: Streptozotocin; TIE: Tyrosine kinase with immunoglobulin-like and EGF-like domains; TIMP: Tissue inhibitor of metalloproteinases; TGF: Transforming Growth Factor; TGF-aR: Transforming growth factor receptor; TLC: Thin Layer Chromatography; TMF: 3'- hydroxy-5,6,7,4'- tetramethoxyflavone; TNF: tumor necrosis factor; TZD: Thiazolidinedione; TNF R: tumor necrosis factor β receptor; TPTZ: 2,4,6-Tripyridyl-s-Triazine; TZD:
thiazolidinediones; uPAR: Urokinase plasminogen activator receptor; VEGF: Vascular Endothelium Growth Factor; VEGFR: Vascular Endothelium Growth Factor receptor; VCEAC: Vitamin-C equivalent antioxidant capacity; WNT: Wingless-related integration site. SUMMARY OF THE INVENTION
[0012] In one embodiment, the invention features a 1:1 (vol/vol) EtOH to water extract of O. stamineus leaves comprising <0.2% TMF. In one embodiment, the invention features a 1:1 (vol/vol) EtOH to water extract of O. stamineus leaves comprising <0.2% TMF. In another embodiment, invention features a 1:1 (vol/vol) EtOH to water extract of O. stamineus leaves comprising <0.1% TMF. In yet another embodiment, invention features a 1:1 (vol/vol) EtOH to water extract of O. stamineus leaves comprising <0.1% TMF. In one other embodiment, the invention features a 1:1 (vol/vol) EtOH to water extract of O. stamineus leaves comprising <14% (wt/wt) total protein (including free amino acids). The extract of the invention can treat a variety of physiological disorders. The extract of O. stamineus leaves described herein has, without limitation, an activity that is anti-angiogenic, antiinflammatory, antihypertensive, antihyperglycemic, antioxidant, anti-neurodegenerative, neuroprotective, anti-pyretic, anti-gout, anti-microbial, antilithiatic, anti-ulcerogenic, anti- asthenic, anti-cachexic, or any combination thereof.
[0013] Certain embodiments feature formulations comprising the extract of O.
stamineus leaves.
[0014] Certain embodiments provide for a method comprising, administering to a subject in need thereof an extract of O. stamineus leaves or a formulation comprising an extract of O. stamineus leaves in amount and for a time sufficient to induce a sustained improvement over baseline of an indicator that reflects the severity of a physiological disorder.
[0015] One embodiment comprises a method of manufacturing an extract of O.
stamineus leaves, the method comprising: (a) contacting pulverized leaves of O. stamineus with a solvent comprising 1:1 (vol/vol) EtOH to water solution preheated to 60°C, wherein the solvent is moving in a first direction for a period of time, (b) continuing the extraction by directing the solvent in a second direction opposite to the first direction for a period of time equal to the time in (a), (c) alternating direction of solvent flow for a period of time, (d) filtering the extract through a filter, and (e) concentrating the filtered extract by evaporation of the solvent. In certain embodiments, the total extraction time is 6hr. In certain embodiments, the extract is filtered through a ΙΟΟμιη filter. In certain embodiments, the filtered and concentrated extract can be further processed by spray drying the extract to
obtain a powder. In certain embodiments, the concentrated extract can be freeze dried to obtain a powder. In certain embodiments, the powder obtained by either spray drying or freeze drying can be subsequently formulated into an appropriate dosage form for administration in a subject in need thereof.
[0016] In one embodiment, the extract comprises phytochemicals. In one
embodiment, the phytochemicals are polysaccharides, glycosaponins, phenolics, flavonoids, phospholipids, proteins (including free amino acids), or any combination thereof. In certain embodiments, the polysaccharides can be present from 2% - 4% (wt/wt) (e.g 2, 2.1, 2.2, 2.3, 2.4, 2.5, 2.6, 2.7, 2.8, 2.9, 3, 3.1, 3.2, 3.3,3.4, 3.5, 3.6, 3.7, 3.8, 3.9 or 4%) of the total extract. In certain embodiments, the polysaccharides can be present from 2% - 3% (wt/wt) (e.g., 2.8, 2.9, 3, 3.1, or 3.2%) of the total extract. In certain other embodiments, the polysaccharides can be present at 3% (wt/wt) of the total extract. In certain embodiments, the glycosaponins can be present from 25% - 40% (wt/wt) (e.g., 25, 26, 27, 28, 29, 30, 31, 32, 33, 34, 35, 36, 37, 38, 39, 40, 41, 42, 43, 44, or 45%) of the total extract. In certain embodiments, the glycosaponins can be present from 28% - 36% (wt/wt) (e.g., 28, 28.5, 29, 29.5, 30, 30.5, 31, 31.5, 32, 32.5, 33, 33.5, 34, 34.5, 35, 35.5 or 36%) (wt/wt) of the total extract. In certain embodiments, the glycosaponins can be present at 32% (wt/wt) of the total extract. In certain embodiments, the phenolics comprising the extract can be present from 32% - 39% (wt/wt) (e.g 32, 32.5, 33, 33.5, 34, 34.5, 35, 35.5, 36, 36.5, 37, 37.5, 38, 38.5 or 39%) of the total extract. In certain embodiments, the phenolics can be present from 35% - 39% (wt/wt) (e.g., 35, 35.5, 36, 36.5, 37, 37.5, 38, 38.5 or 39%) of the total extract. In certain
embodiments, the phenolics can be present at 37% (wt/wt) of the total extract. In certain embodiments, the flavonoids can be present from 5% - 8% (wt/wt) (e.g., 5, 5.5, 6, 6.5, 7, 7.5 or 8%) of the total extract. In certain embodiments, the flavonoids can be present from 6% - 7% (wt/wt) (e.g., 6.1, 6.2, 6.3, 6.4, 6.5, 6.6, 6.7, 6.8, 6.9, or 7%) of the total extract. In certain embodiments, the flavonoids can be present at 6.6% of the total extract. In certain embodiments, the phospholipids comprising the extract can be present from 0.3% - 0.6% (wt/wt) (e.g., 0.3, 0.35, 0.4, 0.45, 0.5, 0.55, or 0.6%) of the total extract. In certain embodiments, the phospholipids can be present from 0.35% - 0.48% (wt/wt) (e.g., 0.35, 0.36, 0.37, 0.38, 0.39, 0.4, 0.41, 0.42, 0.43, 0.44, 0.45, 0.46, 0.47, or 0.48%) of the total extract. In certain embodiments, the phospholipids can be present at 0.44% (wt/wt) of the total extract. In certain embodiments, the total protein content (including free amino acids) in the extract can be present, by weight based on the total weight of the extract, <14% (e.g.,
0, 0.5, 1, 1.5, 2, 2.5, 3, 3.5, 4, 4.5, 5, 5.5, 6, 6.5, 7, 7.5, 8, 8.5, 9, 9.5, 10, 10.5, 11, 11.5, 12, 12.5, 13, 13.5, or 14%). In certain embodiments, the total protein content in the extract can be present <12.5% (wt/wt) (e.g., 0, 0.5, 1, 1.5, 2, 2.5, 3, 3.5, 4, 4.5, 5, 5.5, 6, 6.5, 7, 7.5, 8, 8.5, 9, 9.5, 10, 10.5, 11, 11.5, 12, or 12.5%) of the total extract. In certain embodiments, the total protein content can be present from 11.5% - 12.5% (wt/wt) (e.g., 11.5, 11.6, 11.7, 11.8, 11.9, 12, 12.1, 12.2, 12.3, 12.4 or 12.5%) of the total extract. In certain embodiments, the total protein content can be present at 12% (wt/wt) of the total extract. In certain other embodiments, the total protein content can be <12% (wt/wt) of the total extract (e.g., 0, 0.5,
1, 1.5, 2, 2.5, 3, 3.5, 4, 4.5, 5, 5.5, 6, 6.5, 7, 7.5, 8, 8.5, 9, 9.5, 10, 10.5, 11, 11.5, 11.6, 11.7, 11.8, or 11.9%).
[0017] In one embodiment, the phenolics comprises A, and the flavonoids comprises, EUP, SIN, and TMF.
[0018] In still another embodiment, the extract of O. stamineus leaves features a chemical fingerprint on high performance liquid chromatography substantially similar to that shown FIG. IB.
[0019] In at least one embodiment, the extract of the O. stamineus comprises, A, EUP, SIN, and optionally TMF.
[0020] In one aspect, the amount of TMF present in the extract, by weight based on the total weight of the extract, is <0.2% (e.g., 0, 0.01, 0.02, 0.03, 0.04, 0.05, 0.06, 0.07, 0.08, 0.09, 0.1, 0.12, 0.14, 0.16, 0.18, 0.19, or 0.2%). In one embodiment, such an extract is manufactured by a countercurrent exchange method.
[0021] In one aspect, the amount of TMF present in the extract, by weight based on the total weight of the extract, is <0.2% (e.g., 0, 0.01, 0.02, 0.03, 0.04, 0.05, 0.06, 0.07, 0.08, 0.09, 0.1, 0.12, 0.14, 0.16, 0.18, or 0.19%). In one embodiment, such an extract is manufactured by a countercurrent exchange method.
[0022] In one aspect, the extract of O. stamineus leaves comprises, by weight based on the total weight of the extract, <0.1% TMF, (e.g., 0, 0.01, 0.02, 0.03, 0.04, 0.05, 0.06, 0.07, 0.08, 0.09, 0.1%). In one embodiment, such an extract is manufactured by a countercurrent exchange method.
[0023] In one aspect, the extract of O. stamineus leaves comprises, by weight based on the total weight of the extract, <0.1% TMF, (e.g., 0, 0.01, 0.02, 0.03, 0.04, 0.05, 0.06, 0.07, 0.08, 0.09, or 0.095%). In one embodiment, such an extract is manufactured by a countercurrent exchange method.
[0024] In certain embodiments, RA is present in the extract of O. stamineus leaves, by weight based on the total weight of the extract, from 3% - 8% (e.g., 3, 3.5, 4, 4.5, 5, 5.5, 6, 6.5, 7, 7.5, or 8%). In certain embodiments, the RA is present in the extract of O. stamineus leaves, by weight based on the total weight of the extract, from 4% - 7% (e.g., 4, 4.5, 5, 5.5, 6, 6.5, or 7%).
[0025] In certain embodiments, the extract of O. stamineus leaves comprises, by weight based on the total weight of the extract, 6% ± 1.2% RA, i.e., from 4.8% - 7.2% (e.g., 4.8, 5, 5.2, 5.4, 5.6, 5.8, 6, 6.2, 6.4, 6.6, 6.8, 7, or 7.2%).
[0026] In certain embodiments, the extract of O. stamineus leaves comprises, by weight based on the total weight of the extract, 6% ± 1.2% RA, i.e., from 4.8% - 7.2% (e.g., 4.8, 5, 5.2, 5.4, 5.6, 5.8, 6, 6.2, 6.4, 6.6, 6.8, 7, or 7.2%) and comprises, by weight based on the total weight of the extract, <0.2% (e.g., 0, 0.01, 0.02, 0.03, 0.04, 0.05, 0.06, 0.07, 0.08, 0.09, 0.1, 0.12, 0.14, 0.16, 0.18, 0.19, or 0.2%) TMF. In one embodiment, such an extract is manufactured by a countercurrent exchange method.
[0027] In certain embodiments, the extract of O. stamineus leaves comprises, by weight based on the total weight of the extract, 6% ± 1.2% RA, i.e., from 4.8% - 7.2% (e.g., 4.8, 5, 5.2, 5.4, 5.6, 5.8, 6, 6.2, 6.4, 6.6, 6.8, 7, or 7.2%) and comprises, by weight based on the total weight of the extract, <0.2% (e.g., 0, 0.01, 0.02, 0.03, 0.04, 0.05, 0.06, 0.07, 0.08, 0.09, 0.1, 0.12, 0.14, 0.16, 0.18, or 0.19%) TMF. In one embodiment, such an extract is manufactured by a countercurrent exchange method.
[0028] In certain embodiments, the extract of O. stamineus leaves comprises, by weight based on the total weight of the extract, 6% ± 1.2% RA, i.e., from 4.8% - 7.2% (e.g., 4.8, 5, 5.2, 5.4, 5.6, 5.8, 6, 6.2, 6.4, 6.6, 6.8, 7, or 7.2%) and comprises, by weight based on the total weight of the extract, <0.1% (e.g., 0, 0.01, 0.02, 0.03, 0.04, 0.05, 0.06, 0.07, 0.08,
0.09, or 0.1%) TMF. In one embodiment, such an extract is manufactured by a
countercurrent exchange method.
[0029] In certain embodiments, the extract of O. stamineus leaves comprises, by weight based on the total weight of the extract, 6% ± 1.2% A, i.e., from 4.8% - 7.2% (e.g., 4.8, 5, 5.2, 5.4, 5.6, 5.8, 6, 6.2, 6.4, 6.6, 6.8, 7, or 7.2%) and comprises, by weight based on the total weight of the extract, <0.1% (e.g., 0, 0.01, 0.02, 0.03, 0.04, 0.05, 0.06, 0.07, 0.08, 0.09, or 0.095%) TM F. In one embodiment, such an extract is manufactured by a countercurrent exchange method.
[0030] In certain embodiments, SIN is present, by weight based on the total weight of the extract of O. stamineus leaves, at no more than 0.5% (e.g., 0.01, 0.02, 0.03, 0.04, 0.05, 0.1, 0.15, 0.2, 0.25, 0.3, 0.35, 0.4, 0.45 or 0.5%). In certain embodiments, SIN is present, by weight based on the total weight of the extract of O. stamineus leaves from 0.05% - 0.5% (e.g., 0.05, 0.1, 0.15, 0.2, 0.25, 0.3, 0.35, 0.4, 0.45 or 0.5%).
[0031] In certain embodiments, EUP is present, by weight based on the total weight of the extract of O. stamineus leaves, from 0.05% - 0.5% (e.g., 0.05, 0.1, 0.15, 0.2, 0.25, 0.3, 0.35, 0.4, 0.45 or 0.5%).
[0032] In certain embodiments, the extract of O. stamineus leaves comprises 6% RA, 0.15% EUP, not more than 0.5% SIN, and is <0.2% TMF. In one embodiment, such an extract is manufactured by a countercurrent exchange method.
[0033] In certain embodiments, the extract of O. stamineus leaves comprises 6% RA, 0.15% EUP, not more than 0.5% SIN, and is <0.2% TMF. In one embodiment, such an extract is manufactured by a countercurrent exchange method.
[0034] In certain embodiments, the extract of O. stamineus leaves comprises 6% RA, 0.15% EUP, not more than 0.5% SIN, and is <0.1% TMF. In one embodiment, such an extract is manufactured by a countercurrent exchange method.
[0035] In certain embodiments, the extract of O. stamineus leaves comprises 6% RA, 0.15% EUP, not more than 0.5% SIN, and is <0.1% TMF. In one embodiment, such an extract is manufactured by a countercurrent exchange method.
[0036] In certain embodiments, TMF in the extract of O. stamineus leaves is not detectable by UV using HPLC at 310 - 340 nm. In certain embodiments, TM F in the extract of O. stamineus leaves is not detectable by UV using HPLC at 320 nm.
[0037] In certain embodiments, the extract of O. stamineus leaves can have, by weight based on the total weight of the extract, <14% total protein (including free amino acids).
[0038] In one embodiment, the extract of O. stamineus leaves is manufactured by a countercurrent exchange method.
[0039] In certain embodiments, the extract of O. stamineus leaves is manufactured by a countercurrent exchange method and comprises, by weight based on the total weight of the extract, <0.2% TM F.
[0040] In certain embodiments, the extract of O. stamineus leaves is manufactured by a countercurrent exchange method and comprises, by weight based on the total weight of the extract, <0.1% TM F.
[0041] In certain embodiments, the extract of O. stamineus leaves is manufactured by a countercurrent exchange method and comprises, by weight based on the total weight of the extract, <0.1% TM F.
[0042] In certain embodiments, the extract of O. stamineus leaves is manufactured by a countercurrent exchange and comprises total protein at <14% (wt/wt) of the total extract.
[0043] In one embodiment, the extract of O. stamineus leaves or formulations comprising the extract of O. stamineus leaves, comprises an activity that is anti-angiogenic, anti-inflammatory, antihypertensive, antihyperglycemic, antioxidant, anti- neurodegenerative, neuroprotective, anti-pyretic, anti-gout, anti-microbial, anti-renal lithiasis, anti-ulcerogenic, anti-asthenic, anti-cachexic or any combination thereof.
[0044] One embodiment features a method of treating or ameliorating a preexisting physiological disorder in a subject in need thereof, said method comprising, administering to the subject a therapeutically effective amount of the extract of O. stamineus leaves or a formulation comprising a therapeutically effective amount of the extract of O. stamineus leaves. In one embodiment, the pre-existing physiological disorder is a dermal disorder, neurological disorder, angiogenesis associated disorder, an inflammatory related disorder, inflammation, asthenia, cachexia, hyperglycaemia, hypertension, lithiasis, gout, fever, microbial infection, stomach ulcers, kidney disease, liver diseases, or any combination thereof.
[0045] Another embodiment provides for a method of preventing a physiological disorder in a subject predisposed to said physiological disorder, said method comprising, administering to the subject a therapeutically effective amount of an extract of O. stamineus leaves or a formulation comprising a therapeutically effective amount of an extract of the O. stamineus leaves. In one embodiment, the physiological disorder is a dermal disorder, neurological disorder, angiogenesis associated disorder, an inflammatory related disorder, inflammation, asthenia, cachexia, hyperglycaemia, hypertension, lithiasis, gout, fever, microbial infection, stomach ulcers, kidney disease, liver diseases, or any combination thereof.
[0046] One embodiment features the use of the extract of O. stamineus leaves for the manufacture of a medicament for the treatment, amelioration, or prevention of a a dermal disorder, neurological disorder, an angiogenesis associated disorder, an inflammatory related disorder, inflammation, asthenia, cachexia, hyperglycaemia, hypertension, lithiasis, gout fever, microbial infection, stomach ulcers, kidney disease, liver diseases, or any combination thereof.
[0047] One embodiment features the use of a therapeutically effective amount of the extract of O. stamineus leaves or a formulation comprising a therapeutically effective amount of the extract of O. stamineus leaves for the treatment, amelioration or prevention of a dermal disorder, neurological disorder, an angiogenesis associated disorder, an inflammatory related disorder, inflammation, asthenia, cachexia, hyperglycaemia, hypertension, lithiasis, gout fever, microbial infection, stomach ulcers, kidney disease, liver diseases, or any combination thereof.
[0048] In one embodiment, the extract of O. stamineus leaves comprises anti- angiogenic activity.
[0049] In one embodiment, the extract of O. stamineus leaves can inhibit the proliferation and/or migration of endothelial cells.
[0050] In one embodiment, the extract of O. stamineus leaves can inhibit the invasiveness of cancer cells.
[0051] In one embodiment, the extract of O. stamineus leaves can inhibit capillary tube formation.
[0052] In one embodiment, the extract of O. stamineus leaves can inhibit
neovascularization.
[0053] In one embodiment, the extract of O. stamineus leaves can promote vascular normalization.
[0054] In one embodiment, the extract of O. stamineus leaves can inhibit aggregation of cancer cells to form solid tumors.
[0055] In one embodiment, the extract of O. stamineus leaves can inhibit the growth of a tumor. In one embodiment, the tumor is any tumor beyond 2 mm in diameter, melanomas, blastomas, lymphomas, carcinomas, sarcomas, leukemias, or any combination thereof.
[0056] In one embodiment, the extract of O. stamineus leaves can inhibit further growth of tumors in a tumor bearing subject.
[0057] In one embodiment, the extract of O. stamineus leaves can retard the progression of cancer in a subject diagnosed with cancer.
[0058] In one embodiment, the extract of O. stamineus leaves provides continued survival of a subject bearing a tumor(s).
[0059] One embodiment provides for a method of inhibiting or downregulating angiogenesis in a subject in need thereof, said method comprising, administering to the subject a therapeutically effective amount of the extract of O. stamineus leaves or a formulation comprising a therapeutically effective amount of the extract of O. stamineus leaves for modulating the expression and/or activity of a factor or plurality of factors which inhibit or downregulate angiogenesis.
[0060] One embodiment provides for a method of treating an angiogenesis associated disorder in a subject in need thereof, said method comprising, administering to the subject a therapeutically effective amount of the extract of O. stamineus leaves or a formulation comprising a therapeutically effective amount of the extract of O. stamineus leaves.
[0061] In one embodiment, the extract of O. stamineus leaves or formulations comprising the extract of O. stamineus leaves can modulate expression and/or activity of a factor or a plurality of factors which inhibit or downregulate angiogenesis, i.e., the extract has an overall anti-angiogenic activity. In one embodiment, the factor or plurality of factors is/are pro-angiogenic factors, anti-angiogenic factors, cytokines, or any combination thereof. In one embodiment, the cytokine is a chemokine, interleukin, interferon, lymphokine, tumor necrosis factor, or any combination thereof.
[0062] In one embodiment, an extract of O. stamineus leaves can modulate expression of pro- and anti-apoptotic factors such that the extract has an antiangiogenic activity.
[0063] In one embodiment, an extract of O. stamineus leaves can modulate the expression of transcription factors that have been shown to play a role in carcinogenesis, such that the extract has an antiangiogenic activity.
[0064] In certain embodiments, the extract of O. stamineus leaves can downregulate the expression and/or activity of a factor or plurality of factors that promote angiogenesis. In one such embodiment, the factor or plurality of factors is/are pro-angiogenic factors, cytokines, growth factors, hormones, or any combination thereof. In one embodiment, the
cytokines that have pro-angiogenic activity is a chemokine, interleukin, interferon, lymphokine, tumor necrosis factor, or any combination thereof.
[0065] In one embodiment, the extract of O. stamineus leaves can downregulate the expression and/or activity of a receptor for a pro-angiogenic factor. In certain such embodiments, the receptor for the pro-angiogenic factor is a receptor for a growth factor, hormone, chemokine, interleukin, interferon, lymphokine, tumor necrosis factor, or any combination thereof.
[0066] In certain embodiments, the extract of O. stamineus leaves can up-regulate expression and/or activity of a factor or plurality of factors that inhibit angiogenesis. In one embodiment, the extract of O. stamineus leaves can up-regulate expression and/or activity of a factor or plurality of factors having anti-angiogenic activity. In certain embodiments, the factor or plurality of factors having anti-angiogenic activity is/are chemokines, interleukins, interferons, lymphokines, tumor necrosis factor, or any combination thereof.
[0067] In one embodiment, the extract of the O. stamineus leaves can up-regulate the expression and/or activity of a receptor for an anti-angiogenic factor. In certain such embodiments, the receptor for the anti-angiogenic factor is a growth factor receptor, a hormone receptor, a chemokine receptor, an interleukin receptor, an interferon receptor, a lymphokine receptor, a tumor necrosis factor receptor, or any combination thereof.
[0068] In one embodiment, the extract of O. stamineus leaves or formulations comprising the extract of O. stamineus leaves can inhibit or downregulate expression and/or activity of VEGF, EGF, bFGF, TGF-ot, NGF , TNF-β, IL-2, IL-7, or any combination thereof. In certain embodiments, the VEGF, EGF, bFGF, TGF-ot, NGF , TNF-β, IL-2, IL-7, or any combination thereof, has pro-angiogenic activity.
[0069] In one embodiment, the extract of O. stamineus leaves or formulations comprising the extract of O. stamineus leaves, can inhibit or downregulate the expression and/or activity of a receptor for VEGF, EGF, FGF, TGFot, NGF, IL-2, IL-7, TNF-β, or any combination thereof. In one embodiment, the inhibition or down-regulation of a receptor for VEGF, EGF, FGF, TGFot, NGF, IL-2, IL-7, TNF-β, or any combination thereof, by the extract of O. stamineus or a formulation comprising the extract of the O. stamineus leaves results in anti-angiogenesis.
[0070] One embodiment features a method of treating an angiogenesis associated disorder in a subject in need thereof, said method comprising administering to the subject a therapeutically effective amount of the extract of O. stamineus leaves or formulations comprising a therapeutically effective amount of the extract of O. stamineus leaves for treating the angiogenesis associated disorder by downregulating the expression and/or activity of VEGF, EGF, bFGF, TGF-ot, NGF, IL-2, IL-7, TNF-β, or any combination thereof.
[0071] One embodiment features a method of treating an angiogenesis associated disorder in a subject in need thereof, said method comprising, administering to the subject a therapeutically effective amount of the extract of O. stamineus leaves or a formulation comprising a therapeutically effective amount of the extract of O. stamineus leaves for treating the angiogenesis associated disorder by downregulating the expression and/or activity of a receptor for VEGF, EGF, bFGF, TGFot, NGF, IL-2, IL-7, ΤΝΡβ, or any combination thereof.
[0072] In one embodiment, the extract of O. stamineus leaves can up-regulate the activity of GM-CSF, IFN-a, IFN-β, or any combination thereof. In certain embodiments, GM- CSF, IFN-a, IFN-β, or any combination thereof has anti-angiogenic activity.
[0073] One embodiment features a method of treating an angiogenesis associated disorder in a subject in need thereof, said method comprising, administering to the subject a therapeutically effective amount of the extract of O. stamineus leaves or formulations comprising a therapeutically effective amount of the extract of O. stamineus leaves for the treatment of the angiogenesis associated disorder by up-regulating the expression and/or activity of GM-CSF, IFN-a, IFN-β, or any combination thereof for treating the angiogenesis associated disorder.
[0074] One embodiment features a method of treating an angiogenesis associated disorder in a subject in need thereof, said method comprising, administering to the subject a therapeutically effective amount of the extract of O. stamineus leaves or a formulation comprising a therapeutically effective amount of the extract of O. stamineus leaves for the treatment of an angiogenesis associated disorder by up-regulating the expression and/or activity of a receptor for GM-CSF (CD116), IFN-a, IFN-β, or any combination thereof. In certain embodiments, the activation of a receptor for GM-CSF (CD116), IFN-a, IFN-β, or any combination thereof results in anti-angiogenic activity.
[0075] In one embodiment, the extract of O. stamineus leaves can downregulate the expression of genes HIF-la, WNT, KDR, COX2, or any combination thereof.
[0076] One embodiment features a method of treating a tumorigenic disease in a subject in need thereof, said method comprising, administering to the subject a
therapeutically effective amount of the extract of O. stamineus leaves or a formulation comprising a therapeutically effective amount of the extract of O. stamineus leaves for the treatment of the tumorigenic disease by downregulating the expression of genes HIF-la, WNT, KDR, COX2, or any combination thereof.
[0077] In one embodiment, the angiogenesis associated disorder is a tumorigenic disease, non-tumorigenic disease, or any combination thereof.
[0078] In one embodiment, the tumorigenic disease can be benign or malignant. In one embodiment, the tumorigenic disease is any solid tumor, blood-borne cancer, or any combination thereof.
[0079] In one embodiment, the solid tumor is any tumor beyond 2mm in diameter.
[0080] In one embodiment, the solid tumor is a melanoma, sarcoma, adenocarcinoma, lymphoma, blastoma, skin tumor, brain tumor, or any combination thereof.
[0081] In one embodiment, the non-tumorigenic disease is a disease of the eye involving a retinal vascular component, diabetic retinopathy, retinopathy of prematurity, proliferative sickle cell retinopathy, proliferative diabetic retinopathy, retinal ischemia, proliferative vitreoretinopathy, corneal graft rejection, neovascular glaucoma, epidemic keratoconjunctivitis, atopic keratitis, superior limbic keratitis , pterygium, Sjogren's syndrome, acne rosacea, phylectenulosis, syphilis, mycobacterial infections, infectious diseases wherein pathogens express angiogenic factors, infectious diseases wherein pathogens induce angiogenic programs, infectious diseases wherein pathogens transform endothelial cells, lipid degeneration, gastrointestinal ulcers, Herpes simplex infections, Herpes zoster infections, protozoan infections, Kaposi's sarcoma, chemical burns, Mooren's ulcer, Terrien's marginal degeneration, marginal keratolysis, trauma, osteoarthritis,
inflammatory arthritis, synovitis, systemic lupus, polyarteritis nodosa, Wegener's sarcoidosis, Stevens-Johnson disease, macular degeneration, Exudative and Nonexudative (Dry) Age- related Macular Degeneration (AMD), Stargardt's disease, sickle cell anemia, interstitial lung diseases, sarcoidosis, idiopathic interstitial pneumonias, corneal neovascularization, trachoma, pseudoxanthoma elasticum, Paget's disease of the vulva and breast, Paget's disease of the bone, retinal vein occlusion, chronic uveitis, chronic vitritis, Lyme's disease, Eales' disease, Behcet's disease, diseases related to choroidal neovascularization, inflammatory bowel disease, Crohn's disease, ulcerative colitis, asthma, arterial or venous malformations, vascular dysmorphogenesis, DiGeorge Syndrome, hereditary hemorrhagic telangiectasia, hemangiomas, obesity, cataracts, inflammatory skin diseases, psoriasis, dermatitis, warts, blistering disease, periodontal disease, peritoneal adhesions,
endometriosis, ocular neovascular disease, dysfunctional uterine bleeding, ovarian hyperstimulation syndrome, polycystic ovary syndrome, myometrial fibroids, adenomyosis, diabetes, atherosclerosis, Bartonellosis, angiogenesis of the endocrine glands, primary hyperparathyroidism, secondary hyperparathyroidism, tertiary hyperparathyroidism, pyogenic granulomas, keloids, acoustin neuroma, and pulmonary hypertension, pars planitis, chronic retinal detachment, hyperviscosity syndromes, post-laser complications, abnormal proliferation of fibrovascular or fibrous tissue, infections causing retinitis or choroiditis, presumed ocular histoplasmosis, Best's disease, diseases associated with rubeosis
(neovascularization of the angle), asthenia, cachexia, or any combination thereof.
[0082] In certain embodiments, the extract of O. stamineus leaves or a formulation comprising the extract of O. stamineus leaves can be administered in combination with a therapeutically effective amount of another therapeutic agent for the treatment of angiogenesis associated disorders. In one embodiment, the other therapeutic agent for the treatment of the angiogenesis associated disorder can be a standard therapeutic agent for the treatment of an angiogenesis associated disorder.
[0083] One embodiment provides for a method of decreasing the size of an existing capillary network in a subject in need thereof, wherein the growth and maintenance of the network depends on angiogenesis, said method comprising, administering to the subject a therapeutically effective amount of the extract of O. stamineus leaves or a formulation comprising a therapeutically effective amount of the extract of O. stamineus leaves for decreasing the size of an existing capillary network the growth and maintenance of which is dependent on angiogenesis.
[0084] In one embodiment, the extract of O. stamineus leaves can promote vascular normalization for the treatment of angiogenesis-associated disorders.
[0085] One embodiment provides for a method of treating an angiogenesis associated disorder by promoting vascular normalization in a subject in need thereof, said method comprising, administering to the subject a therapeutically effective amount of the extract of O. stamineus leaves or a formulation comprising a therapeutically effective amount of the extract of O. stamineus leaves.
[0086] In one embodiment, the capillary network is associated with a physiological disorder.
[0087] In one embodiment, the capillary network is associated with a tumorigenic disease, a non-tumorigenic disease, or any combination thereof.
[0088] In one embodiment, the capillary network is associated with corneal neovascularization.
[0089] One embodiment features a method of inhibiting or slowing corneal neovascularization in a subject in need thereof, said method comprising, administering to the subject a therapeutically effective amount of the extract of the O. stamineus leaves or a formulation comprising a therapeutically effective amount of the extract of the O. stamineus leaves.
[0090] In one embodiment, the capillary network is associated with retinal neovascularization.
[0091] One embodiment features a method of inhibiting or slowing retinal neovascularization in a subject in need thereof, said method comprising, administering to the subject a therapeutically effective amount of the extract of the O. stamineus leaves or a formulation comprising a therapeutically effective amount of the extract of the O. stamineus leaves.
[0092] One embodiment provides for a method of treating a retinopathy in a subject in need thereof, said method comprising, administering the subject a therapeutically effective amount of the extract of O. stamineus leaves or a formulation comprising a therapeutically effective amount of the extract of O. stamineus leaves.
[0093] One embodiment provides for a method of treating diabetic retinopathy in a subject in need thereof, said method comprising, administering the subject a therapeutically effective amount of the extract of O. stamineus leaves or a formulation comprising a therapeutically effective amount of the extract of O. stamineus leaves.
[0094] One embodiment provides for a method of treating retinal ischemia in a subject in need thereof, said method comprising, administering the subject a therapeutically effective amount of the extract of O. stamineus leaves or a formulation comprising a therapeutically effective amount of the extract of O. stamineus leaves.
[0095] In one embodiment, the extract of O. stamineus leaves can promote vascular normalization for the treatment of diabetic retinopathy.
[0096] In one embodiment, the extract of O. stamineus leaves can promote vascular normalization for the treatment of AMD.
[0097] In one embodiment, the capillary network is associated with adipose fat tissue.
[0098] In one embodiment, the capillary network is associated with adipose fat tissue wherein decreasing the capillary network decreases or inhibits the growth of the adipose fat tissue.
[0099] One embodiment, features a method of lowering blood glucose in a subject in need thereof, said method comprising, administering to the subject a therapeutically effective amount of the extract of O. stamineus leaves or a formulation comprising a therapeutically effective amount of the extract of O. stamineus leaves for lowering blood glucose.
[0100] One embodiment features a method of treating a subject diagnosed with diabetes, obesity, hyperglycemia, or any combination thereof, said method comprising, administering to the subject a therapeutically effective amount of the extract of O.
stamineus leaves or a formulation comprising a therapeutically effective amount of the extract of O. stamineus leaves for the treatment of diabetes, obesity, hyperglycemia, or any combination thereof.
[0101] One embodiment provides for a method of maintaining a healthy blood glucose level in a subject in need thereof, said method comprising, administering to the subject a therapeutically effective amount of the extract of O. stamineus leaves or a formulation comprising a therapeutically effective amount of the extract of O. stamineus leaves for maintaining a healthy blood glucose level.
[0102] One embodiment, features a method of lowering blood glucose in a subject in need thereof, said method comprising, administering to the subject a therapeutically effective amount of the extract of O. stamineus leaves or a formulation comprising a therapeutically effective amount of the extract of O. stamineus leaves in combination with a therapeutically effective amount of another active agent for lowering blood glucose. In one embodiment, the other therapeutic agent for lowering blood glucose can be a standard therapeutic agent for the use of lowering blood glucose.
[0103] In one embodiment, the capillary network is associated with a tumor.
[0104] One embodiment features a method of inhibiting or slowing the growth of a preexisting tumor in a subject in need thereof, said method comprising, administering to the subject a therapeutically effective amount of the extract of O. stamineus leaves or a formulation comprising a therapeutically effective amount of the extract of O. stamineus leaves for inhibiting or slowing the growth of the preexisting tumor.
[0105] One embodiment provides for a method of promoting the progression free cancer survival of a subject diagnosed with the cancer, said method comprising, administering to the subject a therapeutically effective amount of the extract of O.
stamineus leaves or a formulation comprising a therapeutically effective amount of the extract of O. stamineus leaves for the progression free cancer survival of the subject.
[0106] In one embodiment, the extract of O. stamineus leaves can reduce multidrug resistance.
[0107] One embodiment features a method for reducing multidrug resistance in a subject in need thereof, said method comprising, administering to the subject a
therapeutically effective amount of the extract of O. stamineus leaves or a formulation comprising a therapeutically effective amount of the extract of O. stamineus leaves for reducing multidrug resistance.
[0108] One embodiment provides for a method of treating an angiogenesis associated disorder in a subject in need thereof, said method comprising, administering to the subject a therapeutically effective amount of the extract of O. stamineus leaves or a formulation comprising a therapeutically effective amount of the extract of O. stamineus leaves for reducing multidrug resistance in the treatment of the angiogenesis associated disorder.
[0109] One embodiment provides for a method of enhancing the sensitivity of a tumor to a chemotherapeutic agent in a subject undergoing chemotherapy, said method comprising, administering to the subject a therapeutically effective amount of the extract of O. stamineus leaves or a formulation comprising a therapeutically effective amount of the extract of O. stamineus leaves prior to and/or during chemotherapy or in combination with standard therapy for enhancing the sensitivity of the tumor to the chemotherapeutic or standard therapeutic agent.
[0110] One embodiment provides for a method of treating an angiogenesis associated disorder in a subject in need of such treatment, said method comprising, administering to the subject a therapeutically effective amount of the extract of O. stamineus leaves or a
formulation comprising a therapeutically effective amount of the extract of O. stamineus leaves as a neoadjuvant for the treatment of the angiogenesis associated disorder.
[0111] One embodiment provides for a method of treating an angiogenesis associated disorder in a subject in need thereof, said method comprising, administering to the subject a therapeutically effective amount of the extract of O. stamineus leaves or a formulation comprising a therapeutically effective amount of the extract of O. stamineus leaves for treating the angiogenesis associated disorder by inhibiting or downregulating the expression and/or activity of CA9.
[0112] In one embodiment, a method is provided for the treatment of an angiogenesis associated disorder in a subject in need thereof, said method comprising administering to the subject a therapeutically effective amount of the extract of O. stamineus leaves or a formulation comprising the extract of O. stamineus leaves as an adjuvant for the treatment of the angiogenesis associated disorder.
[0113] In one embodiment, the extract of the O. stamineus leaves or formulations comprising the extract of the O. stamineus leaves can inhibit or downregulate the expression and/or activity of CA9.
[0114] In one embodiment, the extract of O. stamineus leaves comprises antiinflammatory activity.
[0115] One embodiment provides for a method of treating inflammation or an inflammatory related disorder in a subject in need thereof, said method comprising, administering to the subject a therapeutically effective amount of the extract of O.
stamineus leaves or a formulation comprising a therapeutically effective amount of the extract of O. stamineus leaves for the treatment of inflammation or an inflammatory related disorder.
[0116] One embodiment provides for a method of inhibiting or downregulating the activity of a proinflammatory factor or plurality of proinflammatory factors, in a subject in need thereof, said method comprising, administering to the subject a therapeutically effective amount of the extract of the O. stamineus leaves or a formulation comprising a therapeutically effective amount of the extract of the O. stamineus leaves for inhibiting or downregulating the activity and/or expression of the proinflammatory factor or plurality of proinflammatory factors.
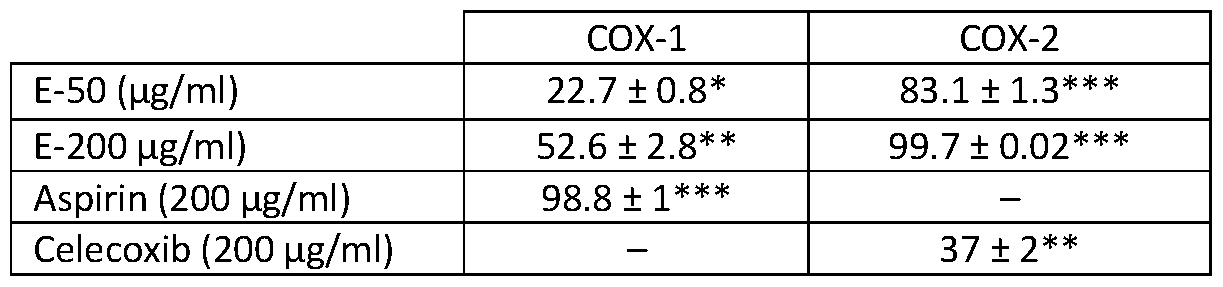
[0117] One embodiment provides for a method of inhibiting or downregulating the activity of IL-1, IL-6, IL-8, TNF-a, COX-1, COX-2, or any combination thereof , in a subject in need thereof, said method comprising, administering to the subject a therapeutically effective amount of the extract of the O. stamineus leaves or a formulation comprising a therapeutically effective amount of the extract of the O. stamineus leaves for inhibiting or downregulating the activity and/or expression of IL-1, IL-6, IL-8, TNF-a, COX-1, COX-2, or any combination thereof. In certain embodiments, IL-1, IL-6, IL-8, TNF-a, COX-1, COX-2, or any combination thereof has proinflammatory activity.
[0118] One embodiment provides for a method of inhibiting or downregulating the expression and/or activity of a receptor for a proinflammatory factor, said method comprising, administering to the subject a therapeutically effective amount of the extract of O. stamineus leaves or a formulation comprising a therapeutically effective amount of the extract of O. stamineus leaves for inhibiting or downregulating the expression and/or activity of the receptor for the proinflammatory factor.
[0119] One embodiment provides for a method of inhibiting or downregulating the activity of of a receptor for IL-1, IL-6 (CD126), IL-8 (CXC 1), TNF-a, or any combination thereof, in a subject in need thereof, said method comprising, administering to the subject a therapeutically effective amount of the extract of the O. stamineus leaves or a formulation comprising a therapeutically effective amount of the extract of the O. stamineus for downregulating the expression and/or activity of IL-1, IL-6 (CD126), IL-8 (CXCR1), TNF-a, or any combination thereof.
[0120] One embodiment provides for the treatment of inflammation or an
inflammatory related disorder in a subject in need thereof, said method comprising, administering to the subject a therapeutically effective amount of the extract of the O. stamineus leaves or a formulation comprising a therapeutically effective amount of the extract of the O. stamineus for the treatment of inflammation of an inflammatory related disorder by downregulating the activity and/or expression of IL-1, IL-6, IL-8, TNF-a, COX-1, COX-2, or any combination thereof.
[0121] One embodiment provides for a method of treating inflammation or an inflammatory related disorder by inhibiting or downregulating the activity of a receptor for IL-1, IL-6 (CD126), IL-8 (CXCR1), TNF-a, or any combination thereof, in a subject in need thereof, said method comprising, administering to the subject a therapeutically effective amount of the extract of O. stamineus leaves or a formulation comprising a therapeutically effective amount of the extract of the O. stamineus for treating inflammation or and inflammatory related disorder by downregulating the activity of a receptor for IL-1, IL-6 (CD126), IL-8 (CXCR1), TNF-a, or any combination thereof.
[0122] In one embodiment, the inflammatory related disorder is asthma, chronic peptic ulcer, tuberculosis, chronic periodontitis, colitis, ulcerative colitis, Crohn's disease, chronic sinusitis, chronic active hepatitis, acne vulgaris, autoimmune diseases, celiac disease, diabetes mellitus type 1, Graves disease, inflammatory bowel disease, multiple sclerosis, psoriasis, rheumatoid arthritis, and systemic lupus erythematosus, autoinflammatory diseases (also known as periodic fever syndromes or auto inflammatory syndromes), chronic prostatitis, diverticulitis, glomerulonephritis, hidradenitis suppurativa, hypersensitivities, allergies, interstitial cystitis, otitis, pelvic inflammatory disease, reperfusion injury, rheumatic fever, sarcoidosis, transplant rejection, vasculitis, atherosclerosis, myopathies, leukocyte defects, inflammation resulting from certain drugs or exogenous chemical compounds, cancer, HIV, AIDS, or any combination thereof.
[0123] In certain embodiments, a therapeutically effective amount of extract of O. stamineus leaves or a formulation comprising a therapeutically effective amount of the extract of O. stamineus leaves can be administered in combination with a therapeutically effective amount of at least one other therapeutic agent for the treatment of inflammation or inflammatory related disorders. In one embodiment, the at least one other therapeutic agent for the treatment of inflammation or inflammation related disorders can be a standard therapeutic agent for the treatment of inflammation or inflammation related disorders.
[0124] One embodiment features a method of treating an angiogenesis associated disorder in a subject, said method comprising, administering to the subject a therapeutically effective amount of the extract of O. stamineus leaves or a formulation comprising a therapeutically effective amount of the extract of O. stamineus leaves in combination with a
therapeutically effective amount of at least one anti-inflammatory agent for the treatment of the angiogenesis associated disorder.
[0125] In one embodiment, the extract of O. stamineus leaves comprises antioxidant activity.
[0126] One embodiment provides for a method of increasing the antioxidant activity in a subject in need thereof, said method comprising, administering to the subject a therapeutically effective amount of the extract of O. stamineus leaves or a formulation comprising a therapeutically effective amount of the extract of O. stamineus leaves for increasing antioxidant activity in the subject.
[0127] One embodiment features a method of treating an angiogenesis associated disorder, an inflammatory or an inflammatory related disorder, atherosclerosis, ischemic injury or a neurodegenerative disease by increasing the antioxidant activity in a subject in need thereof, said method comprising, administering to the subject a therapeutically effective amount of the extract of O. stamineus leaves or a formulation comprising a therapeutically effective amount of the extract of O. stamineus leaves for treating an angiogenesis associated disorder, an inflammatory or an inflammatory related disorder, atherosclerosis, ischemic injury or a neurodegenerative disease by increasing the antioxidant activity in the subject.
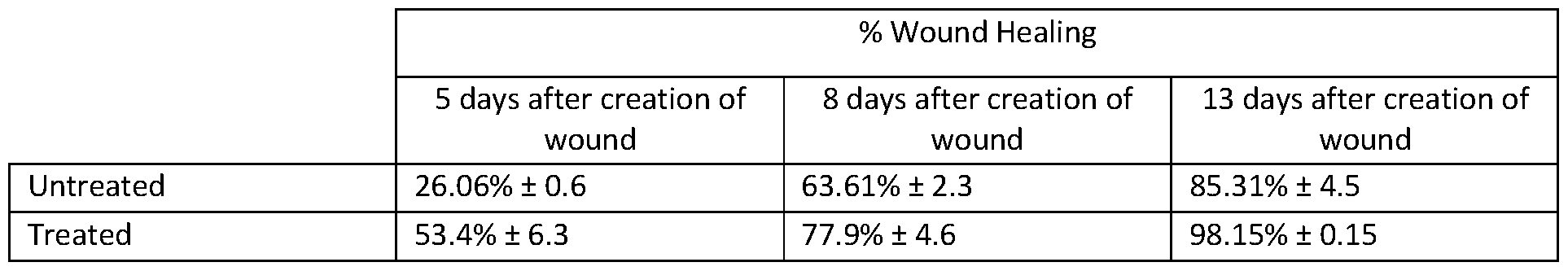
[0128] One embodiment provides a method of treating a skin condition comprising, topically applying to skin in need thereof a formulation comprising a therapeutically effective amount of the extract of O. stamineus leaves, wherein the formulation increases the antioxidant activity in the skin.
[0129] One embodiment provides for a method of treating a skin condition comprising, topically applying to skin in need thereof a topical formulation comprising a therapeutically effective amount of the extract of O. stamineus leaves in combination with another antioxidant.
[0130] One embodiment provides for a method of treating a skin condition comprising, topically applying to skin in need thereof a topical formulation comprising a therapeutically effective amount of the extract of O. stamineus leaves in combination with another antioxidant in combination with an anti-inflammatory agent.
[0131] One embodiment provides for a method of treating a skin condition comprising, topically applying to skin in need thereof a topical formulation comprising a therapeutically effective amount of the extract of O. stamineus leaves to reduce inflammation in combination with another plant and/or animal extract which other plant and/or animal extract promotes angiogenesis.
[0132] One embodiment provides for a method of treating a skin condition comprising, topically applying to skin in need thereof a topical formulation comprising a therapeutically effective amount of the extract of O. stamineus leaves to reduce inflammation in combination with a therapeutically effective amount of an extract of Channa striata fish.
[0133] In one embodiment, skin condition to be treated is dry skin, flaky skin, chapped skin, pruritus, spider veins, lentigo, age spots, senile purpura, keratosis, melasma, blotches, nodules, sun damaged skin, dermatitis (including, but not limited to seborrheic dermatitis, nummular dermatitis, contact dermatitis, atopic dermatitis, exfoliative dermatitis, perioral dermatitis, and stasis dermatitis), psoriasis, folliculitis, rosacea, acne, impetigo, erysipelas, erythrasma, eczema, sun burns, burned skin, open wounds, skin- inflammatory skin
conditions, exposure to UV light, age, irradiation, chronic sun exposure, environmental pollutants, air pollution, wind, cold, heat, chemicals, disease pathologies, smoking, lack of nutrition, skin cancer (including, but not limited to basal-cell carcinoma, squamous-cell carcinoma, and malignant melanoma), or any combination thereof.
[0134] In one embodiment, the topical formulation can be a cosmeceutical.
[0135] One embodiment provides for a method of treating an angiogenesis associated disorder in a subject, said method comprising administering a first, second and third therapeutic agent, wherein the first, second, and third therapeutic agents are different from each other, and wherein the first therapeutic agent is a therapeutically effective amount of the extract of O. stamineus leaves or a formulation comprising a therapeutically effective amount of the extract of O. stamineus leaves, the second therapeutic agent is a
therapeutically effective amount of an anti-angiogenic agent, and the third therapeutic agent is a therapeutically effective amount of an agent for the treatment of inflammation or an inflammatory related disorder. In certain embodiments, the therapeutic agents for the treatment of the angiogenesis associated disorder, inflammation or the inflammatory related disorder can be the standard therapeutic agent for the particular disorder.
[0136] One embodiment provides for a method of treating an angiogenesis associated disorder in a subject, said method comprising administering a first, second, third, and fourth therapeutic agent, wherein the first, second, third and fourth therapeutic agents are different from each other, and wherein the first therapeutic agent is a therapeutically effective amount of an extract of O. stamineus leaves or a formulation comprising a therapeutically effective amount of the extract of O. stamineus leaves, the second therapeutic agent is a therapeutically effective amount of an anti-angiogenic agent, the third therapeutic agent is a therapeutically effective amount of an agent for the treatment of inflammation or an inflammatory related disorder, and the fourth therapeutic agent is a therapeutically effective amount of an antioxidant.
[0137] In one embodiment, the extract of O. stamineus leaves can inhibit or downregulate the expression and/or activity of ACE-I.
[0138] One embodiment provides for a method of inhibiting or downregulating the expression and/or activity of ACE-I in a subject in need thereof, said method comprising, administering to the subject a therapeutically effective amount of the extract of O.
stamineus leaves or a formulation comprising a therapeutically effective amount of the extract of O. stamineus leaves for inhibiting or downregulating the activity of ACE-I.
[0139] One embodiment provides for a method of treating hypertension in a subject in need thereof, said method comprising, administering to the subject a therapeutically effective amount of the extract of O. stamineus leaves or a formulation comprising a therapeutically effective amount of the extract of O. stamineus leaves for treating hypertension.
[0140] Certain embodiments feature a method of inhibiting or downregulating the activity of ACE-I in a subject in need thereof, said method comprising, administering a therapeutically effective amount of the extract of O. stamineus leaves or a formulation comprising a therapeutically effective amount of the extract of O. stamineus leaves in combination with a therapeutically effective amount of another active agent that inhibits or downregulates ACE-I activity.
[0141] In a related embodiment, a method is provided for the treatment of hypertension in a subject in need thereof, said method comprising, administering to the subject a therapeutically effective amount of the extract of O. stamineus leaves or a formulation comprising a therapeutically effective amount of the extract of O. stamineus leaves in combination with a therapeutically effective amount of another antihypertensive agent for treating hypertension. In one embodiment, the other antihypertensive agent can be a standard therapeutic agent for the use of treating hypertension.
[0142] In one embodiment, the extract of O. stamineus leaves can inhibit or downregulate the expression and/or activity of AChE.
[0143] One embodiment provides for a method of inhibiting or downregulating the expression and/or activity of AChE in a subject in need thereof, said method comprising, administering to the subject a therapeutically effective amount of the extract of O.
stamineus leaves or a formulation comprising a therapeutically effective amount of the extract of O. stamineus leaves for inhibiting or downregulating the expression and/or activity of AChE.
[0144] One embodiment provides for a method for treating a neurological disorder in a subject in need thereof, said method comprising, administering to the subject a
therapeutically effective amount of the extract of O. stamineus leaves or a formulation comprising a therapeutically effective amount of the extract of O. stamineus leaves for the treatment of the neurological disorder.
[0145] In one embodiment, the neurological disorder includes, for example, vascular dementia, Alzheimer's disease (AD), Huntington's disease, Fragile X syndrome, Downs syndrome, Autism, Parkinson's disease (PD), prion disease, DLB, movement disorders (e.g., myasthenia gravis), and ALS.
[0146] In one embodiment the neurological disorder is a neurodegenerative disorder. In one embodiment, the neurodegenerative disorder is a disorder associated with an aging central nervous system.
[0147] One embodiment provides for a method of inhibiting or downregulating the expression and/or activity of AChE in a subject in need thereof, said method comprising, administering to the subject a therapeutically effective amount of the extract of O.
stamineus leaves or a formulation comprising a therapeutically effective amount of the extract of O. stamineus leaves in combination with another active agent which inhibits or downregulates the expression and/or activity of AChE.
[0148] One embodiment provides for a method of treating a neurological disorder in a subject in need thereof by inhibiting or down regulating the expression and/or activity of AChE in a subject in need thereof, said method comprising, administering to the subject a therapeutically effective amount of an extract of O. stamineus leaves or a formulation comprising a therapeutically effective amount of an extract of O. stamineus leaves for inhibiting or downregulating the expression and/or activity of AChE. In one embodiment, the neurological disorder can be a neurodegenerative disorder. In one embodiment, the neurodegenerative disorder is associated with an aging central nervous system.
[0149] One embodiment features a method of treating a neurological disorder in a subject in need thereof, said method comprising, administering to the subject the extract of O. stamineus leaves or a formulation comprising a therapeutically effective amount of the extract of O. stamineus leaves in combination with another therapeutic agent for the
treatment of the neurodegenerative disorder. In one embodiment, the neurological disorder can be a neurodegenerative disorder. In one embodiment, the neurodegenerative disorder is associated with an aging central nervous system.
[0150] In one embodiment, the extract of O. stamineus leaves can prevent or slow the progression of Αβ dependent or Αβ induced cell death.
[0151] One embodiment provides for a method of treating a neurological or ophthalmic disorder by preventing or slowing the progression of Αβ dependent or Αβ induced cell death in a subject in need thereof, said method comprising administering to the subject a therapeutically effective amount of an extract of O. stamineus leaves or a formulation comprising a therapeutically effective amount of an extract of O. stamineus leaves for preventing Αβ dependent or Αβ induced cell death. In one embodiment, the neurological disorder can be a neurodegenerative disorder. In one embodiment, the neurodegenerative disorder is associated with an aging central nervous system. In one embodiment, the opthlamic disorder is associated with an aging retina.
[0152] In certain embodiments, the extract of the O. stamineus leaves or formulations comprising the extract of the O. stamineus leaves inhibit angiogenesis by at least 40% (e.g., 40, 45, 50, 55, 60, 65, 70, 75, 80, 85, 90, 95 or 100%).
[0153] In certain embodiments, the extract of the O. stamineus leaves or formulations comprising the extract of the O. stamineus leaves inhibits endothelial cell migration in vitro by at least 40% (e.g., 40, 45, 50, 55, 60, 65, 70, 75, 80, 85, 90, 95 or 100%).
[0154] In certain embodiments, the extract of the O. stamineus leaves or formulations comprising the extract of the O. stamineus leaves inhibits tumor growth by at least 40% (e.g., 40, 45, 50, 55, 60, 65, 70, 75, 80, 85, 90, 95 or 100%).
[0155] In one embodiment, the extract of O. stamineus can be formulated together with at least one pharmaceutically acceptable excipient.
[0156] In one embodiment, the extract of O. stamineus can be formulated as a modified release formulation.
[0157] In one embodiment, the extract of O. stamineus can be formulated as an immediate release formulation.
[0158] In certain embodiments, the extract of O. stamineus can be formulated as granules, a normal release matrix or a controlled release matrix.
[0159] In certain embodiments, the granules, normal release or a controlled release matrices can form cores which can be coated with a suitable polymer based coat to modulate the release of the extract of O. stamineus leaves from the cores.
[0160] In certain embodiments, the suitable polymer based coat is a moisture barrier, controlled release coat, immediate release coat, or any combination thereof.
[0161] In certain embodiments, the formulations can take the form of an immediate release dosage form (oral or non-oral), a modified release dosage form (oral or non-oral), a sublingual film, a sublabial film, a buccal film, an ointment, a gel, dendrimers, an oral spray, an orally disintegrating tablet, a lozenge, an effervescent tablet, sublingual drops, a lollipop, a chewing gum, a solid immediate release dosage form (e.g. tablets, microspheres, granules, mini tablets, etc.), a modified release dosage form (e.g. tablets, microspheres, granules, mini tablets, etc.), a capsule, a gelcap, a pastille, multiparticulates (e.g., microspheres, granules, powder), a mini tablet, a caplet, an effervescent powder, a hydrogel, syrups, a medicated straw, a dry-powder inhaler, a nebulizer, a metered dose inhaler, a suppository, dendrimers,
a catheter, a vaginal tablet, a vaginal cream, a vaginal suppository, a vaginal ring, a dermal patch, a transdermal patch, ethosomes, niosomes, discosomes, phytosomes, liposomes, a lotion, a lip balm, an ointment, a cream, an emulsion, a topical spray, a nasal spray, a medicated shampoo, eye drops, an injectable, a topical emulsion, biodegradable microparticles, biodegradable microspheres, biodegradable nano-microspheres, nanoparticles, polymeric microparticles, polymeric nanoparticles, steroidal nano
microparticles, steroidal microparticles, silicon microneedles, or nanostructured lipid carriers.
[0162] In certain embodiments, the formulations comprise a pharmaceutically acceptable excipient which can be a binder, an emulsifying agent, a stabilizing agent, a preservative, a disintegrant, a taste masking agent, an effervescent couple, a diluent or filler, a lubricant, an anti-caking agent, an adsorbent, a surfactant, a buffering agent, a flavoring agent, a colorant, a plasticizer, a sustained-release ingredient, an extended release agent, a rate-controlling polymer, a viscosity-increasing agent, a mucoadhesive agent, an emollient, a granulating agent, a chelating agent, a film forming agent, a humectant, a coating agent, a penetration enhancer, a pore former, or any combination thereof.
[0163] In certain embodiments, the pharmaceutically acceptable excipient comprises β-Cyclodextrin. In certain embodiments, the ratio of the extract of the O. stamineus leaves to β-Cyclodextrin is from 1:0.5 to 1:6 (wt/wt) (e.g., 1:0.5, 1:1, 1:1.5, 1:2, 1:2.5, 1:3, 1:3.5, 1:4, 1:4.5, 1:5, 1:5.5, or 1:6). In certain embodiments, the β-Cyclodextrin is at least 0.5 times (wt/wt) the amount of the extract of O. stamineus leaves. In certain embodiments, the β- Cyclodextrin is 2.5 times (wt/wt) the amount of the extract of O. stamineus leaves.
[0164] In certain embodiments, the pharmaceutically acceptable excipient is a soluble polymer. In certain embodiments, the soluble polymer is poly(ethylene glycol),
polyvinylpyrrolidone, polyvinyl alcohol, polyacrylic acid, polyacrylamides, N-(2- Hydroxypropyl) methacrylamide, divinyl ether-maleic anhydride, polyoxazoline,
polyphosphates, polyphosphazenes, xanthan gum, pectins, chitosan derivatives, dextran, carrageenan, guar gum, cellulose ethers, hyaluronic acid, albumin, starch, starch based derivatives, or any combination thereof. In certain embodiments, the ratio of the extract of the O. stamineus leaves to the soluble polymer is 1:1 (wt/wt). In certain embodiments, the soluble polymer can be polyvinylpyrrolidone.
[0165] In certain other embodiments, the pharmaceutically acceptable excipient can be a poloxamer. In certain embodiments, the poloxamer is PLURONIC® 10R5, PLURONIC® 17R2, PLURONIC® 17R4, PLURONIC® 25R2, PLURONIC® 25R4, PLURONIC® 31R1, PLURONIC® F 108 Cast Solid Surfacta, PLURONIC® F 108 NF, PLURONIC® F 108 Pastille, PLURONIC® F 108 Prill, PLURONIC® F 108NF Prill Poloxamer 338, PLURONIC® F 127, PLURONIC® F 127 Prill, PLURONIC® F 127 NF, PLURONIC® F 127 NF 500 BHT Prill, PLURONIC® F 127 NF Prill
Poloxamer 407, PLURONIC® F 38, PLURONIC® F 38 Pastille, PLURONIC® F 68, PLURONIC® F 68 Pastille, PLURONIC® F 68 LF Pastille, PLURONIC® F 68 NF, PLURONIC® F 68 NF Prill Poloxamer 188, PLURONIC® F 68 Prill, PLURONIC® F 77, PLURONIC® F 77 Micropastille, PLURONIC® F 87, PLURONIC® F 87 NF, PLURONIC® F 87 NF Prill Poloxamer 237, PLURONIC® F 87 Prill,
PLURONIC® F 88, PLURONIC® F 88 Pastille, PLURONIC® F 88 Prill, PLURONIC® F 98,
PLURONIC® F 98, PLURONIC® F 98 Prill, PLURONIC® L 10, PLURONIC® L 101, PLURONIC® L 121, PLURONIC® L 31, PLURONIC® L 35, PLURONIC® L 43, PLURONIC® L 44, PLURONIC® L 61, PLURONIC® L 62, PLURONIC® L 62 LF, PLURONIC® L 62D, PLURONIC® L 64, PLURONIC® L 81,
PLURONIC® L 92, PLURONIC® L44 NF INH surfactant Poloxamer 124, PLURONIC® N 3, PLURONIC® P 103, PLURONIC® P 104, PLURONIC® P 105, PLURONIC® P 123 Surfactant, PLURONIC® P 65, PLURONIC® P 84, PLURONIC® P 85, or any combination thereof. In certain embodiments, the ratio of the extract of the O. stamineus leaves to the poloxamer is 1:1 (wt/wt). In at least one embodiment, the poloxamer is PLURONIC® F 68
(HO(C2H40)8o(C3H60)27(C2H40)8oH). In at least one other embodiment, the poloxamer is PLURONIC® F 127 (HO^hUOhoiiCsHeOjse^hUOjioiH).
[0166] In certain embodiments, the pharmaceutically acceptable excipient, is a combination of a soluble polymer and a poloxamer. In certain such embodiments, the ratio of the extract of the O. stamineus leaves to the soluble polymer to the poloxamer is 2:1:1 (wt/wt/wt). In certain embodiments, the soluble polymer can be polyvinylpyrrolidone and the poloxamer is PLURONIC® F 68, PLURONIC® F 127, or any combination thereof. In certain embodiments, the poloxamer can be PLURONIC® F 68. In certain other embodiments, the poloxamer can be PLURONIC® F 127.
[0167] In certain embodiments, the pharmaceutically acceptable excipient, is a combination of the extract of the O. stamineus leaves, a soluble polymer and a first and second poloxamer, wherein the first and second poloxamers are different and wherein the ratio of said extract to the soluble polymer to the first poloxamer to the second poloxamer is 2:1:1:1 (wt/wt/wt/wt). In at least one embodiment, the soluble polymer is
polyvinylpyrrolidone, the first poloxamer is PLURONIC® F 68 and the second poloxamer is PLURONIC® F 127.
[0168] In certain embodiments, the formulations comprise: (a) a therapeutically effective amount of the extract of the O. stamineus leaves, (b) an effervescent couple, (c) an anti-caking agent, and (d) a taste masking agent. In certain other embodiments, the formulation comprises, by weight based on the total weight of the formulation, (a) 8% - 17% of the extract of O. stamineus leaves (e.g., 8%, 8.5%, 9%, 9.5%, 10%, 10.5%, 11%, 11.5%, 12%, 12.5%, 13%, 13.5%, 14%, 14.5%, 15%, 15.5%, 16%, 16.5% or 17%), (b) 30% - 80% effervescent couple (e.g., 30%, 35%, 40%, 45%, 50%, 55%, 60%, 65%, 70%, 75%, or 80%), (c) 0.5% - 2% anti-caking agent (e.g., 0.5%, 0.6%, 0.7%, 0.8%, 0.9%, 1%, 1.1%, 1.2%, 1.3%, 1.4%, 1.5%, 1.6%, 1.7%, 1.8%, 1.9% or 2%),and (d) 14% - 50% taste masking agent (e.g., 14%, 16%, 18%, 20%, 22%, 24%, 26%, 28%, 30%, 32%, 34%, 36%, 38%, 40%, 42%, 44%, 46%, 48%, or 50%). In certain embodiments, the effervescent couple comprises, an acidic component and an alkaline component. In certain embodiments, the acidic component is anhydrous citric acid, tartaric acid, sodium gluconate, trisodium citrate, fumaric acid, malic acid, adipic acid, or any combination thereof. In certain embodiments, the alkaline component is anhydrous sodium, potassium, calcium bicarbonates, sodium glycine carbonates or any combination thereof. In certain embodiments, the effervescent couple is anhydrous sodium bicarbonate and anhydrous citric acid. In certain embodiments, the anti-caking agent is magnesium aluminometasilicate, tricalcium phosphate, powdered cellulose, magnesium stearate, sodium bicarbonate, sodium ferrocyanide, potassium ferrocyanide, calcium ferrocyanide, bone phosphate, sodium silicate, silicon dioxide, calcium silicate, magnesium trisilicate, talcum powder, sodium aluminosilicate, potassium aluminium silicate, calcium
aluminosilicate, bentonite, aluminium silicate, stearic acid, polydimethylsiloxane, or any combination thereof. In certain embodiments, the anti-caking agent is magnesium aluminometasilicate. In certain embodiments, the taste masking agent is a monosaccharide,
disaccharide, sugar alcohol, polydextrose, dextrate, maltodextrin, sugar substitute, cyclodextrin, flavouring agent, or any combination thereof. In certain embodiments, the taste masking agent is a combination of β-cyclodextrin, sucralose, and citron flavouring.
[0169] In certain embodiments, the formulations comprise, by weight based on the total weight of the formulation, (a) 8.3% of the extract of O. stamineus leaves, 75% effervescent couple, 1.5% anti-caking agent, and 15.2% taste masking agent. In certain embodiments, the effervescent couple comprises 33% sodium bicarbonate and 42% citric acid, the anti-caking agent is magnesium aluminometasilicate, and the taste-masking agent comprises 8.6%, β-cyclodextrin, 5% citron flavouring and 1.6% sucralose.
[0170] In certain other embodiments, the formulations comprise, by weight based on the weight of the total formulation, (a) 16.5% of the extract of O. stamineus leaves, (b) 35.5% effervescent couple, (c) 1% anti-caking agent, and (d) 47% taste-masking agent. In certain embodiments, the effervescent couple comprises 8.3% sodium bicarbonate and 27.2% citric acid, the anti-caking agent is magnesium aluminometasilicate, and the taste masking agent comprises, 41% β-cyclodextrin, 5% citron flavouring and 1% sucralose.
[0171] In certain embodiments, the formulations comprise from 100 mg - 2000 mg of the extract of O. stamineus leaves (e.g., 100, 125, 150, 175, 200, 225, 250, 275, 300, 325, 350, 375, 400, 425, 450, 475, 500, 525, 550, 575, 600, 625, 650, 675, 700, 725, 750, 775, 800, 825, 850, 875, 900, 925, 950, 975, 1000, 1025, 1050, 1075, 110, 1125, 1150, 1175, 1200, 1225, 1250, 1275, 1300, 1325, 1350, 1375, 1400, 1425, 1450, 1475, 1500, 1525, 1550, 1575, 1600, 1625, 1650, 1675, 1700, 1725, 1750, 1775, 1800, 1825, 1850, 1875, 1900, 1925, 1950, 1975, or 2000 mg). In certain embodiments, the formulations comprise 250 mg - 1000 mg (e.g., 250, 260, 270, 280, 290, 300, 310, 320, 330, 340, 350, 360, 370, 380, 390, 400, 410, 420, 430, 440, 450, 460, 470, 480, 490, 500, 510, 520, 530, 540, 550, 560, 670, 580, 590, 600, 610, 620, 630, 640, 650, 660, 670, 680, 690, 700, 710, 720, 730, 740, 750, 760, 770, 780, 790, 800, 810, 820, 830, 840, 850, 860, 870, 880, 890, 900, 910, 920, 930, 940, 950, 960, 970, 980, 990, or 1000 mg) of the extract of O. stamineus leaves. In certain embodiments, the formulations comprise 250 mg of the extract of the O. stamineus leaves. In certain other embodiments, the formulations comprise 1000 mg of the extract of the O. stamineus leaves.
[0172] One embodiment features a tablet dosage form comprising 1000 mg of the extract of O. stamineus leaves which provides a Tmax of 0.5 ± 0.2 (hr), a Cmax of 10 ± 3.44 (ng/ml), an AUQM of 13.9 ±7.74 (ng.hr/ml), an AUCo-inf of 60 ± 120.4 (ng.hr/ml), and ti/2 of 15 ± 38.41 (hr) for A.
[0173] One embodiment features an effervescent dosage form comprising 1000 mg of the extract of O. stamineus leaves which provides a Tmax of 0.5 ± 0.2 (hr), a Cmax of 17 ± 6
(ng/ml), an AUQM of 20.57 ± 11.1 (ng.hr/ml), an AUCo-inf of 30.5 ± 19.3 (ng.hr/ml), and ti/2 of 3 ± 4 (hr) for RA.
[0174] In one embodiment, formulations in the form of a topical cream, topical spray, moisturizer, a lotion, a skin softener, a foundation, a night cream, a lipstick, a cleanser, a toner, a sunscreen, a mask, and an anti-aging product can comprise ethosomes comprising a therapeutically effective amount of an extract of O. stamineus leaves, a phospholipid, a sophorolipid, or any combination thereof.
[0175] One embodiment features a formulation comprising a therapeutically effective amount of an extract O. stamineus leaves and a sophorolipid for the treatment of a dermal disorder.
[0176] One embodiment features a formulation comprising a therapeutically effective amount of an extract of O. stamineus leaves and a sophorolipid for the treatment of melanoma.
[0177] One embodiment features a formulation comprising a therapeutically effective amount of an extract O. stamineus leaves and a sophorolipid for the treatment of a wound.
[0178] One embodiment features a formulation comprising, by weight based on the total weight of the formulation, (a) 5% - 10% of Channa striata fish extract (e.g., 5, 5.5, 6, 6.5, 7, 7.5, 8, 8.5, 9, 9.5 or 10%) (b) 8% - 10% of virgin coconut oil (e.g., 8, 8.1, 8.2, 8.3, 8.4, 8.5, 8.6, 8.7, 8.8, 8.9, 9, 9.1, 9.2, 9.3, 9.4, 9.5, 9.6, 9.7, 9.8, 9.9 or 10%), (c) 10% - 15% of cetyl alcohol (e.g., 10, 10.2, 10.4, 10.6, 10.8, 11, 11.2, 11.4, 11.6, 11.8, 12, 12.2, 12.4, 12.6, 12.8, 13, 13.2, 13.4, 13.6, 13.8, 14, 14.2, 14.4, 14.6, 14.8, or 15%), (d) 0.5% - 1% of vitamin E (e.g., 0.5, 0.6, 0.7, 0.8, 0.9 or 1%), (e) 35% - 60% purified water (e.g., 35, 38, 40, 42, 44, 46, 48, 50, 52, 54, 56, 58 or 60%), (f) 1% - 5% Malaysian Tualang honey (e.g., 1, 1.2, 1.4, 1.6, 1.8, 2, 2.2, 2.4, 2.6, 2.8, 3, 3.2, 3.4, 3.6, 3.8, 4, 4.2, 4.4, 4.6, 4.8, or 5%), (g) 15% - 22% bee's wax (e.g., 15, 15.5, 16, 16.5, 17, 17.5, 18, 18.5, 19, 19.5, 20, 20.5, 21, 21.5 or 22%), and (h) 0.5% - 5% (e.g., 0.5, 0.55%, 0.6, 0.65, 0.7, 0.75, 0.8, 0.85, 0.9, 0.95, 1, 1.5, 2, 2.5, 3, 3.5, 4 or 4.5%) of a 1:1 (vol/vol) EtOH to water extract of O. stamineus leaves comprising <0.2% (wt/wt of the extract of O. stamineus leaves) TMF, such that the total weight percent of (a) + (b) + (c) + (d) + (e) + (f) + (g) + (h) is 100%. In other embodiments, the formulation can comprise 0.5% - 5% of a 1:1 (vol/vol) EtOH to water extract of O. stamineus leaves comprising <0.1% (wt/wt of the extract of O. stamineus leaves) TMF. In other embodiments, the formulation can further comprise TMF, by weight based on the total weight of the formulation, from greater than 0.1% - 2% (e.g., 0.11, 0.15, 0.2, 0.25, 0.3, 0.35, 0.4, 0.45, 0.5, 0.5, 0.6, 0.65, 0.7, 0.75, 0.8, 0.85, 0.9, 0.95, 1, 1.5, or 2%). In other embodiments, the formulation can comprise 0.5% - 5% of a 1:1 (vol/vol) EtOH to water extract of O. stamineus leaves comprising <0.1% (wt/wt of the extract of O. stamineus leaves) TMF. In other embodiments, the formulation can further comprise TMF, by weight based on the total weight of the formulation, from greater than 0.1% - 2% (e.g., 0.11, 0.15, 0.2, 0.25, 0.3, 0.35, 0.4, 0.45, 0.5, 0.5, 0.6, 0.65, 0.7, 0.75, 0.8, 0.85, 0.9, 0.95, 1, 1.5, or 2%). In one embodiment, the formulation can be in the form of a topical cream, topical spray, moisturizer, a lotion, a skin softener, a foundation, a night cream, a lipstick, a cleanser, a toner, a sunscreen, a mask, and an anti-aging product.
[0179] Certain embodiments provide for phytosome formulations comprising a therapeutically effective amount of the extract of O. stamineus leaves. In one embodiment, the phytosome comprises a phospholipid. In one embodiment, the phytosome comprises a lecithin.
[0180] Certain other embodiments provide for ethosome formulations comprising a therapeutically effective amount of the extract of O. stamineus leaves. In one embodiment, the ethosome comprises a phospholipid. In one embodiment, the ethosome comprises phosphotidylcholine. In one other embodiment, the ethosome comprises a sophorolipid.
[0181] In one embodiment, the route of administration for the extract of O. stamineus or route of administration of formulations comprising the extract of O. stamineus leaves is sublingual, sublabial, buccal, digestive tract, respiratory tract, rectal, extra-amniotic administration, intraarterial, intraarticular, intracardiac, intracavernous, intradermal, intralesional, intramuscular, intracerebral, intracerebroventricular, intraocular, intraosseous, intraperitoneal, intrathecal, intravaginal, intravenous, intravesical, ophthalmic, otologic,
urogenital, dermal, epidural, subcutaneous, vaginal, dermal, ophthalmic, otologic, or any combination thereof.
[0182] Certain embodiments provide for kits comprising the extract of O. stamineus leaves either alone or in combination with other therapeutic agents.
[0183] Certain embodiments comprise a kit comprising a suitable dosage form comprising a therapeutically effective amount of the extract of O. stamineus leaves in a package together with instructions for the treatment of an angiogenesis associated disorder in a subject in need thereof, wherein said instructions include instructions for the administration of said dosage form.
[0184] Certain embodiments comprise a kit comprising a suitable dosage form comprising a therapeutically effective amount of the extract of O. stamineus leaves in a package together with instructions for the treatment of inflammation or an inflammatory related disorder in a subject in need thereof, wherein said instructions include instructions for the administration of said dosage form.
[0185] Certain embodiments comprise a kit comprising a suitable dosage form comprising a therapeutically effective amount of the extract of O. stamineus leaves in a package together with instructions for the treatment of hypertension in a subject in need thereof, wherein said instructions include instructions for the administration of said dosage form.
[0186] Certain embodiments comprise a kit comprising a suitable dosage form comprising a therapeutically effective amount of the extract of O. stamineus leaves in a package together with instructions for the treatment of hyperglycemia in a subject in need thereof, wherein said instructions include instructions for the administration of said dosage form.
[0187] Certain embodiments comprise a kit comprising a suitable dosage form comprising a therapeutically effective amount of the extract of O. stamineus leaves in a package together with instructions for the treatment of a neurological disorder in a subject in need thereof, wherein said instructions include instructions for the administration of said dosage form.
[0188] Certain embodiments comprise a kit comprising a suitable dosage form comprising a therapeutically effective amount of the extract of O. stamineus leaves in a package together with instructions for the treatment of a dermal disorder in a subject in need thereof, wherein said instructions include instructions for the administration of said dosage form.
[0189] Certain embodiments provide for functional foods comprising a therapeutically effective amount of the extract of O. stamineus leaves or a formulation comprising a therapeutically effective amount of the extract of O. stamineues leaves either alone or in combination with other therapeutic agents.
[0190] Certain embodiments provide for dietary supplements comprising a therapeutically effective amount of the extract of O. stamineus leaves or a formulation comprising a therapeutically effective amount of the extract of O. stamineues leaves either alone or in combination with other therapeutic agents.
[0191] Certain embodiments provide for a cosmeceutical comprising the extract of O. stamineus leaves either alone or in combination with other therapeutic agents.
[0192] In certain embodiments, the subject is a mammal, including but not limited to a dog, cat, horse, cow, pig, sheep, goat, rodent, primate or human. In certain embodiments, the human subject can be a pediatric, adult, or a geriatric subject, and can be of either gender. In other embodiments, the subjects include animals such as house pets (e.g., dogs, cats, and the like), agricultural stock subjects (e.g., cows, horses, pigs, chickens, etc.), laboratory subjects (e.g., mice, rats, rabbits, etc.), but are not so limited.
BRIEF DESCRIPTION OF THE DRAWINGS
[0193] FIGURE 1, comprising Figures 1A and IB, illustrates chromatograms generated using High Performance Liquid Chromatography at 320 nm. Figure 1A illustrates a chromatogram of standard markers for A, TMF, SIN, and EUP. Figure IB illustrates a chromatogram of a 1:1 (vol/vol) EtOH to water (50% EtOH) extract of O. stamineus leaves manufactured as described in Example 1.
[0194] FIGURE 2, comprising Figure 2A through Figure 2F, is a series of images showing the effects of an extract of O. stamineus leaves manufactured as described in Example 1, and RA on aggregation of HCT-116 cells in-vitro in a hanging drop assay. Figure 2A shows the negative control group. Figure 2B shows the effect of the extract at 100μg/mL. Figure 2C shows the effect of the extract at 200μg/mL. Figure 2D shows the effect of the extract at 300μg/mL. Figure 2E shows the effect of RA at 100μg/mL. Figure 2F shows the effect of Betulinic acid at 100μg/mL. Cells were photographed by fluorescence microscope at 40X magnification.
[0195] FIGURE 3, comprising Figures 3A through 3F, is a series of images showing hematoxylin/eosin staining of crosses sections of tumors harvested from orthotopic xenografts of human colorectal tumor-bearing mice 35-days after implantation into the cecal wall of nude mice treated or untreated with an extract of O. stamineus leaves manufactured as described in Example 1. Figure 3A is a cross-section of a tumor from untreated mice showing minimal necrosis, compact cells and abundant blood vessels indicted by the arrows. Figure 3B is a cross-section of a tumor from mice treated with the extract at 100 mg/kg body weight. Figure 3C is a cross-section of a tumor from mice treated with the extract at 200 mg/kg body weight. Figure 3D is a cross-section of a tumor from mice treated with the extract at 400 mg/kg body weight. Figure 3E is a cross-section of a tumor from mice treated with RA at 30 mg/kg body weight. Figure 3F is a cross-section of a tumor from mice treated with 30mg/kg body weight imatinib. "V" refers to viable tumor cells, "N" refers to necrotic/apoptotic tumor cells and "BV" refers to blood vessels. The pictures were taken at 20X magnification.
[0196] FIGURE 4, comprising Figures 4A through 4C, is a series of images showing the gross morphology and size of tumors of human colorectal cancer cells ectopically grafted in nude mice pre-treated or untreated for 14 days with an extract of O. stamineus leaves manufactured as described in Example 1 prior to implantation of the colorectal cancer cells for 28 days. Figure 4A shows the size of the tumor in a negative control. Figure 4B shows the size of tumors from mice pre-treated with 200mg/kg body weight of the extract. Figure 4C shows the size of tumors from mice pre-treated with 400mg/kg body weight of the extract.
[0197] FIGURE 5, comprising Figure 5A through 5C, is a series of images showing haematoxylin/eosin stained cross sections of tumor tissues excised from nude mice pre- treated for 14-days with an extract of O. stamineus leaves manufactured as described in
Example 1 prior to ectopic xenograft implantation of human colon cancer cells. Figure 5A shows the extent of necrotic areas in tumors excised from animals in the negative control group. Figure 5B shows the extent of necrotic areas in tumors excised from animals pre- treated with 200mg/kg body weight of the extract. Figure 5C shows the extent of necrotic areas in tumors excised from animals pre-treated with 400 mg/kg body weight of the extract. "V" refers to viable tumor cells, "N" refers to necrotic tumor cells, and "BV": refers to blood vessels. The pictures were taken at 20X magnification.
[0198] FIGURE 6, comprising Figures 6A through 6H, is a series of images showing the gross morphology and size of tumors excised from nude mice implanted ectopically with human lung adenocarcinoma cells and treated with an unformulated extract of O. stamineus leaves manufactured as described in Example 1, said extract formulated as a nano-liposome (NP2), imatinib, or vehicle. Figure 6A shows a series of tumors from untreated negative control (NC) mice. Figure 6B shows a series of tumors excised from mice treated with 20mg/kg body weight of positive control (PC), imatinib. Figure 6C shows a series of tumors excised from mice treated with lOOmg/kg body weight of the extract (E-100). Figure 6D shows a series of tumors excised from mice treated with 200mg/kg body weight of the extract (E-200). Figure 6E shows a series of tumors excised from mice treated with 400mg/kg body weight of the extract (E-400). Figure 6F shows a series of tumors excised from mice treated with lOOmg/kg body weight NP2 (NP2-100). Figure 6G shows a series of tumors excised from mice treated with 200mg/kg body weight NP2 (NP2-200). Figure 6H shows a series of tumors excised from mice treated with 400mg/kg body weight NP2 (NP2-400).
[0199] FIGURE 7, comprising Figures 7A through 7D, is a series of images showing the effect of an extract of O. stamineus leaves manufactured as described in Example 1 after 21 days of treatment in diabetic rats compared to normal rats on vascular normalization associated with diabetic retinopathy. Figures 7A through 7D shows fundus photographs of rats treated with a gel composition comprising vehicle or a gel composition comprising the extract for 21-days. Figure 7A shows left eye of normal rat treated with gel composition comprising vehicle. Figure 7B shows right eye of normal rat treated with gel composition comprising the extract. Figure 7C shows left eye of diabetic rat treated with gel composition comprising vehicle (arrow indicates vessel tortuosity). Figure 7D shows right eye of diabetic rat treated with gel composition comprising the extract. OD = optic disk, V = retinal vessel.
[0200] FIGURE 8, shows the effect of two different formulations of an extract of O. stamineus leaves manufactured as described in Example 1 in lowering blood glucose in Type 2 diabetic patients.
[0201] FIGURE 9, comprising Figure 9A and Figure 9B, illustrates chromatograms generated using High Performance Liquid Chromatography at 320 nm. Figure 9A illustrates a chromatogram of a 1:1 (vol/vol) EtOH to water (50% EtOH) extract of O. stamineus leaves manufactured as described in Example 1 formulated as ethosomes comprising
phosphatidylcholine at a ratio of 6:1 (wt/wt) of phosphatidylcholine to extract. Figure 9B illustrates the chromatogram of an unformulated extract of O. stamineus leaves manufactured as described in Example 1.
[0202] FIGURE 10, comprising Figure 10A and Figure 10B, shows the in-vitro wound healing activity of a formulation comprising Channa striata fish extract in combination with a low concentration of an extract of O. stamineus leaves manufactured as described in Example 1. Figure 10A shows the effect of the formulation on HUVEC cell migration at at
escalating concentrations of the formulation compared to vehicle over a 18 hour period. Figure 10B illustrates the percent wound closure at concentrations of 12, 25, 50 and 100 μg/ml of the formulation over an 18 hr period.
[0203] FIGURE 11, comprises a series of figures showing the in-vivo wound healing activity in an excision wound healing assay of a formulation comprising Channa striata fish extract in combination with a low concentration of an extract of O. stamineus leaves manufactured as described in Example 1. N.C. = Negative Control (Vehicle), P.C. = Positive Control (Sulphathiazole).
[0204] FIGURE 12, shows the effect of a formulation comprising Channa striata fish extract in combination with a low concentration of an extract of O. stamineus leaves manufactured as described in Example 1 on the the expression of VEGF in HUVECS.
[0205] FIGURE 13 shows the effect of a formulation comprising Channa striata fish extract in combination with a low concentration of an extract of O. stamineus leaves manufactured as described in Example 1 on neovascularization with increasing
concentrations of the formulation compared to control (vehicle).
[0206] FIGURE 14, shows the effect of a formulation comprising Channa striata fish extract in combination with a low concentration of an extract of O. stamineus leaves manufactured as described in Example 1 on inflammation in a carrageenan induced rat paw edema assay.
[0207] FIGURE 15, comprising Figure 15A through Figure 15D, is a series of images showing the antimicrobial activity of a formulation comprising Channa striata fish extract in combination with a low concentration of an extract of O. stamineus leaves manufactured as described in Example 1. Figure 15A shows the antimicrobial activity of the formulation against Staphylococcus aureus. Figure 15B shows the antimicrobial activity of the formulation against Escherichia coli. Figure 15C shows the antimicrobial activity of the formulation against Aspergillus. Figure 15D shows the antimicrobial activity of the formulation against Trichoderma.
DETAILED DESCRIPTION OF THE INVENTION
[0208] The present invention relates to an extract of O. stamineus leaves, formulations comprising such an extract, and methods of using such an extract or formulations comprising such an extract for the treatment of a variety of physiological disorders. One such physiological disorder is an angiogenesis associated disorder.
[0209] While the present invention is capable of being embodied in various forms, the description below of the embodiments is made with the understanding that the present disclosure is to be considered as an exemplification of the invention, and is not intended to limit the invention to the specific embodiments described or illustrated. Headings are provided for convenience only and are not to be construed to limit the invention in any manner. Embodiments described or illustrated under any heading can be combined with embodiments described or illustrated under any other heading.
[0210] The numerical values specified throughout this disclosure, are stated as approximations as though the numerical values are preceded by the word "about" unless expressly stated otherwise. Similarly, where a range of numeric values are specified, the minimum and maximum values of the range as well as all values within the range are stated as approximations as though preceded by the word "about" unless expressly stated
otherwise. In this manner, equivalent variations from a stated value can be used to achieve substantially the same results as the stated value. Also, the disclosure of ranges is intended as a continuous range including every value between the minimum and maximum values recited as well as any ranges that can be formed by such values. Also, disclosed herein are all ratios (and ranges of any such ratios) that can be formed by dividing a recited numeric value into any other recited numeric value. Accordingly, the skilled person will appreciate that many such ratios, ranges, and ranges of ratios can be unambiguously derived from the numerical values presented herein and in all instances, such ratios, ranges, and ranges of ratios represent various embodiments of the present invention.
[0211] The term "a" or "an" as used herein means "one" or "one or more".
[0212] The term "angiogenic associated disorder(s)" or "angiogenesis associated disorders" are diseases or physiological disorders dependent on or associated with abnormal or excessive vascularization.
[0213] Unless expressly stated otherwise, the term "extract of O. stamineus leaves" refers to a 1:1 (vol/vol) water to ethanol extract of O. stamineus leaves manufactured as described in Example 1.
[0214] As used herein, the term "standardized extract" means a form of an extract derived from of an herb comprising a concentrated but set percentage (standardized) of medicinally active botanical ingredients. The standardized extract can be in the form of a liquid, solid or emulsion. Standardized extracts provide a consistent therapeutic dosage strength, or therapeutic potency, from one batch of the extract to the next. Methods of standardizing herbal extracts are well known to the person of ordinary skill. For example, one method of standardizing an extract is to identify and quantify the extract to one or more known chemical marker compounds. Another method identifies and concentrates one or more bioactive phytochemicals or phytoconstituents in a defined and optimum proportion in the extract. Standardized extracts comprising such phytoconstituents exhibit batch to batch consistency in therapeutic efficacy of the extract. Bioactive compounds present in standardized extracts can comprise proteins, polysaccharides, glycosaponins, phenolic compounds, flavonoids or mixtures thereof. Methods for standardizing herbal extracts include the use of analytical instruments such as HPLC, FTI , MS, NMR, and TLC.
[0215] The term "formulation(s)" or "composition(s)" as used herein includes therapeutic and dietary compositions including, but not limited to dietary supplements, nutraceutical formulations, or pharmaceutical formulations comprising the extract of O. stamineus leaves alone or in combination with either food additives and/or
pharmaceutically acceptable excipients and additional inert ingredients. The formulations can be manufactured into a variety of dosage forms dependent on the route of
administration, which can vary with the location and nature of the condition to be treated. A "dosage form" is the physical manifestation containing the active and inactive ingredients that delivers a dose of the drug product. This includes such factors as the physical appearance of the drug product; the physical form of the drug product prior to dispensing to the patient; the way the product is administered; and the design features that affect frequency of dosing. Non-limiting examples of dosage forms include, immediate release dosage forms (oral or non-oral), modified release dosage forms (oral or non-oral), sublingual films, sublabial films, buccal films, ointments, gels, dendrimers, oral sprays, orally disintegrating tablets, lozenges, effervescent tablets, sublingual drops, lollipops, chewing
gums, solid immediate release dosage forms (e.g. tablets, microspheres, granules, mini tablets, etc.), modified release dosage forms (e.g. tablets, microspheres, granules, mini tablets, etc.), capsules, gelcaps, pastilles, multiparticulates (e.g., microspheres, granules, powder), mini tablets, caplets, effervescent powders, hydrogels, syrups, medicated straws, dry-powder inhalers, nebulizers, metered dose inhalers, suppositories, vaginal tablets, vaginal creams, vaginal suppositories, vaginal rings, dermal patches, transdermal patches, ethosomes, niosomes, discosomes, phytosomes, liposomes, lotions, lip balms, creams, emulsions, topical sprays, nasal sprays, medicated shampoos, eye drops, injectables, topical emulsions, biodegradable microparticles, biodegradable microspheres, biodegradable nano- microspheres, nanoparticles, polymeric microparticles, polymeric nanoparticles, steroidal nano microparticles, steroidal microparticles, silicon microneedles, and nanostructured lipid carriers. It should be noted that in embodiments comprising formulations described herein, the total of all ingredients comprising the formulations does not exceed 100% (wt/wt of the tablet).
[0216] The term "functional food" as used herein means any edible or drinkable foods or dietary components (e.g., juices, milk, yogurt, butter, margarine, baking products) that are fortified or enhanced with the extract of O. stamineus leaves or formulations comprising the extract of O. stamineus leaves. The functional food can be, e.g., solid, liquid, semisolid, or a combination thereof. The term "functional food" also encompasses edible and drinkable nutritional supplements.
[0217] The standardized extract as a whole, can constitute the active pharmaceutical ingredient. As used herein, the term "Active Pharmaceutical Ingredient" or "API",
"therapeutic agent", "pharmacologically active molecules", "phytochemical compounds", "active(s)", "active ingredient(s)", "active agents", "pharmaceutically active ingredient", or "active drug" is used interchangeably and is intended to furnish pharmacological activity or to otherwise have direct effect in the diagnosis, cure, mitigation, treatment or prevention of disease, or to have direct effect in restoring, correcting or modifying physiological functions in a subject. Accordingly, the extract of O. stamineus leaves described herein can be defined as an API, active, therapeutic agent, active drug, active ingredient, active agent, or pharmaceutically active ingredient.
[0218] As used herein "TM F" refers to 3'-hydroxy-5,6,7,4'- tetramethoxyflavone.
[0219] The term "substantially similar" as used herein refers to the possibility that small differences in factors and concentration of factors can exist between two extracts even after following the same extraction procedure, but that these small differences do not affect the properties of the extract as measured and described herein for the extract of O.
stamineus leaves of the invention.
[0220] As used herein, a "dose" refers to a specified quantity of the therapeutic agent prescribed to be taken at one time or at stated intervals. The therapeutic agent can be the extract of O. stamineus leaves alone or co-administered with another therapeutic agent, which can be an anti-angiogenic agent (e.g, a chemotherapeutic agent), an antiinflammatory agent, an antioxidant, an antihyperglycemic agent, an antihypertensive agent, or a neuroprotective agent.
[0221] "Modified release formulations" as used herein is as defined by the United States Pharmacopoeia (USP) as those whose active drug release characteristics of time course and/or location are chosen to accomplish therapeutic or convenience objectives not
offered by conventional, immediate release or uncoated normal release matrix
formulations. The rate of release of the API from a modified release formulation is controlled by features of the formulation and/or in combination with physiologic or environmental conditions. The design of conventional, immediate release or uncoated normal release matrix formulations is generally based on getting the fastest possible rate of drug release. Modified release formulations, on the other hand, avoid large peak-to-trough fluctuations normally seen with conventional or immediate release formulations and can provide a substantially flat serum concentration curve throughout the therapeutic period. The modified release formulations of the invention can be constructed in many forms known to one of ordinary skill in the drug delivery arts and described in the prior art such as for example, "modified release matrix formulations", "normal release matrix formulations" coated with at least one "control-releasing coat", "osmotic formulations", "multiparticulate formulations", and "gastric retention formulations". The USP considers the terms controlled release, prolonged release and sustained release as interchangeable. Accordingly, the terms "modified-release", controlled-release", "control-releasing", "rate-controlled release", "prolonged-release", and "sustained-release" are used interchangeably herein. As used herein, the definition of the terms "modified-release" encompasses the scope of the definitions for the terms "extended release", "enhanced-absorption", "controlled release", and "delayed release".
[0222] The terms "osmagent", "osmotic agent", "osmotically effective solute",
"osmotic enhancer" "osmotically effective compounds", "osmotic solutes", or "osmotic fluid imbibing agents" are all used interchangeably herein and define any material that increases the hydrostatic pressure within an osmotic formulation. The osmagent can be either soluble or swellable and totally or partially solubilized. The osmagent can be the extract of O.
stamineus leaves.
[0223] The term "normal release matrix" as used herein is defined to mean formulations in which the extract of O. stamineus leaves is dispersed within a matrix, which matrix can be either insoluble, soluble, or combinations thereof but constructed such that the release of the extract of O. stamineus leaves mimics the release rate of an uncoated non-matrix conventional or immediate release formulation comprising the extract of O. stamineus leaves. The release rate from normal release matrix formulations can be slowed down or modified in conjunction with a "control releasing coat".
[0224] The term "controlled release matrix" as used herein is defined to mean formulations in which the API (e.g., the extract of O. stamineus leaves) is dispersed within a matrix, which matrix can be either insoluble, soluble, or combinations thereof but constructed such that the release of the API slows the release rate of the API when compared to a normal release matrix or an uncoated non-matrix conventional or immediate release formulation comprising the API. The release rate from control release matrix formulations can be further slowed down or modified in conjunction with a "control releasing coat".
[0225] A "control releasing coat" or "controlled release coat" as used herein is defined to mean a functional coat which can, for example, comprise at least one pH independent polymer, pH dependent polymer (e.g., enteric or reverse enteric types), soluble polymer, insoluble polymer, lipids, lipidic materials or combinations thereof, which when applied onto a formulation can slow (e.g., when applied to a normal release matrix formulation), further
slow (e.g., when applied to a controlled release matrix formulation) or modify the rate of release of an API (e.g., the extract of O. stamineus leaves) when applied to an uncoated formulation. For example, the control releasing coat can be designed such that when the control releasing coat is applied to a formulation, the formulation in conjunction with the control releasing coat can exhibit the release of the API, such as for example, as a "modified- release", "controlled-release", "sustained-release", "extended-release", "delayed-release", "prolonged-release" or combinations thereof. The "control releasing coat" can optionally comprise additional materials that can alter the functionality of the control releasing coat.
[0226] The term "moisture barrier" as used herein is one, which impedes or retards the absorption of moisture. The extract of O. stamineus leaves is hygroscopic and as such is susceptible to decomposition over time under high humidity conditions. Accordingly, the application of a suitable moisture barrier can prolong the shelf life of the extract, especially in high humidity environments. Suitably, the moisture barrier is comprised of an enteric and/or acrylic polymer, suitably an acrylic polymer, optionally a plasticizer, and a permeation enhancer. The permeation enhancer is a hydrophilic substance, which allows water to enter without physical disruption of the barrier. The moisture barrier can additionally contain other conventional inert excipients, which can improve processing of modified release formulations described herein.
[0227] The term "core" as used herein, in the context of a formulation or dosage form, is defined to mean any structure that is not surrounded by a wall, membrane, or coating. Accordingly, such structures are uncoated cores. The wall, membrane, or coating of a coated core can be a functional or non-functional coating.
[0228] The term "microparticle", as used herein refers to a drug formulation in discrete particulate form, and is interchangeable with the terms "core", "microspheres", "spherical particles", "microcapsules", "particles", "multiparticulates", "granules", "spheroids", beads" and "pellets". Microparticles can be designed as immediate release or modified release microparticles. Microparticles can be coated with a control releasing coat and or a moisture barrier.
[0229] As used herein, an "effective amount" or "therapeutically effective amount" of a composition as described in certain embodiments herein can be a quantity sufficient to achieve a desired therapeutic and/or prophylactic effect, for example, an amount which results in the prevention of, or a decrease in the symptoms associated with, a disease or physiological disorder that is being treated. The amount (e.g., the dose of the extract of O. stamineus leaves) administered to the subject can depend on the type and severity of the disease or physiological disorder and on the characteristics of the subject, such as subject type (i.e., human or animal), general health, age, sex, body weight and tolerance to drugs. A skilled person will be able to evaluate appropriate dosages depending on these and other factors. Typically, an effective amount of the extract of O. stamineus leaves can be sufficient for achieving a therapeutic or prophylactic effect.
[0230] In certain embodiments, the term "subject" or "patient" as used herein includes, but is not limited to, house pets (e.g., dogs, cats, or rodents), agricultural stock subjects (e.g., horses, cows, pigs, sheep, goats, chickens), laboratory subjects (e.g., mice, rats, rabbits, etc.), primates or humans. A human subject can be a pediatric, adult, or a geriatric subject, and can be of either gender.
[0231] As used herein, "treatment" is an approach for obtaining beneficial or desired results, including clinical results. Beneficial or desired clinical results can include, but are not limited to, alleviation or amelioration of one or more symptoms or conditions, diminishment of extent of disease, stabilized (i.e. not worsening) state of disease, preventing spread of disease, delay or slowing of disease progression, amelioration or palliation of the disease state, and remission (whether partial or total), whether detectable or undetectable.
"Treatment" can also mean prolonging survival as compared to expected survival if not receiving treatment. "Palliating" a disease means that the extent and/or undesirable clinical manifestations of a disease state are lessened and/or the time course of progression is slowed or lengthened, as compared to a situation without treatment. As is recognized by the skilled person, drugs employed as therapeutic agents can reduce the severity of a disease or physiological disorder, but need not abolish every manifestation of a given disease or physiological disorder to be regarded as a useful therapeutic agent. Thus, "treatment" with a therapeutically effective amount of the extract of O. stamineus leaves or a formulation comprising a therapeutically effective amount of the extract of O. stamineus leaves need not effect a complete cure, or eradicate every symptom or manifestation of a disease, to constitute a viable therapeutic agent.
[0232] The terms "inhibits", "reduces", "downregulates" or any variation of these terms, when used herein means any measurable decrease or complete inhibition to achieve a desired result.
[0233] "Standard of care" or "standard therapy" as used herein means a treatment that is accepted by medical experts as a recognized treatment for a certain type of disease and that is widely used by healthcare professionals. One standard of care or standard therapy for a certain disease or physiological disorder may not be the only standard of care or standard therapy for that disease or physiological disorder. Similarly, a "standard therapeutic agent" is one which is accepted by medical experts as a recognized therapeutic agent for a certain type of disease and that is widely used by healthcare professionals. One standard therapeutic agent for a certain disease or physiological disorder may not be the only standard therapeutic agent for that disease or physiological disorder.
[0234] "Adjuvant Therapy" is therapy given in addition to the primary or main therapy to maximize effectiveness of the primary or main therapy. The primary or main therapy can be, for example, surgery. Thus, adjuvant therapy is therapy provided after surgery if there remains a risk of occult disease. "Neoadjuvant therapy", on the other hand, is given prior to the main treatment. In the case of cancer, for example, neoadjuvant therapy is given mainly to reduce the size of a tumor(s) to facilitate effective surgery. The treatments
provided during neoadjuvant and adjuvant therapy can be different or the same.
Neoadjuvant or adjuvant therapy can be in combination with other therapeutic agents. The therapeutic agents can be standard therapeutic agents. The extract of the O. stamineus leaves can be administered as neoadjuvant or adjuvant therapy alone or in combination with other therapeutic agents.
[0235] "Factors" as used herein means endogenous bioactive molecules, which can include, without limitation, proteins, lipids, carbohydrates, glycoproteins, and glycolipids. The proteins include, without limitation, amino acid monomers, peptides, or polypeptides. The peptides and polypeptides can be linear or cyclic. The lipids include, without limitation, fatty acids, glycerolipids (e.g., triglyceride), phospholipids (e.g, phosphatidylcholine,
phosphatidylserine, phosphatidylethanolamine, phosphatidylinositol, phosphatidic acid), sphingolipids (e.g., glycosphingolipid, phosphosphingolipid (e.g., sphingomyelin), and sterol lipids (e.g., steroids and cholesterol). The carbohydrates include, without limitation, monosaccharides, disaccharides, polysaccharides, and lipopolysaccharides. The factors can function in a paracrine or autocrine manner. The factors can comprise pro-angiogenic factors, anti-angiogenic factors, cytokines, pro-apoptotic factors, anti-apoptotic factors, transcriptions factors, and combinations thereof. The cytokines can comprise chemokines, interferons, interleukins, lymphokines, tumor necrosis factor, and combinations thereof.
[0236] "Tumorigenic" as used herein means as capable of forming or tending to form tumors and refers to both malignant and benign tumors.
[0237] The term "normalization of the vasculature" or "vascular normalization" as used herein refers to a reversion of the abnormal vasculature observed with angiogenesis associated disorders to a substantially normal phenotype when treated with an anti- angiogenic inhibitor. In one embodiment, the anti-angiogenic inhibitor is the extract of O. stamineus leaves described herein.
METHOD OF MANUFACTURE OF THE EXTRACT
[0238] Extraction (as the term is pharmaceutically used) is the separation of medicinally active components in plant tissues using selective solvents. Such extraction techniques separate the soluble plant primary and secondary metabolites from the botanical and leave behind the insoluble cellular marc. The extract so obtained from plants is a complex mixture of primary and secondary metabolites comprising, without limitation, vitamins, essential amino acids, alkaloids, glycosides, terpenoids, flavonoids and lignans. The extracts can be in liquid or semisolid state or, after removing the solvent, in dry powder form, and can be further processed into formulations intended for enteral, parenteral, or topical use. The purpose of standardized extraction procedures is to obtain phytochemically consistent extracts with a defined proportion of therapeutically desired components and to eliminate unwanted material by treatment with a selective solvent or a different ratio of two or more solvents. The extract thus obtained, after standardization, can be used as an active pharmaceutical ingredient (API) in the form of tinctures or fluid extracts or further processed to be incorporated in any dosage form such as for example, immediate release dosage forms (oral or non-oral), modified release dosage forms (oral or non-oral), sublingual films, sublabial films, buccal films, ointments, gels, dendrimers, oral sprays, orally disintegrating tablets, lozenges, effervescent tablets, sublingual drops, lollipops, chewing gums, solid immediate release dosage forms (e.g. tablets, microspheres, granules, mini tablets, etc.), modified release dosage forms (e.g. tablets, microspheres, granules, mini tablets, etc.), capsules, gelcaps, pastilles, multiparticulates (e.g., microspheres, granules, powder), mini tablets, caplets, effervescent powders, hydrogels, syrups, medicated straws, dry-powder inhalers, nebulizers, metered dose inhalers, suppositories, vaginal tablets, vaginal creams, vaginal suppositories, vaginal rings, dermal patches, transdermal patches, ethosomes, niosomes, discosomes, phytosomes, liposomes, lotions, lip balms, creams, emulsions, topical sprays, nasal sprays, medicated shampoos, eye drops, injectables, topical emulsions, biodegradable microparticles, biodegradable microspheres, biodegradable nano- microspheres, nanoparticles, polymeric microparticles, polymeric nanoparticles, steroidal
nano microparticles, steroidal microparticles, silicon microneedles, and nanostructured lipid carriers.
[0239] The extract described herein is derived from a popular perennial medicinal herb of the genus Orthosiphon, which comprises 40 species found in tropical and subtropical Asia including Southern Africa and Madagascar (31). Crude extracts from various species of this genus are known for their medicinal properties. Accordingly, the extract described herein can be manufactured using the method described herein from any one or more of the species of Orthosiphon. In certain embodiments, the species of Orthosiphon is O.
adenocaulis, O. allenii, O. aristatus var. aristatus, O. biflorus, O. bullosus, O. cladotrichos, O. cuanzae, O. discolor, O. ellipticus, O. ferruginous, O. fruticosus, O. glandulosus, O.
hanningtonii, O. humbertii, O. incurvus, O. lanatus Doan, O. miserabilis, O. nigripunctatus, O. pallidus, O. parvifolius, O. pseudoaristatus, O. robustus, O. rubicundus Benth, O. rubicundus var. hainanensis, O. rubicundus var. rubicundus, O. sarmentosus, O. schimperi, O.
stamineus, O. thymiflorus, O. truncates, O. vernalis, O. violaceus, O. wattii, or any combination thereof. In certain embodiments, the extracts described herein can be manufactured from O. aristatus var. aristatus, O. pallidus, O. stamineus, O. thymiflorus, or any combination thereof. In one embodiment, the species is O. stamineus.
[0240] Briefly, in one embodiment, the method of manufacturing an extract of the leaves of O. stamineus, comprises: (a) contacting cleaned, dried and pulverized leaves of O. stamineus with a solvent comprising 1:1 (vol/vol) EtOH to water solution preheated to 60°C, wherein the solvent is moving in a first direction for a period of time, (b) continuing the extraction by directing the solvent in a second direction opposite to the first direction for a period of time equal to the time in (a), (c) alternating direction of solvent flow for a total time of 4-6 hrs, (d) filtering the solvent comprising extract through a filter, and (e) concentrating the filtered extract by evaporation of the solvent. In certain embodiments, the filtered and concentrated extract can be further processed by spray drying the extract to obtain granules.
[0241] Prior to subjecting the O. stamineus plant material to the extraction technique, the O. stamineus plant is cultivated and processed as follows. O. stamineus can be cultivated on farms under Good Agricultural Practice (GAP). The crop is cultivated under shade in a tropical climate with temperatures range from 21°C to 32°C, with humidity ranging from 82% to 86%. Although the entire plant can be used to manufacture the extract, the leaves are the preferred part of the plant and contain the highest concentration of the
pharmacologically active biomolecules. Leaves are harvested from plants about 3 months to 1 year old. Ideally, the leaves are harvested prior to the flowering stage during the vegetative stage. Plants grown in tissue culture environment or in greenhouse conditions can also be used.
[0242] Harvested leaves of O. stamineus are thoroughly cleaned by removing any sand pneumatically and any iron-containing material magnetically. The leaves are then washed thoroughly in deionized water and subsequently dried for a time sufficient to dry the leaves completely. Drying can be performed in a hot air oven, air-dried, or a combination of both drying methods can be used in no particular order. In at least one embodiment, the leaves are dried in a hot air oven for 24 to 48 hours at a temperature ranging from 35°C-50°C. Drying the leaves prevents microbial or fungal growth, particularly if the leaves are to be stored for later processing. The dried O. stamineus leaves are hygroscopic. Accordingly, if the
dried O. stamineus leaves are not to be processed immediately, the dried leaves should be stored under low humidity controlled conditions.
[0243] To maximize extraction of the pharmacologically active compounds, the cleaned and dried leaves are further processed by shredding and/or grinding mechanically the whole leaves to smaller dimensions using methods well known in the art (e.g., a grinding mill or toothed disc disintegrators). The smaller particles allow for an increase in the surface area exposed to the extraction solvent and hence maximize extraction of the pharmacologically active compounds. The processed material can be passed through a sieve or a series of sieves of gradually smaller pore size to obtain particles of uniform size. The processed leaves that do not pass through the sieve(s) can be subjected to multiple rounds of shredding and/or grinding to maximize the amount of leaves used for the extraction. In at least one embodiment, the size of the cleaned, dried, and processed O. stamineus leaves should be from 3mm - 5mm. In one embodiment, the size of the shredded leaves should not be less than 3mm.
[0244] The general techniques of medicinal plant extraction include maceration, infusion, percolation, digestion, decoction, distillation, hot continuous extraction (Soxhlet), aqueous-alcoholic extraction by fermentation, CCE, microwave-assisted extraction, ultrasound extraction (sonication), supercritical fluid extraction, and phytonic extraction (with hydrofluorocarbon solvents) or any combination thereof. In one embodiment, the pharmacologically active extract of O. stamineus is obtained using CCE technology. The extract of O. stamineus leaves obtained by CCE has a unique chemical fingerprint as determined by high performance liquid chromatography, and as described in detail below, and in the examples, has properties beneficial for the treatment of a variety of health disorders. Generally, in CCE, the material to be extracted is first finely shredded and/or ground to maximize surface area for extraction and flows in a direction (generally in the form of a fine slurry) opposite the direction of the preferred extraction solvent. The flow of solvent and flow of material to be extracted can be alternated multiple times to maximize the extraction. This countercurrent contact between the material to be extracted and the extraction solvent results in the gradual enrichment of the biologically active compounds in the solvent phase throughout the extraction process. Complete or almost complete extraction is thus possible when the quantities of solvent and material and their flow rates are optimized. The process is highly efficient, requiring little time and posing minimal risk from high temperature. Finally, sufficiently concentrated extract comes out at one end of the extractor while the marc falls out at the other end.
[0245] Any CCE apparatus can be used to manufacture the extract. In at least one embodiment, the extract of O. stamineus leaves is obtained using a DIG-MAZ®
Multifunctional Extraction System (Samtech Extraktionstechnik GmbH, Jagerzeile 34, Mannersdorf, Austria 2452). The solvent used is 1:1 (vol/vol) EtOH to water (50% EtOH). The ratio of the processed O. stamineus leaves to the 50% EtOH solvent can range from 1:10 to 1:20 (wt:vol). For example, in certain embodiments the ratio can be 1:10, 1:10.5, 1:11,
1:11.5, 1:12, 1:12.5, 1:13, 1:13.5, 1:14. 1:14.5, 1:15, 1:15.5, 1:16, 1:16.5, 1:17, 1:17.5, 1:18, 1:18.5, 1:19, 1:19.5 or 1:20 (wt:vol). In one embodiment, the ratio of the processed O. stamineus leaves to the 50% EtOH solvent is 1:10. In another embodiment, the ratio of the processed O. stamineus leaves to the 50% EtOH solvent is 1:20 (wt:vol). The size of the extraction system used will depend on the volume of extract desired and the extraction time
will vary depending on the temperature of the solvent. Thus, a longer extraction time is required when the solvent temperature is low. Conversely, a shorter extraction time is required when the solvent temperature is higher. In certain embodiments, the temperature of the solvent can range from 50°C - 70°C. In certain other embodiments, the temperature of the solvent can be 50°C, 55°C, 60°C, 65°C, or 70°C. In one embodiment, the temperature of the solvent is 60°C. In certain embodiments, the extraction time can be from 2hrs -12hrs (e.g., 2hr, 2.5hr, 3hr, 3.5hr, 4hr, 4.5hr, 5hr, 5.5hr, 6hr, 6.5hr, 7hr, 7.5hr, 8hr, 8.5hr, 9hr, 9.5hr, lOhr, 10.5hr, llhr, 11.5hr or 12hr). In certain other embodiments, the extraction time ranges from 4hr - 6 hr (e.g., 4hr, 4.5hr, 5hr, 5.5hr, or 6hr). In one embodiment, the extraction time is 6hrs. In one embodiment, the temperature of the solvent is 60°C and the extraction time is 4hr - 6hrs. In one embodiment, the temperature of the solvent is 60°C and the extraction time is 6hrs.ln certain embodiments, the solvent flow rate can be from 500L - 2000L per hour (e.g., 500L/hr, 600L/hr, 700L/hr, 800L/hr, 900L/hr, lOOOL/hr, HOOL/hr, 1200L/hr, 1300L/hr, 1400L/hr, 1500L/hr, 1600L/hr, 1700L/hr, 1800L/hr, 1900L/hr or 2000L/hr). In certain other embodiments, the solvent flow rate ranges from 500L/hr - lOOOL/hr (e.g., 500 L/hr, 600 L/hr, 700 L/hr, 800 L/hr, 900 L/hr, or 1000 L/hr). In one embodiment, the solvent flow rate is 800 L/hr.
[0246] Prior to removing the solvent, the extract is passed through a filter by means well known in the art. In certain embodiments, the permeability of the filter can range from 785 L/m2/min - 1275 L/m2/min (e.g., 785, 800, 825, 850, 875, 900, 925, 950, 975, 1000,
1025, 1050, 1075, 1100, 1125, 1150, 1175, 1200, 1225, 1250, or 1275 L/m2/min). In certain embodiments, the permeability of the filter can range from 850 - 1000 L/m2/min (e.g., 850, 875, 900, 925, 950, 975, 1000 L/m2/min). In certain embodiments, the permeability of the filter can be 925 L/m2/min. In certain embodiments, the filter is a Seitz® K700 filter from Pall Corporation (Port Washington, NY, USA). In certain embodiments, the number of layers of the filter can range from 1-9. In certain embodiments, the number of layers of the filter can be 9.
[0247] The solvent in the filtered extract can be removed by several methods well known in the art, such as for example, distillation, evaporation, spray drying, vacuum oven drying, fluid-bed drying or freeze drying (also known as lyophilization) or any combination thereof. The solvent can also be removed in stages depending on the volume of solvent to be evaporated. The different stages of evaporation can use different evaporating techniques. For example, in one embodiment, the solvent can be removed in a first step using an evaporator. The evaporator can be any type of evaporator (e.g., plate evaporator, falling film evaporator, thin film evaporator, forced circulation evaporator, circulation evaporator, fluidized bed evaporator, rising film evaporator, or stirrer evaporator). Plate vaporizers are used when high vaporising power is required. Depending on the intended use of the extract, a thin-film vaporiser can be used. For production of instant products that are dried with spray dryers, the concentration that is reached with the plate vaporiser can be sufficient. In one embodiment, the solvent in the extract is evaporated using a plate evaporator (Samtech Extraktionstechnik GmbH, Jagerzeile 34, Mannersdorf, Austria 2452) for 2 hours to recover about 40% solvent (the parameters for plate evaporator are, vacuum: -800 mbar at 60 °C). The extract from this step is further concentrated by using a thin film evaporator (Samtech Extraktionstechnik GmbH, Jagerzeile 34, Mannersdorf, Austria 2452)
for 2 hr to recover 80% of the remaining solvent (the parameters for thin film evaporator are, vacuum: -800 mbar at 60 °C).
[0248] The remaining solvent in the concentrated extract is finally evaporated and the extract converted to a powder using methods well known in the art. In certain
embodiments, the extract can be freeze dried or spray dried. In one embodiment, the extract is converted into powder form with consistent particle size distribution using a spray drying approach. Any commercially available spray dryer can be used (e.g., LabPlant SD-05 spray drier, Keison Products, Chelmsford, Essex CMl 3UP, England or a Labultima LU228 spray dryer, Labultima, Mumbai, 400 068 Maharashtra, India). In at least one embodiment, the extract is spray dried in a Labultima LU288 spray dryer with the following operating parameters: an air pressure of 1.4 bar, inlet temperature: 150 °C, outlet temperature: 130 °C, inlet high temperature: 200 °C, outlet high temperature: 180 °C, cool temp temperature: 100 °C, ID blower: 400 units, fD blower: 200 units, Feed pump speed: 30 ml/min, D Block: 1, Nozzle Pressure: 60 bar, Cycle: 999, and Vacuum: -400 mbar. The powder obtained can now be further processed for chemical analysis, used as described in the examples below, and/or manufactured into formulations for the treatment of a variety of physiological disorders. One embodiment of the method of manufacturing the extract of O. stamineus leaves is described in Example 1. CHEMICAL FINGERPRINT AND PHYTOCHEMICAL ANALYSIS OF THE EXTRACT OF O. stamineus
LEAVES
[0249] The extract of O. stamineus leaves obtained herein was analyzed for the quality and quantity of four (4) dominant compounds - RA, EUP, SIN, and TMF, known to be normally present in such extracts (26) (32) (33) (34) (35) (36), by HPLC, a technique well known in the art. Briefly, chromatographic analysis of the extract was carried out by reverse- phase HPLC on a Dionex-Ultimate® 3000 Rapid Separation LC system (Thermo Fisher Scientific Inc., USA). Chromatographic separation was performed using a reverse phase C18 column (Acclaim Polar Advantage II, USA) and a diode array detector (DAD) was used for the identification of peaks in the extract. The detection wavelength can be from 310-340 nm. In one embodiment, the detection wavelength was 320 nm. Identification of compounds in the extract was based on the retention time and the DAD spectrum against standards of EUP (3', 5-Dihydroxy-4',6,7-trimethoxyflavone), RA ((2 ?)-2-(((2"E")-3-(3,4-Dihydroxyphenyl)-l-oxo-2- propenyl))oxy)-3-(3,4-dihydroxyphenyl)propanoic acid), TMF, and SIN (3',4',5,6,7- pentamethoxy flavone). The presence of these four compounds in the extract was identified by comparison of their retention time values in the extract with those of the standards separated under identical conditions. In one embodiment, the chemical fingerprint of the extract, obtained by HPLC 320 nm, is described in Example 2. In one embodiment, the chemical fingerprint of the standards and extract obtained by HPLC at 320 nm is shown in Fig. 1A and IB respectively. The chemical fingerprint shown in Figure IB shows the presence of RA, EUP and SIN in the extract. However, TMF, one of the molecules that would otherwise be expected to be present was not detected. Thus, in certain embodiments, the extract of O. stamineus leaves comprises <0.2% (wt/wt) TMF (e.g., 0, 0.01, 0.02, 0.03, 0.04, 0.05, 0.06, 0.07, 0.08, 0.09, 0.1, 0.15, 0.16, 0.17, 0.18, 0.19 or 0.2%). In certain embodiments, the extract of O. stamineus leaves comprises <0.2% (wt/wt) TM F (e.g., 0, 0.01, 0.02, 0.03, 0.04, 0.05, 0.06, 0.07, 0.08, 0.09, 0.1, 0.15, 0.16, 0.17, 0.18, 0.19 or 0.195%). In certain
embodiments, the extract of O. stamineus leaves comprises, <0.1% (wt/wt) of the total extract of O. stamineus leaves TMF (e.g., 0, 0.01, 0.02, 0.03, 0.04, 0.05, 0.06, 0.07, 0.08, 0.09, or 0.1%). In certain embodiments, the extract of O. stamineus leaves comprises, <0.1% (wt/wt) of the total extract of O. stamineus leaves TMF (e.g., 0, 0.01, 0.02, 0.03, 0.04, 0.05, 0.06, 0.07, 0.08, 0.09, or 0.095%). TMF belongs to the methoxy flavone group and can be detected by UV in the range of 310 - 340 nm. In certain embodiments, TMF is not detectable in the extracts of O.s stamineus leaves by UV using HPLC between 310 - 340 nm. In one embodiment, TMF is not detectable by UV using HPLC at 320 nm in the chemical fingerprint of the extract of O. stamineus leaves,
[0250] In certain embodiments, A is present in the extract of O. stamineus leaves, by weight based on the total weight of the extract, from 3% - 8% (e.g., 3, 3.5, 4, 4.5, 5, 5.5, 6, 6.5, 7, 7.5, or 8%). In certain embodiments, the RA is present in the extract of O. stamineus leaves, by weight based on the total weight of the extract, from 4% - 7% (e.g., 4, 4.5, 5, 5.5, 6, 6.5, or 7%). In certain embodiments, the extract of O. stamineus leaves comprises, by weight based on the total weight of the extract, 6% ± 1.2% RA, i.e., from 4.8% - 7.2% (e.g., 4.8, 5, 5.2, 5.4, 5.6, 5.8, 6, 6.2, 6.4, 6.6, 6.8, 7, or 7.2%). In certain embodiments, the extract of O. stamineus leaves comprises, by weight based on the total weight of the extract, 6% ± 1.2% RA, i.e., from 4.8% - 7.2% (e.g., 4.8, 5, 5.2, 5.4, 5.6, 5.8, 6, 6.2, 6.4, 6.6, 6.8, 7, or 7.2%) and <0.2%, by weight based on the total weight of the extract, TMF. In certain
embodiments, the extract of O. stamineus leaves comprises, by weight based on the total weight of the extract, 6% ± 1.2% RA, i.e., from 4.8% - 7.2% (e.g., 4.8, 5, 5.2, 5.4, 5.6, 5.8, 6, 6.2, 6.4, 6.6, 6.8, 7, or 7.2%) and <0.2%, by weight based on the total weight of the extract, TM F. In certain embodiments, the extract of O. stamineus leaves comprises, by weight based on the total weight of the extract, 6% ± 1.2% RA, i.e., from 4.8% - 7.2% (e.g., 4.8, 5, 5.2, 5.4, 5.6, 5.8, 6, 6.2, 6.4, 6.6, 6.8, 7, or 7.2%) and <0.1%, by weight based on the total weight of the extract, TMF. In certain embodiments, the extract of O. stamineus leaves comprises, by weight based on the total weight of the extract, 6% ± 1.2% RA, i.e., from 4.8% - 7.2% (e.g., 4.8, 5, 5.2, 5.4, 5.6, 5.8, 6, 6.2, 6.4, 6.6, 6.8, 7, or 7.2%) and <0.1%, by weight based on the total weight of the extract, TMF.
[0251] In certain embodiments, the extract also comprises, 0.15% (wt/wt) EUP, and not less than 0.05% (wt/wt) SIN.
[0252] In one embodiment, the extract of O. stamineus leaves is standardized such that the amount of RA in the extract comprises, by weight based on the total weight of the extract, 6% ± 1.2% i.e., from 4.8% - 7.2% (e.g., 4.8, 5, 5.2, 5.4, 5.6, 5.8, 6, 6.2, 6.4, 6.6, 6.8, 7, or 7.2%). In one embodiment, the extract of O. stamineus leaves is standardized such that the amount of RA in the extract comprises, by weight based on the total weight of the extract, 6% ± 1.2% and <0.2%, by weight based on the total weight of the extract, TMF. In one embodiment, the extract of O. stamineus leaves is standardized such that the amount of RA in the extract comprises, by weight based on the total weight of the extract, 6% ± 1.2% and <0.2%, by weight based on the total weight of the extract, TMF. In one embodiment, the extract of O. stamineus leaves is standardized such that the amount of RA in the extract comprises, by weight based on the total weight of the extract, 6% ± 1.2% and <0.1%, by weight based on the total weight of the extract, TMF. In one embodiment, the extract of O. stamineus leaves is standardized such that the amount of RA in the extract comprises, by weight based on the total weight of the extract, 6% ± 1.2% and <0.1%, by weight based on
the total weight of the extract, TMF. Certain batches of O. stamineus leaves can provide an extract comprising greater than 7.2% (wt/wt) A and certain other batches can provide an extract less than 4.8% (wt/wt) RA. Such extracts are not discarded, but stored for future use in adjusting the levels of RA in subsequent extracts to between 4.8% - 7.2% (wt/wt). For example, in extracts <4.8% (wt/wt) RA, an extract having >4.8% (wt/wt) RA is added to the extract comprising <4.8% (wt/wt) RA, such that the %(wt/wt) RA is adjusted to between 4.8% - 7.2% (wt/wt). Conversely, in extracts >7.2% (wt/wt) RA, an extract having <7.2% (wt/wt) RA is added to the extract comprising >7.2% (wt/wt) RA, such that the %(wt/wt) RA is adjusted to between 4.8% - 7.2% (wt/wt).
[0253] In one embodiment, detection by HPLC was optimized at 320 nm absorbance to detect RA, TMF, EUP and SIN. However, the skilled person will appreciate that this does not exclude the presence of other phytochemical compounds in the extract. Accordingly, the extract can comprise, without limitation, tetramethyl scutellarein, salvigenin, cirsimaritin, pilloin, rhamnazin, trimethylapigenin, tetramethyl luteolin, orthosiphonone, orthosiphonone B, orthosiphol A, orthosiphol B, orthosiphol F, orthosiphol G, orthosiphol H, neoorthosiphols, staminol A, orthochromene A, methylripariochromene A, acetovaillochromene, β-elemene, β-caryophyllene, a-humulene, β-caryophyllene oxide, Can-2-one, Palmitic acid, ladanein, vomifoliol, 7,3,4-tri-O-methylluteolin, scutellareintetramethyl- ether, caffeic acid, cichoric acid 2, 3-dicaffeoyltartaric acid, acetic acid (3-hydroxy-7-isopropenyl-l, 4a-dimethyl- octahydronaphthalen-2-yl) ester, dimethyl-4-(l-methylethylidene)-2,4,6,7,8,8a-hexahydro- 5(lH)-azulenone, anthracene, 9-(2-propenyl), 2-propen-l-one, 1,3-diphenyl, 2-amino-2-oxo- acetic acid N-(3,4-dimethylphenyl) ethyl ester, β-Elemene, l-Octen-3-ol, β-Carryophyllene, a-Humulene, β-Bourbene, Caryophyllene oxide, β- Pinene, Phenylacetaldehyde, Decanal, δ- Elemene, 1,8-Cineol, 4-Heptenal, Isomenthone, Camphene, cis-2-Octenal, 3-Octanol, Limonene, 2-Pentenyl furane, Hexanal, Naphtalene, Benzaldehyde, trans 2-Hexanal,
Heptenal, trans cis-Octa-3-5- dien-2-one, Methyl Chavicol, a-Pinene, Tridecan, p-Cymene, Camphor, 1- Methylnaphtalene, a-Muniolene, trans trans-Octa-3-5-dien-2-one, 2- Amylfurane, Menthone, Carvone, Cittonellol, δ-Cadipene, trans-2-(cis)-6- Nonadienale, Methyleugenol, a-Gubebene, Geranylacetane, δ-Terpineol, Acetophenone, trans- Anethol, Germacrene D, β-Cyclocitral, cis-Linalooloxide, Undecan, Bornyl Acetate, 2-
Methylnapthalene, β-lonone, a-Copaene, Damascenone, Dehydroionone, Borneol,
Dodecane, Eugenol, Linalool, trans-Linalooloxide, Perillen, Safranal,
Hexahydrofamesylacetone, Hexan-l-ol,2,6,6-Trimethyl-2-cyclohexe-l,4-dione,
Isobornylacetate, trans-Deca-2,4-dienal, cis-Caryophylene, Germacrene, cis- 3-Hexen-l-o, and combinations thereof.
[0254] In one embodiment, a phytochemical analysis, was conducted on the standardized extract to determine the total polysaccharide, glycosaponin, phenolic, flavonoid, phospholipids, and protein content by methods well known in the art. In certain embodiments, the polysaccharides can be present from 2% - 4% (wt/wt) (e.g 2, 2.1, 2.2, 2.3, 2.4, 2.5, 2.6, 2.7, 2.8, 2.9, 3, 3.1, 3.2, 3.3, 3.4, 3.5, 3.6, 3.7, 3.8, 3.9 or 4%) of the total extract. In certain embodiments, the polysaccharides can be present from 2.8% - 3.2% (wt/wt) (e.g., 2.8, 2.9, 3, 3.1, or 3.2%) of the total extract. In certain other embodiments, the
polysaccharides can be present at 3%(wt/wt) of the total extract. In certain embodiments, the glycosaponins can be present from 25% - 40% (wt/wt) (e.g., 25, 26, 27, 28, 29, 30, 31, 32, 33, 34, 35, 36, 37, 38, 39, 40, 41, 42, 43, 44, or 45%) of the total extract. In certain
embodiments, the glycosaponins can be present from 28% - 36% (wt/wt) (e.g., 28, 28.5, 29, 29.5, 30, 30.5, 31, 31.5, 32, 32.5, 33, 33.5, 34, 34.5, 35, 35.5 or 36%) (wt/wt) of the total extract. In certain embodiments, the glycosaponins can be present at 32% (wt/wt) of the total extract. In certain embodiments, the phenolics comprising the extract can be present from 32% - 39% (wt/wt) (e.g., 32, 32.5, 33, 33.5, 34, 34.5, 35, 35.5, 36, 36.5, 37, 37.5, 38, 38.5 or 39%) of the total extract. In certain embodiments, the phenolics can be present from 35% - 39% (wt/wt) (e.g., 35, 35.5, 36, 36.5, 37, 37.5, 38, 38.5 or 39%) of the total extract. In certain embodiments, the phenolics can be present at 37% (wt/wt) of the total extract. In certain embodiments, the flavonoids can be present from 5% -8% (wt/wt) (e.g., 5, 5.5, 6, 6.5, 7, 7.5 or 8%) of the total extract. In certain embodiments, the flavonoids can be present from 6% - 7% (wt/wt) (e.g., 6.1, 6.2, 6.3, 6.4, 6.5, 6.6, 6.7, 6.8, 6.9, or 7%) of the total extract. In certain embodiments, the flavonoids can be present at 6.6% of the total extract. In certain embodiments, the phospholipids comprising the extract can be present from 0.3% - 0.6% (wt/wt) (e.g., 0.3, 0.35, 0.4, 0.45, 0.5, 0.55, or 0.6%) of the total extract. In certain embodiments, the phospholipids can be present from 0.35% - 0.48% (wt/wt) (e.g., 0.35,
0.36, 0.37, 0.38, 0.39, 0.4, 0.41, 0.42, 0.43, 0.44, 0.45, 0.46, 0.47, or 0.48%) of the total extract. In certain embodiments, the phospholipids can be present at 0.44% (wt/wt) of the total extract. In certain embodiments, the total protein content (including free amino acids) in the extract can be present, by weight based on the total weight of the extract, <14% (e.g., 0, 0.5, 1, 1.5, 2, 2.5, 3, 3.5, 4, 4.5, 5, 5.5, 6, 6.5, 7, 7.5, 8, 8.5, 9, 9.5, 10, 10.5, 11, 11.5, 12, 12.5, 13, 13.5, or 14%). In certain embodiments, the total protein content in the extract can be present <12.5% (wt/wt) (e.g., 0, 0.5, 1, 1.5, 2, 2.5, 3, 3.5, 4, 4.5, 5, 5.5, 6, 6.5, 7, 7.5, 8, 8.5, 9, 9.5, 10, 10.5, 11, 11.5, 12, or 12.5%) of the total extract. In certain embodiments, the total protein content can be present from 11.5% - 12.5% (wt/wt) (e.g., 11.5, 11.6, 11.7, 11.8, 11.9, 12, 12.1, 12.2, 12.3, 12.4 or 12.5%) of the total extract. In certain embodiments, the total protein content can be present at 12% (wt/wt) of the total extract. In certain other embodiments, the total protein content can be <12% (wt/wt) of the total extract (e.g., 0, 0.5,
1, 1.5, 2, 2.5, 3, 3.5, 4, 4.5, 5, 5.5, 6, 6.5, 7, 7.5, 8, 8.5, 9, 9.5, 10, 10.5, 11, 11.5, 11.6, 11.7, 11.8, or 11.9%). In one embodiment, the chemical fingerprint and phytochemical profile of the extract of O. stamineus leaves is described in Examples 2 and 3 respectively.
PROPERTIES OF THE EXTRACT
[0255] Some of the natural compounds comprising extracts of O. stamineus have been known to demonstrate health benefits individually. The extract of O. stamineus leaves described herein comprises combinations of natural compounds, that although can be present at low molar concentrations, exhibit a potent synergistic enhancement of their individual efficacies in the treatment of a variety of diseases and health disorders. Moreover, the art has acknowledged that not all plant phytochemicals are effective medicines. This is particularly true for angiogenesis associated disorders (37) (38) (39) (40). Accordingly, the absence, or presence at very low levels of certain phytochemical compounds, in
standardized plant extracts, would be beneficial in the treatment of certain diseases.
[0256] For example, TMF is a known flavonoid. The best-described property of almost every flavonoid is their capacity to act as antioxidants, which function to protect the body against reactive oxygen species ( OS) (37). While it has become a matter of conventional wisdom in popular culture that raising antioxidant levels, especially by consuming over-the-
counter antioxidant supplements, improves overall health and keeps certain physiological disorders, such as cancer, at bay, there is mounting evidence that not all antioxidants are beneficial, and in fact, certain antioxidants can accelerate cancer progression (38). As described herein, TM F has the least anti-angiogenic activity in extracts of O. stamineus leaves, and it is believed, without being held to any one theory, that TMF can even function as a pro-angiogenic factor in certain angiogenesis associated disorders. Certain plant proteins can also contribute to the progression of certain physiological disorders, including cancer (39) (40). Thus, prior art extracts of O. stamineus comprising these phytochemicals can promote progression of certain physiological disorders. It would therefore be beneficial to obtain an extract of O. stamineus that is very low or is free of such compounds. In certain embodiments, the extract of O. stamineus leaves described herein comprises <0.2% (wt/wt) of TMF and <14% (wt/wt) total protein (including free amino acids). In certain embodiments, the extract of O. stamineus leaves described herein comprises <0.2% (wt/wt) of TMF and <14% (wt/wt) total protein (including free amino acids). In certain embodiments, the extract of O. stamineus leaves described herein comprises <0.1% (wt/wt) of TMF and <14% (wt/w) total protein (including free amino acids). In certain embodiments, the extract of O.
stamineus leaves described herein comprises <0.1% (wt/wt) of TMF and <14% (wt/w) total protein (including free amino acids).
[0257] As described below and demonstrated by the following examples, the extract of O. stamineus leaves has a variety of activities that can be beneficial for the treatment of a variety of physiological disorders. In one embodiment, the extract of O. stamineus leaves has an anti-angiogenic, anti-inflammatory, antihypertensive, blood glucose lowering, antioxidant and/or neuroprotective activity.
[0258] Angiogenesis is the sprouting of new capillary blood vessels from preexisting blood vessels and involves recruitment of associated supporting cells to different parts of the newly formed vasculature. In healthy adult subjects, angiogenesis is dormant, except during wound healing (41) (42), hair growth (43), the menstrual cycle (44), and during embryogenesis. Angiogenesis is a complex process and is characterized by a series of events, which include the proliferation and migration of endothelial cells, remodeling of the extracellular matrix, capillary formation, and recruitment of surrounding structures and cells for maintenance and proper functioning of the newly formed capillary network (45) (46). Angiogenesis is under the control of both angiogenesis growth factors (also referred to herein as "pro-angiogenic factors") and angiogenesis inhibitors (also referred to herein as "anti-angiogenic factors"). These factors include, for example, integrins, chemokines, angiopoietins, oxygen sensing agents, junctional molecules and endogenous inhibitors, all of which are maintained at a perfect balance in a healthy adult subject. When more pro- angiogenic factors are produced than anti-angiogenic factors, the scales are tipped in favor of new blood vessel growth, which can lead to an angiogenesis associated disorder in an otherwise healthy subject. Abnormal blood vessel growth is the hallmark of many angiogenesis associated disorders, such as for example cancer, retinopathy and
inflammation. In cancer, any increase in tumor size must be preceded by an increase in the vascular supply, to deliver nutrients and oxygen to the tumor. For example, in cancer, detectable solid tumors (i.e., tumors over 2 mm in diameter) subvert angiogenesis by secreting pro-angiogenic factors, which coax the sprouting of new blood vessels from preexisting blood vessels, and promote their subsequent growth and development to form
new vasculature that will support the tumor's continued growth and eventual metastasis (47). Thus, anti-angiogenic approaches to inhibiting any one or more of the events contributing to angiogenesis could offer therapeutic opportunities for the treatment of angiogenesis associated disorders.
[0259] One of the steps in angiogenesis includes the ability of the angiogenic source to promote sprouting of new blood vessels (which includes the proliferation, migration, and formation of new endothelial cells into capillaries). In one embodiment, the extract of O. stamineus leaves can substantially inhibit the sprouting of new blood vessels from preexisting blood vessels (this process is also referred to herein as "neovascularization") in a subject in need thereof. In one embodiment, the ability of the extract of O. stamineus to inhibit this step in angiogenesis was demonstrated by the ability of the extract to inhibit sprouting of microvessels from everted rat aortas as described in Examples 4 and 15. Briefly, the ability of the extract of O. stamineus leaves and the extent to which the extract can inhibit sprouting of new blood vessels from preexisting blood vessels was assessed in an ex vivo rat aortic ring assay. In this assay, rings of everted rat aorta are exposed to a three- dimensional matrix containing angiogenic factors and the effect of the extract of O.
stamineus leaves is evaluated by quantifying the extent to which microvessels sprout from the exposed endothelium of the everted rat aorta.
[0260] The experiment was first carried out with the extract of O. stamineus leaves as described herein at 100μg/mL and compared to extracts of O. stamineus leaves obtained by the maceration technique (26) with water, 100% methanol, 50% methanol, 100% EtOH, A and suramin (positive control). The result of this comparative experiment is shown in Example 4 (Table 4) which shows the potency of the different maceration extracts on the inhibition of microvessels from the rat aortic ring in comparison to the effect of an extract of O. stamineus leaves manufactured as described in Example 1.
[0261] The above experiment was then followed with evaluating five different concentrations of the extract of O. stamineus leaves manufactured as described herein to obtain the IC5o value for the anti-angiogenic activity. The results are shown in Example 4 (Table 5). Example 15 (Table 27) illustrates the effectivness of an unformulated extract of O. stamineus leaves and said extract formulated as nano-liposomes on neovascularization.
[0262] In normal healthy subjects, the vascular endothelium, which lines the inside of blood vessels, is in a quiescent state and has turnover rates of months to years and proliferates only upon angiogenic activation. The proliferation and migration of new endothelial cells, which form the lining of blood vessels, is a necessary event in angiogenesis. It is hoped that by blocking the formation of new blood vessels through drugs that act on endothelial cells, it can be possible to block angiogenesis and treat angiogenesis associated disorders. In one embodiment, an extract extract of O. stamineus leaves can inhibit the proliferation and/or migration of endothelial cells in a subject in need thereof. In one embodiment, the effectiveness of such an extract of O. stamineus leaves in inhibiting the proliferation and/or migration of human endothelial cells and cancer cells was demonstrated in Examples 5 (Table 6), 6 (Table 7), and 15 (Table 29).
[0263] In one embodiment, an extract of O. stamineus leaves can inhibit invasiveness of cancer cells. Tissue invasion and metastasis is one of the hallmarks of cancer, which requires migration of cancerous cells from the tumor to form colonies at a distant site. In
one embodiment, the extract of O. stamineus leaves can inhibit or suppress the invasive property of cancer cells as demonstrated in Example 7 (Table 8) and Example 15 (Table 31).
[0264] It is not enough that angiogenesis requires the proliferation and migration of endothelial cells towards the angiogenic source. These newly formed and migrating endothelial cells must also be able to shape themselves into three dimensional structures that in the early stages of angiogenesis resemble capillaries. The formation of these three- dimensional capillary-like structures (referred to in the art as "tubes") can be reproduced in vitro by methods well known in the art (48) (49). These methods allow the efficacy of drugs to inhibit capillary-like tube formation, one of the steps in angiogenesis, to be tested. In one embodiment, the extract of O. stamineus leaves can inhibit capillary formation by endothelial cells in a subject in need thereof. In one embodiment, the effectiveness of the extract in inhibiting capillary formation by endothelial cells was tested on VEGF induced capillary-like tube formation using a HUVEC cell line as demonstrated in Example 8 (Table 9) and Example 15 (Table 32).
[0265] In one embodiment, the extract of O. stamineus leaves can inhibit
neovascularization in a subject in need thereof. The ability of the extract of O. stamineus leaves to inhibit neovascularization in vivo was demonstrated using a chick embryo chorioallantoic membrane (CAM) assay as described in Example 9. The effect of the extract on neovascularization as determined by the CAM assay is shown in Table 10.
[0266] The multicellular spheroid tumour model ("hanging drop assay") was first established by (50). The aim of this assay was to evaluate anti-angiogenic and
antitumorigenic property of an extract of O. stamineus leaves using multicellular spheroids as a 3D in vitro tumour model of human colorectal cancer (HCT-116) and human lung adenocarcinoma (A549) and to assess penetration efficiency of the extract into the 3D in vitro tumour model (51) (52). Multicellular spheroids are useful as in vitro avascular tumor models to study cytotoxicity of chemotherapeutic agents. Formation of 3D in vitro tumour spheroid models of cancerous cells, without addition of any artificial substrate to support cell adhesion, is prefered over conventional 2D monolayer cell cultures, where it closely mimics development of tumors in vivo especially with respect to microenvironmental conditions, such as hypoxia and nutritional depletion.
[0267] In one embodiment, the extract of O. stamineus leaves can inhibit aggregation of cancer cells to form solid tumors in a subject in need thereof. The anti-tumorigenicity property of the extract of O. stamineus leaves was evaluated in comparison to A and a negative control using a spheroid assay as demonstrated in Example 10 and Example 15. This assay allows cells to aggregate and sediment in the cultures due to the applied gravitational force on the suspended cells. Subsequently, the suspended cells form spheroid shaped solid aggregates within 72 h, mimicking solid tumor formation. After complete sedimentation, the cellular aggregates are harvested and transferred into pre-coated agar plates. Fig. 2 shows the effect of the extract on spheroid tumor development of a human colorectal cells.
Example 15 (Table 30) shows the effect of the extract on spheroid tumor development of human lung adenocarcinoma cells.
[0268] Xenograft (the grafting of tissue from one species to an unlike species) models of human cancer are an important tool in the screening and evaluation of candidates for new anticancer agents. In this model, human tumor cells are transplanted, either under the skin (ectopic) or into the organ type in which the tumor originated (orthotopic), into
immunocompromised mice that do not reject human cells. For example, the xenograft will be readily accepted by athymic nude mice, severely compromised immunodeficient (SCID) mice, or other immunocompromised mice (53). For example, in an ectopic tumor xenograft model, the human cancer cells are injected under the skin of an immunocompromised mouse. In an orthotopic tumor xenograft model, for example, human colon cancer cells are injected directly into the colon and human breast cancer cells are injected directly into the breast of immunocompromised mice.
[0269] In one embodiment, an extract of O. stamineus leaves can inhibit growth tumors in a subject in need thereof. In one embodiment, the anti-angiogenic activity of such an extract of O. stamineus leaves was tested in vivo for its ability to inhibit growth of a human ectopic xenograft colorectal tumor in nude mice in a short term 28-day model. The in vivo antitumor activity of such an extract of O. stamineus leaves was evaluated by implanting human colorectal cancer cells subcutaneously in NCR nu/nu nude mice as demonstrated in Example 11. The effect of such an extract of O. stamineus leaves on growth of human colorectal tumors and body weight is presented in Tables 11 and 12 respectively.
[0270] The effect of an extract of O. stamineus leaves on the long-term survival was investigated in athymic nude mice bearing the human colorectal tumors as demonstrated in Example 12. Table 13 shows the long-term survival of animals treated with an extract of O. stamineus leaves versus RA and imatinib on xenograft ectopic human colorectal tumor growth. Thus, in one embodiment, the long-term administration of the extract increased the survival of animals treated with the extract.
[0271] In one embodiment, the extract of O. stamineus can inhibit human colorectal cancer growth in vivo in a dose dependent manner in a subject in need thereof. The antitumor effect of the extract of O. stamineus leaves on an orthotopic model of human colorectal cancer cells (HCT-116) injected into the cecal wall of nude mice was evaluated based on the intensity of two fluorescent imaging agents: 1) AngioSense® 750 - an in vivo blood pool imaging agent that is a marker for blood vessel density, enabling imaging of blood vessels and angiogenesis in animal tumor models, and 2) HypoxiSense® 680 - a fluorescent imaging agent that detects tumor cell surface expression of CA9, which is increased in hypoxic regions of many tumors. This embodiment is demonstrated in Example 13. The effect of the extract of O. stamineus leaves on tumor vascularization and tumor growth is shown Table 14.
[0272] Further, Table 15 shows the effect of the various treatments on the levels of several blood markers. ALT and AST levels were significantly lower in all treated groups compared to the control group. The higher levels of ALT and AST in the untreated control group can be due to the metastasis of the tumor to the liver. Total protein, albumin, globulin, the albumin to globulin ratio, ALP, total bilirubin, and GGT levels were not statistically significantly different among all groups (P > 0.05).
[0273] In one embodiment, pre-treatment of the extract of O. stamineus leaves in a subject in need thereof (e.g., a subject that may be predisposed to an angiogenesis associated disorder, such as for example cancer) can inhibit or suppress establishment of tumors and their subsequent growth, progression and metastasis in the subject. The ability of the extract of O. stamineus leaves to inhibit or suppress establishment and growth of tumors and their subsequent progression and metastasis was evaluated by pretreating mice at two different doses of the extract of O. stamineus leaves for two-weeks prior to
implantation of human colorectal cancer cells as demonstrated in Example 14. Human colorectal cancer cells were subsequently implanted ectopically and allowed to form tumors for 28 days. At the end of the 28-day period, tumor volume was assessed and histological analysis was conducted on tumors grown in untreated animals and animals pre-treated with the extract of the O. stamineus leaves. The gross morphology of the excised tumors from untreated animals compared to pretreated animals is shown in Fig. 4A - C. Tumor volume of tumors excised from untreated and pretreated animals is shown in Table 16. The body weight of the animals from time of pretreatment to time of tumor excision is shown in Table 17. Fig. 5 shows cross-sections of the tumors stained with haematoxylin/eosin.
[0274] In one embodiment, an extract of O. stamineus leaves can inhibit growth of lung cancer in a subject in need thereof. In one embodiment, the anti-angiogenic activity of the extract of O. stamineus leaves formulated as a liposomal drug delivery system or unformulated extract was evaluated in-vivo in nude mice in a short term 28-day model for its ability to inhibit growth of human lung adenocarcinoma. The in-vivo antitumor activity of formulated and unformulated extract was demonstrated by implanting human lung adenocarcinoma cells ectopically in NCR nu/nu nude mice as demonstrated in Example 15. In one embodiment, the formulated and unformulated extract of O. stamineus leaves exhibits a dose-dependent inhibition of human lung cancer while maintaining body weight over the treatment period for the various treatments. The effect of the formulated and unformulated extract of O. stamineus leaves on growth of human lung cancer in-vivo is presented in Tables 34-36. The change in weight of animals over the treatment period is shown in Table 37. Fig. 6 shows the gross morphology of tumors excised from the untreated and treated mice. Vascularization is apparent in tumors from untreated mice (Fig. 6A) with a dose dependent decrease in vascularization and a corresponding decrease in tumor size in mice treated with the formulated (Fig. 6F-H) or unformulated extract of O. stamineus leaves (Fig. 6C-E).
[0275] The imbalance in pro- and anti-angiogenic factors, and their subsequent abnormal signaling in angiogenesis associated disorders creates an abnormal vasculature that is characterized by dilated, tortuous and hyperpermeable blood vessels (54) (55).
Tortuosity of retinal and conjunctival blood vessels has been associated with angiogenesis, hypertension, atherosclerosis, diabetes, retinopathies (e.g., diabetic retinopathy, retinal ischemia, and AMD) amongst other angiogenesis associated disorders (55) (56) (57). It has been postulated that the physiological manifestations of these abnormalities, together with the resulting microenvironment created by the abnormal vasculature, favours the growth and progression of these angiogenesis associated disorders (54).
[0276] The abnormal vasculature associated with angiogenesis associated disorders results in poor delivery of therapeutic drugs and hence results in poor therapeutic outcomes. With respect to cancers, the abnormal vasculature can lead to a reduction in the efficacy of chemotherapy, immunotherapy and radiotherapy (54). However, experiments with anti-angiogenic inhibitors, such as for example inhibitors of VEGF (VEGF is believed to be the primary driver of angiogenesis) have shown that the abnormal vasculature associated with angiogenesis associated disorders, especially tumors, can be made to revert to a more normal phenotype (54). Thus, normalization of the vasculature, by treatment with anti- angiogenic drugs can reduce hypoxia and hyperpermeability, improve the efficacy of radiotherapy, chemotherapy, immunotherapy, and reduce metastasis of tumors.
[0277] In one embodiment, the extract of O. stamineus leaves can promote vascular normalization for the treatment of angiogenesis-associated disorders. In one embodiment, the extract of O. stamineus leaves can promote vascular normalization for the treatment of diabetic retinopathy. In one embodiment, the extract of O. stamineus leaves can promote vascular normalization for the treatment of AMD. In one embodiment, the extract of O. stamineus leaves can treat diabetic retinopathy in a subject in need thereof. In one embodiment, the extract of O. stamineus leaves can treat retinal ischemia in a subject in need thereof. In one embodiment, the extract of O. stamineus leaves can treat AMD in a subject in need thereof. In one embodiment, the ability of the extract of O. stamineus leaves to revert blood vessel tortuosity to a substantially normal phenotype, and thus promote vascular normalization is demonstrated in Example 16 and shown in Fig. 7. This example, which utilizes a rat diabetic retinopathy model, demonstrates the ability of an extract of O. stamineus leaves to treat diabetic retinopathy by substantially normalizing the retinal vasculature in diabetic rats.
[0278] In one embodiment, the ability of the extract to treat retinal ischemia is demonstrated in Example 16 in-vitro (Table 39) and in-vivo (Table 40).
[0279] Regulation of angiogenesis is a complex, dynamic process, often involving multiple proteins and cellular pathways. Positive and negative feedback loops, pleiotropic effects and redundant functions, spatial and temporal expression of or synergistic interactions between multiple pro- and anti-angiogenic factors, are common mechanisms modulating the effects of angiogenesis. Thus, abnormal angiogenesis is not the result of a single molecular target or cellular pathway that is dysregulated. It is believed, without being held to any one theory, that the multi-component extract of O. stamineus leaves synergistically affects multiple targets to promote an anti-angiogenic outcome. The synergistic effect of the extract of O. stamineus leaves on the expression of a select number of factors, some of which are chosen from pro- and anti-angiogenic factors, was determined by treating human endothelial cells with the extract of O. stamineus leaves, RA, EUP, SIN and TM F, and evaluating the levels of expression of the factors using an array of antibodies to the factors in comparison to untreated cells. An example of this embodiment is described in Example 17. The result of this analysis is shown in Table 41, which shows that the anti- angiogenic activity of the extract of O. stamineus leaves has the following order in comparison to RA, SIN, EUP, and TM F:
RA > extract of O. stamineus leaves > SIN > EUP > TM F
[0280] In one embodiment, the extract of O. stamineus leaves comprises <0.2% TMF. In certain other embodiments, the extract of O. stamineus leaves comprises <0.2% TMF. In certain other embodiments, the extract of O. stamineus leaves comprises <0.1% TMF. In certain other embodiments, the extract of O. stamineus leaves comprises <0.1% TMF. In certain embodiments, the extract of O. stamineus leaves is free of TMF. As shown herein, TM F by itself has the least overall anti-angiogenic activity when evaluated for the pro- and anti-angiogenic factors shown in Table 41. The skilled person will appreciate that the pro- and anti-angiogenic factors in Table 41 are not exhaustive. It is believed, without being held to any one theory, that TMF can demonstrate pro-angiogenic activity depending on the nature of the physiological disorder. For example, TMF has been reported to increase expression of TIMP-1, a tissue inhibitor of metalloproteinases (58). Increased expression of TIMP-1 has been found to be associated with worse prognosis for certain tumors, such as
laryngeal carcinoma or melanoma (59) (60). Accordingly, extracts of O. stamineus leaves comprising <0.2% (wt/wt), <0.2% (wt/wt), <0.1% (wt/wt), or <0.1% (wt/wt) are
advantageous over prior extracts comprising high levels of TM F, which can promote certain angiogenesis associated disorders, such as certain cancers.
[0281] In one embodiment, the extract of O. stamineus leaves can inhibit the expression and/or activity of CA9. In cancer, the tumor microenvironment contributes substantially to the progression of the disease. Despite the ability of tumors to promote the development of a vasculature for the delivery of the much-needed nutrients and oxygen to the tumor for its continued growth, the metabolic demands of the tumor generate a microenvironment with insufficient oxygen supply. One of the most significant adaptations by cancer cells to this hypoxic environment is to shift to anaerobic glycolysis, which results in excessive amounts of lactate, protons, and CO2, to keep up with the tumors' energy demands (61). To maintain optimal intracellular pH, these by-products must be excreted from the cell. The levels of oxygen within a cell are primarily detected by HIF1, which comprises a regulatory ot-subunit and a DNA binding β-subunit (62). The hypoxic environment activates HIF1, which in turn increases expression of several key proteins related to angiogenesis and glycolysis, including MCT, LDH PDK, HK 1/2; GLUT-1, and CA9 (63). The increased metabolic rate of cancer cells generates high levels of intracellular H+- ions, which must be eliminated to maintain an intracellular pH above 7, a prerequisite for cell growth and survival. The proteins expressed in response to HIFl-a assist in eliminating excess intracellular H+-ions, thus increasing intracellular pH to above 7.
[0282] CA9 is most widely expressed in response to hypoxia in tumors and its expression is often correlated with aggressive phenotypes (61). CA9 is a transmembrane isoform of CA and is located on the extracellular surface of the cell with an extracellular- facing catalytic site (63). One method used by cancer cells to prevent the decrease in the intracellular pH is to titrate the H+-ions generated with intracellular HCO3" forming CO2. The CO2 formed, which is membrane permeable, exits the cell and is hydrated by the catalytic activity of CA9 to form H+-ions and HCO3". The HCO3" is pumped back into the cell via a Na+ driven bicarbonate co-transport process (NBC), thereby replenishing intracellular HCO3". This process of titrating intracellular HCX with metabolically generated H+-ions is repeated to eliminate excess intracellular H+-ions and reduce intracellular acidity. Thus, HCO3" cycles at the cell membrane resulting in acidification of the extracellular environment of the tumor due to the deposition of H+-ions from the catalytic breakdown of CO2 by CA9. It is believed that this process achieves two critical steps in the tumor's survival: 1) the acidification of the tumor's extracellular environment, which aids in the breakdown and remodeling of the extracellular matrix, and in turn assists in the neovascularization process and metastasis of the tumor (61) and, 2) intracellular pH of the tumor cells is maintained at above 7, a prerequisite for the tumor's growth and survival. Accordingly, the significant role played by CA9 in tumorigenesis and maintenance of the tumor's pH balance has made it an important therapeutic target for cancer treatment (61) (63).
[0283] In one embodiment, the extract of O. stamineus leaves can inhibit the activity and/or expression of CA9 in a dose dependent manner. It is believed, without being held to any one theory, that the inhibition and/or down-regulation of the activity and/or expression of CA9 by the extract of O. stamineus leaves can decrease a cancer cell's intracellular pH and prevent acidification of the tumor's microenvironment thereby reducing the tumor's
potential to survive, grow, and eventually metastasize. One embodiment for evaluating the ability of the extract of O. stamineus leaves in inhibiting and/or downregulating the activity and/or expression of CA9 is demonstrated in Example 18. The results of this experiment are shown in Table 42.
[0284] Drug resistance is one of the major causes of ineffective chemotherapy in cancer patients. The primary mechanism for this resistance is due to the ability of cancer cells to prevent intracellular accumulation of chemotherapeutic agents and exert its effects by actively expelling the chemotherapeutic agent from inside the cell via transmembrane transport proteins (64) (65). Cancer cells can develop MDR during the course of
chemotherapy not only to a primary chemotherapeutic agent, making the chemotherapeutic agent ineffective for continued treatment, but also to other chemotherapeutic and/or pharmaceutical agents that are unrelated to the primary chemotherapeutic. This type of resistance has been referred to as "Multidrug Resistance" (MDR).
[0285] MDR is due to several transmembrane transport proteins that function as pumps (effluxers) and extrude toxins and drugs out of the cell (66). The transmembrane transport proteins identified in MDR belong to the ABC family of proteins (64) (65) (66) (67), which include, but are not limited to, Pgp (which is encoded by the MDR-1 gene), the MDR related proteins (MRP), and BCRP (ABCG2) (67). Functionally, all members of the ABC superfamily confer MDR (67) (68). Pgp, which is encoded by the MDR-1 gene, is of particular relevance in MDR because of its broad substrate specificity, which includes, but is not limited to, anticancer agents, antihypertensive agents, antiarrhythmics, glucocorticoids, antiviral agents, antibiotics, antimycotics, immunosuppressants, antidepressants, neuroleptics, anti-epileptics, anti-acids, opioids, and antiemetics) and its wide tissue distribution (69). Like Pgp, the MRPs also differ in their membrane localization, tissue distribution and substrate specificity (68). Amongst the members of the ABC superfamily, ABCC-4 (also known as M RP-4) is unique because of its dual membrane localization in polarized cells (68). Inhibiting expression of members of the ABC superfamily genes, such as for example, MDR-1 (and its encoded protein Pgp), as well as other members of the MRP family, would make a cell less resistant to a medication and hence increase efficacy of the medication long term. This is particularly true in the treatment of cancers, but also applies to a host of other physiological disorders which can become resistant to the medication through continued use.
[0286] In one embodiment, the extract of O. stamineus leaves may substantially reduce M DR in cancer cells. In one embodiment, the ability of the extract of O. stamineus leaves to substantially reduce MDR in cancer cells was evaluated on human pancreatic cancer cells as demonstrated in Example 19. The results of this experiment are shown in Tables 43 and 44.
[0287] As described herein, angiogenesis is complex and is regulated by a set of pro- and anti-angiogenic factors which are in perfect balance in a healthy adult subject, except during wound healing, embryogenesis, hair growth and during the menstrual cycle. In cancer, tumor growth and metastasis is the result of an imbalance in the levels of pro- and anti-angiogenic factors, with more pro-angiogenic factors being released by the tumor(s) to stimulate angiogenesis and promote neovascularization for the delivery of nutrients and oxygen to the tumor for its continued growth and survival. Several pro- and anti-angiogenic factors have been identified (45) (47), some of which are listed in Table 41.
[0288] Apoptosis is a normal physiological process of programmed cell death that occurs in multicellular organisms. Apoptosis is a highly regulated and controlled process and can be contrasted from necrosis, which is a form of traumatic cell death resulting from acute cellular injury. Apoptosis can be identified by characteristic morphological changes comprising cellular blebbing, cell shrinkage, nuclear fragmentation, chromatin condensation, chromosomal DNA fragmentation, and global m RNA decay. Underlying these morphological changes are modulation of factors that control cellular pathways leading to apoptosis.
Defective apoptotic pathways have been implicated in a variety of diseases. For example, cancer can develop when the apoptotic pathways are disrupted causing cells to become immortal and proliferate out of control. On the contrary, excessive apoptosis can lead to neurodegenerative diseases, such as Parkinson's and Alzheimer's disorders. It has been postulated that cancers can occur when the balance between cell death and cell proliferation is disturbed. Thus, cancers may occur either by an increase in cell proliferation or a decrease in cell death. Biochemically, this can be, inter alia, due to the modulation of factors regulating pro- and anti-apoptosis factors. One goal of cancer therapy is to promote death of cancer cells while minimally affecting normal cells.
[0289] In one embodiment, an extract of O. stamineus leaves can modulate expression of pro- and anti-angiogenic factors, cytokines, factors implicated in apoptosis, and transcription factors that have been shown to play a role in carcinogenesis, such that the extract has an anti-carcinogenic activity. In one embodiment, the cytokine is a chemokine, interferon, interleukin, lymphokine, tumor necrosis factor, or any combination thereof. In one embodiment, the extract of O. stamineus leaves can modulate expression of pro- and anti-angiogenic factors such that the factors can inhibit proliferation and/or migration of endothelial cells. In certain embodiments, the extract of O. stamineus leaves can inhibit the expression and/or activity of pro-angiogenic factors. In certain embodiments, the extract of O. stamineus leaves can increase and/or stimulate the expression and/or activity of anti- angiogenic factors. In certain embodiments, the extract of O. stamineus leaves modulates expression of several factors such that the extract can inhibit or suppress the growth of a tumor. In certain embodiments, the extract of O. stamineus leaves modulates expression and/or activity of apoptosis factors such that the extract promotes apoptosis of transformed cells. In certain embodiments, the extract of O. stamineus leaves modulates expression and/or activity of transcription factors implicated in carcinogenesis.
[0290] In one embodiment, the levels of pro- and anti-angiogenic factors known to influence angiogenesis were measured in tissue lysates of xenograft ectopic human colorectal tumors excised from nude mice treated for 28-days with the extract of O.
stamineus leaves, RA or imatinib, using the Luminex® Multiplexing Platform (xMAP® Technology, Luminex® Corporation, TX, USA) as described in Example 20. The pro- and anti- angiogenic factors measured included VEGF, bFGF, EGF, TGF-ot, NGF-β, TNF-ot, TNF-β, I L-2, I L-7, GM-CSF, I FN-ot, I FN-β, and I FN-γ. The effect of an extract of O. stamineus leaves on the expression of the pro- and anti-angiogenic factors in human colorectal tumors is shown in Table 45.
[0291] In one embodiment, the levels of pro- and anti-angiogenic factors known to have an influence on angiogenesis were also measured in cell lysates of untreated HUVECs or HUVECs treated with the extract of O. stamineus leaves, RA or imatinib for 24hr, using the Luminex® Multiplexing Platform (xMAP® Technology, Luminex® Corporation, TX, USA). The
pro-and anti-angiogenic factors measured included VEGF, bFGF, EGF, TGF-ot, NGF-β, TNF-a, TNF-β, IL-2, IL-7, GM-CSF, IFN-a, IFN-β, and IFN-γ. The effect of an extract of O. stamineus leaves on the expression of the pro- and anti-angiogenic factors in HUVECs is shown in Table 46. The effect of an extract of O. stamineus leaves on the expression of transcription factors implicated in carcinogenesis is shown in Table 47. The effect of an extract of O. stamineus leaves on the expression of regulatory proteins implicated in apoptosis is shown in Table 48.
[0292] In one embodiment, the effect of the extract of O. stamineus leaves on VEGF165 expression in A549 cells grown in vitro and human lung adenocarcinoma tumors excised from mice was measured using an ELISA for VEGF165, the results of of which are shown in Tables 33 and 38.
[0293] In a related embodiment, the extract of O. stamineus leaves can inhibit expression of HIF-la, WNT, KDR, and COX2 genes in tumors in-vivo.
[0294] As described herein, low levels of intracellular oxygen (hypoxia) in cancer cells activates HIF-1, which comprises an a regulatory and β DNA binding subunit. Under normoxic conditions, HIF-la is targeted for proteasomal degradation. Under hypoxic conditions, however, HIF-la accumulates inside the cell and heterodimerizes with HIF-β (62). The heterodimer is now capable of binding to DNA elements referred to as hypoxia responsive elements (HREs). Under hypoxic conditions HIF targets expression of erythropoietin (for stimulation of red blood cells), VEGF, which stimulates angiogenesis, and other glycolytic enzymes, some of which have been described herein (70).
[0295] The Wingless-type M MTV Integration (Wnt) family of proteins are secreted glycolipoproteins that activate signaling pathways in nearby cells (paracrine) or same-cells (autocrine) by binding to their cognate Frizzled family receptors (71). The Wnt signaling pathways function in the vasculature to regulate proliferation, apoptosis, branch morphogenesis, cell polarity and extracellular matrix remodeling - all of which are steps essential in angiogenesis (71).
[0296] KDR, also known as VEGFR2 or CD309, is a receptor for VEGF. VEGF is an important signaling protein involved in angiogenesis and VEGFR2 appears to mediate known cellular responses to VEGF (72).
[0297] Activation of VEGFR-2 leads to proliferation, migration, survival, and increased permeability to a variety of fluids and solutes. Expression of VEGFR-2 is upregulated in the tumor vasculature compared to the normal vasculature and its increased expression is a prognostic marker in the clinical outcome of patients with a variety of malignancies (73) (74) (75).
[0298] COX catalyzes the conversion of arachidonic acid to prostaglandin H2. Two isoforms of COX have been identified, namely COX-1 and COX-2. COX-1 is constitutively expressed and is believed to be responsible for maintaining cellular homeostasis. On the other hand, COX-2 has gained significant interest as it is barely detectable in normal tissues, but is highly expressed in response to stimuli such as mitogens, cytokines, and growth factors (76). COX-2 is also overexpressed in colon, head and neck, lung, prostate, stomach, and breast cancer (76) (77). While the role of COX-2 in tumorigenesis is not clear, an increased expression of COX-2 has been associated with angiogenesis and the expression of VEGF (76) (77).
[0299] In one embodiment, the extract of O. stamineus leaves can inhibit expression of HIF-la, WNT, KDR, and COX2 genes in tumors. In one embodiment, the effect of the extract
of O. stamineus leaves, A, and imatinib on the expression of HIF-la, WNT, KDR, and COX2 genes was evaluated using total RNA isolated from xenograft ectopic colorectal tumors as demonstrated in Example 21. The results of the effect of treating mice with the extract of O. stamineus leaves, RA and imatinib for 28 days on the expression of HIF-l a, WNT, KDR, and COX2 genes in xenograft ectopic human colorectal tumors is shown in Table 50.
[0300] The vascular endothelium, which lines the inside of all blood vessels, is normally quiescent in normal adult subjects with turnover rates of months to years (78). Loss of quiescence, however, is a common feature in physiological disorders such as, angiogenesis, atherosclerosis, restenosis, and inflammation. There is now considerable evidence showing that angiogenesis and inflammation are intricately linked and share the same molecular events (12) (78) (79). The complex interplay between these two processes at both the cellular and molecular level has been well documented (reviewed in (12) and (80)).
Inflammation sustains angiogenesis by the secretion of several factors (e.g., interferons, cytokines, chemokines, growth factors) by immune cells that act on endothelial cells either directly or indirectly. In turn, angiogenesis sustains inflammation by providing the necessary nutrients and oxygen to the cells present at sites of inflammation. At least one physiological stimulus common to both inflammation and angiogenesis appears to be hypoxia. As described herein, hypoxia activates HIF1, which in turn up-regulates expression of several key proteins related to angiogenesis. Additionally, cells respond to hypoxia by production of nitric oxide (NO), which is produced by inducible NO Synthase (iNOS) in immune cells. NO promotes vasodilation and increases permeability of the endothelial lining, which is not only required for the extravasation of immune cells, but also promotes metastasis of tumors.
[0301] Normally, the body's response to inflammation leads to a fast healing process and a return of the vascular endothelium to the quiescent state. However, in certain physiological disorders, sustained release of proinflammatory factors leads to chronic inflammation, hyper-activation of endothelial cells, induction of angiogenesis and tissue damage. Chronic inflammation underlies the pathophysiology of several physiological disorders such as psoriasis, arthritis (rheumatoid arthritis and osteoarthritis, atherosclerosis, diabetes, Crohn's disease, and cancer (12).
[0302] Inflammation has been described as an "enabling characteristic" of cancer (81). Hypoxia, angiogenesis, infiltration of immune cells and fibroblasts, high levels of proinflammatory cytokines and growth factors, and ongoing tissue remodeling are observed during inflammation and tumor growth. In cancer, the tumor microenvironment can be regarded as chronically inflamed tissue rich in immune cell-derived factors with pro- angiogenic activity, such as for example, IL-1, IL-6, IL-7, IL-8, TNF-ot, COX-2 and VEGF. These factors stimulate neighboring fibroblasts and endothelial cells to further secrete angiogenic factors such as VEGF, bFGF, EGF, β-NGF, and TGF-ot and promote angiogenesis. Further, generation of ROS can induce mutations in not only the DNA of cells producing this highly reactive species of molecules, but also in the DNA of neighboring cells, which can promote tumorigenesis. Another line of evidence linking inflammation and tumorigenesis is the observation that non-steroidal anti-inflammatory drugs (NSAIDs) have anticancer activity (80) (82) (83) (84) (85) (86).
[0303] In one embodiment, the extract of O. stamineus leaves can inhibit expression of inflammatory cytokines. In at least one embodiment, the extract of O. stamineus leaves can inhibit expression of IL-1, TNF-ot, and NO in human macrophages. In one embodiment, the
effect of the extract of O. stamineus leaves on the expression of inflammatory cytokines in comparison to A and indomethacin (a nonsteroidal anti-inflammatory drug (NSAID) commonly used as a prescription medication to reduce fever, pain, stiffness, and swelling from inflammation) was tested on Salmonella abortus lipopolysaccharide (LPS) stimulated macrophages as demonstrated in Example 22. The effect of the extract of O. stamineus leaves on the expression of IL-1, TNF-ot, and NO relative to untreated cells and the effect of RA on the expression of IL-1, TNF-ot, and NO relative to untreated cells is shown in Table 51. The expression of TNF-ot was inhibited by the extract of O. stamineus leaves with an IC5o value of 63 ± l^g/mL. The expression of IL-1 was inhibited by the extract of O. stamineus leaves with an IC5o = 88 ± l^g/mL. Expression of NO was inhibited by the extract of O. stamineus leaves with an IC5o = 371 ± 1.9 μg/mL. RA inhibited TNF-ot expression with an IC5o = 63 μg/mL, IL-1 expression with an IC50 = 103 ± 2%μg/mL. RA at 25 μg/ml showed 31% inhibition of NO expression.
[0304] In one embodiment, the extract of O. stamineus leaves can inhibit the enzyme activity of COX-1 and COX-2. The effect of the extract of O. stamineus leaves on the enzyme activity of COX-1 and COX-2 in comparison to aspirin (a nonselective NSAID of both COX-1 and COX-2, but is weakly more selective for COX-1) and celecoxib (the COX-2 selective NSAID) was tested on recombinant COX-1 (ovine) and COX-2 (human) as demonstrated in Example 22. The effect of the extract of O. stamineus leaves, celecoxib and aspirin on the enzyme activity of COX-1 and COX-2 is shown in Table 52.
[0305] Oxidative stress occurs during excess production of ROS. Oxidative stress causes damage to essential cellular functions and is implicated in various diseases. It is linked to inflammation, cancer, atherosclerosis, aging, ischemic injury and neurodegenerative diseases (87). Naturally derived antioxidants have attracted increasing interest among consumers and the scientific community because epidemiological studies have indicated a great number of health benefits (88) (89). Antioxidants are needed to prevent oxidative stress, which causes damage to cell membranes and other structures such as
deoxyribonucleic acid (DNA), proteins and lipids (90). Fruits and vegetables are natural sources of antioxidants, which contain three major groups of phytochemicals: vitamins, phenolics, and carotenoids.
[0306] Antioxidants play an essential role against the damaging effects of ROS, such as superoxide, hydroxyl radicals, singlet oxygen, peroxynitrite and peroxyl radicals. Cellular damage occurs due to an imbalance between antioxidants and reactive oxygen species, because of exposure to free radicals generated by exogenous agents such as hyperoxia, chemicals, radiation and endogenous processes, such as normal cellular metabolism (91).
[0307] As described herein, extracts of O. stamineus are rich in antioxidants. In one embodiment, the extract of O. stamineus leaves comprises antioxidant activity. In one embodiment, the antioxidant activity of the extract of O. stamineus leaves was assessed based on the capacity of the extract to reduce the ABTS radical cation (ABTS+). In one other embodiment, the antioxidant activity of the extract of O. stamineus leaves was assessed based on the capacity of the extract to reduce Fe3+/tripyridyltriazine complex to its blue- colored ferrous form (FRAP). In still another embodiment, the antioxidant capacity of the extract of O. stamineus leaves was assessed based on its ability to scavenge l,l-diphenyl-2- picrylhydrazyl (DPPH). These various embodiments are described in Example 23. The results are shown in Tables 53 and 54.
[0308] Macerated methanol, chloroform, and aqueous extracts of O. stamineus have been shown to reduce blood glucose levels in normal and STZ induced Type 2 diabetic rats (92) (93) (94) (95). Accordingly, the ability of the extract of O. stamineus leaves to also lower blood glucose was evaluated by administering two different formulations comprising the extract of O. stamineus leaves in human patients diagnosed with Type 2 diabetes as demonstrated in Example 24. In one embodiment, the extract of O. stamineus leaves can lower blood glucose levels in a subject diagnosed with Type 2 diabetes. In another embodiment, the extract of O. stamineus leaves can promote maintenance of healthy blood sugar levels in a subject. In one embodiment, the extract of O. stamineus leaves can be administered as an adjunct treatment for the maintenance of healthy blood glucose levels in Type 2 diabetic patients.
[0309] The effect of the extract of O. stamineus leaves in lowering blood glucose in these patients is shown in Table 55 and Fig. 8. The data show that regardless of the dosage forms, the extract of O. stamineus leaves was effective in lowering blood glucose in humans. Table 55 also shows that the blood glucose levels in these patients was well controlled. The American Diabetes Association (ADA) has established blood glucose targets for adult nonpregnant adults with diabetes (Diabetes Care. 2016. 39 (suppl 1): S1-S106). The ADA recommends that such patients maintain preprandial plasma glucose between 4.4 - 7.2 mmol/L (80 - 130 mg/dL) and peak postprandial plasma glucose at <10 mmol/L (<180 mg/dL). Table 55 shows that at the end of the 7-day administration period, 63% of the patients maintained their preprandial plasma glucose levels and 88% of the patients were able to maintain their postprandial plasma glucose levels within or below the recommended ADA targets.
[0310] Hypertension or high blood pressure is one of the leading causes of death among the industrialized societies (96). Globally, about one-quarter of the adult population suffers from hypertension (97). It is a major risk factor for cardiovascular disease and related complications, such as heart disease, kidney damage, eye damage and stroke (98). The renin-angiotensin-aldosterone system ( AAS) is a key determinant in the maintenance of arterial blood pressure. ACE-I (EC3.4.15.1) is one of the main components of the RAAS (99). ACE-I is a glycosylated zinc dipeptidyl-carboxypeptidase, which catalyzes the conversion of the precursor angiotensin I into angiotensin II. ACE-I regulates arterial blood pressure and electrolyte balance by triggering vasoconstriction of blood vessels and degrades bradykinin, which is a potent vasodilator in the RAAS. Therefore, inhibition of ACE-I is a promising target for regulation and treatment of high blood pressure (100).
[0311] While many of the synthetic ACE-I inhibitors such as captopril, benazepril, enalapril and alacepril are widely used in the treatment of hypertension and heart failure, the chronic use of these synthetic inhibitors may be associated with many undesirable side effects, such as persistent cough, postural hypotension, renal failure, and angioedema (101) (102) (103). Several studies have recently been conducted to discover new ACE-I inhibitor compounds from natural resources (104) (105). Natural ACE-I inhibitors as alternatives to synthetic ones are of interest for their better drug profiles and fewer side effects (106). ACE- I inhibition by natural substances, such as peptides and triterpenes, have been described in the literature (107) (108) (109). Recent studies have also demonstrated in vitro inhibition of ACE-I by flavonoid compounds isolated from different plants (110) (111) (112). The inhibitory effect of these flavonoid compounds has been largely ascribed to the generation of chelate
complexes within the active center of ACE-I (113). Phenolic compounds such as ferulic acid and tannic acid and flavonoids such as quercetin, anthocyanins, flavones and flavonols have been shown to inhibit different zinc metalloproteinases, including ACE-I (113) (114) (115) (116) (117) (118) (119). Moreover, the ACE-I inhibitory activity of different foods and plant extracts rich in flavonoids have also been demonstrated by in vitro and in vivo studies in spontaneous hypertensive rats (110) (120) (121). Macerated methanolic extracts of O. stamineus have been shown to have antihypertensive effects in spontaneous hypertensive rats (122). Further, Shafaei et.al. (123) have demonstrated that macerated water (OS-W), macerated 100% EtOH (OS-E), macerated 100% methanol (OS-M), macerated 50%
EtOH/water (OS-EW), and macerated 50% methanol/water (OS-MW) extracts of O.
stamineus inhibit ACE-I activity in the following order: (Highest) OS-E > OS-M > OS-EW > OS- MW > OS-W (Lowest). Shafaei et al. (123) also assessed the in-vitro ACE-I inhibition activity and binding ability of the four major phytochemicals present in these extracts, namely, A, EUP, SIN, and TMF. Their data show that both binding of ACE-I and inhibition of ACE-I activity followed the following order: (Highest) EUP > RA > TMF > SIN (Lowest). Accordingly, in one embodiment, the extract of O. stamineus leaves can inhibit ACE-I activity. In at least one other embodiment, the extract of O. stamineus leaves can comprise antihypertensive activity and thus lower blood pressure. One embodiment illustrating the effect of the extract of O. stamineus is described in Example 25.
[0312] The involvement of the cholinergic system has emerged as a common denominator in the etiology of several neurodegenerative diseases. The cholinergic system comprises nerve cells that release acetylcholine as the neurotransmitter during propagation of a nerve impulse. Acetylcholine, when released into the synaptic cleft by the presynaptic neuron or by the motor neuron at the neuromuscular junction, binds to its receptor on the postsynaptic neuron or to its receptor on the sarcolemma of the muscle at the
neuromuscular junction, allowing for the continued transmission of the impulse in the postsynaptic neuron or contraction of the muscle. Termination of the signal is achieved by AChE, the enzyme which hydrolyses acetylcholine into choline and acetate.
Neurodegenerative diseases, particularly those affected by the cholinergic system, are characterized neurochemical^ by a consistent deficit in cholinergic neurotransmission. Examples of such neurodegenerative disorders include, without limitation, AD, PD, dementia, DLB, movement disorders (e.g., myasthenia gravis), and ALS. The aim of therapies for the treatment of such neurodegenerative diseases has been to target inhibition of AChE (122), thereby enabling accumulation of acetylcholine in the synaptic cleft and
neuromuscular junction, which then allows for prolonged activation of postsynaptic neurons or contraction of muscle.
[0313] Several drugs have been approved, are under pre-clinical, or clinical development that target AChE and inhibit its activity. These include for example, physostigmine, tacrine, donepezil, metrifonate, galanthamine, rivastigmine, tolserine, esolerine, tesofensine, huperzine A, huperzine B, extracts of Nelumbo nucifera and
Himatanthus lancifolius, galangin, rutin, donepezil hybrids, tacrine hybrids, galantamine derivatives, rivastigmine derivatives, xanthostigmine derivatives, aminobenzoic acid derivatives, pyrrolo-isoxazole derivatives, coumarin, coumarin derivatives, and synthetic analogues, such as for example phenyl-5,6-dimethoxy-l-oxo-2,3-dihydro-lH-2-indenyl- methanone analogues, N-alkyl-7-methoxytacrine hydrochlorides, and ladostigil (125) (126).
[0314] Phytochemicals from plants have been, and are still considered to be, an important source of AChE inhibitors (e.g., physostigmine, rivastigmine (a semi-synthetic derivative of physostigmine), galanthamine, huperzine A and B, for example, are plant derived inhibitors of AChE). A significant number of plant extracts, other than that of Nelumbo nucifera and Himatanthus lancifolius have also been reported to have potent AChE inhibitory activity (127) (128) (129).
[0315] In one embodiment, the extract of O. stamineus leaves can inhibit AChE activity. The effect of the extract of O. stamineus leaves on inhibition of AChE activity is
demonstrated in Example 26. The data are shown in Table 56. The extract of O. stamineus leaves showed strong AChE inhibitory activity (80-90%) at 5 mg/ml at all time points with an IC5o value of 3.13mg/ml.
[0316] Given that current therapies aim to treat neurodegenerative diseases such as AD, PD, dementia, DLB, movement disorders (e.g., myasthenia gravis), and ALS by inhibiting the activity of AChE, and since the extract of O. stamineus leaves inhibits the activity of AChE, certain embodiments provide for the use of a therapeutically effective amount of an extract of O. stamineus leaves or a formulation comprising a therapeutically effective amount of an extract of O. stamineus leaves in the treatment of neurodegenerative diseases.
[0317] Certain proteins normally soluble in living organisms can form aggregates of β- pleated sheet structures called amyloid. These intra- or extra-cellular deposits are hallmarks of many neurodegenerative pathologies including vascular dementia, Alzheimer's disease (AD), Huntington's disease Fragile X syndrome, Downs syndrome, Autism, Parkinson's disease (PD), prion disease, and other progressive neurological diseases that develop in the aging human central nervous system.
[0318] AD is a chronic neurodegenerative disease characterized clinically by a progressive and gradual decline in memory and thinking skills and, eventually, the ability to carry out the simplest tasks. The hallmark pathological features of AD include the presence of extracellular plaque deposits (senile plaques) composed primarily of: 1) Αβ peptide, a highly penetrative, aggregate-prone, and toxic, family of peptides, in brain parenchyma and, 2) intracellular neurofibrillary tangles (N FT) due to hyperphosphorylation of the microtubule binding protein tau within neurons. The "amyloid cascade hypothesis" proposes that amyloidogenesis, i.e., the formation of amyloid-β aggregates (also referred to as Αβ plaques or senile plaques), in the brain is a central event in the pathogenesis in these
neurodegenerative disorders, particularly in AD (130). Both Αβ aggregates and NFTs are believed to contribute to synaptic dysfunction and premature neuronal death. Despite the long standing observation that neurodegenerative neurons show a strong correlation with formation of senile plaques, formation of senile plaques doesn't appear to be sufficient in the progression of AD, suggesting that other key factors are necessary for the pathogenesis and continued progression of the disease (130) (131) (132) (133).
[0319] Recent research has clearly established oxidative stress as an important contributor to the etiology of AD (134) (135) (136) (137). Oxidative stress is characterized by an imbalance in the production of ROS and/or oxidative defence mechanisms, resulting in excessive production of ROS. It is believed that oxidative stress in the brain participates in protein oxidation, lipid oxidation, nucleic acid oxidation and glycoxidation of neuronal components due to mitochondrial dysfunction, increased metal levels, inflammation, and Αβ
peptides (138) (137). Cellular changes suggest that oxidative stress precedes the hallmark features of AD (136) and promotes Αβ deposition and tau hyperphosphorylation, resulting ultimately in synaptic loss and neuronal death (137).
[0320] A growing body of evidence suggests that vascular dysfunction is a crucial pathological hallmark of AD. The "vascular hypothesis" proposes that the leakiness of the blood-brain-barrier, which precedes other AD pathology, is likely due to hypoxia and inflammation which leads to vascular damage and eventual apoptosis (130) (131) (132) (133). An alternative hypothesis proposes that amyloidogenesis stimulates angiogenesis leading to increased vascular permeability and hypervascularization seen in AD (131) (132) (133). This alternative hypothesis proposes that impaired cerebral blood flow, tight junction disruption of the blood-brain-barrier, and disturbances in proteins regulating Αβ levels in the brain contribute to elevated Αβ levels, which in turn stimulates angiogenesis. In addition, inflammation gives rise to elevated pro-angiogenic cytokines such as vascular endothelial growth factor (VEGF), further promoting vascular remodeling in the AD brain.
Neovascularization leads to further Αβ secretion by endothelial cells, which in turn increases oxidative stress, endothelial damage, and neuronal death.
[0321] The neovascularization observed in AD brains parallels the pathogenic angiogenesis seen in many other angiogenesis dependent disorders described herein, such as for example, tumorigenesis, diabetes, and ophthalmic disorders. The brain and eye share many similarities in both development and pathology (139). Both the retinal-blood-barrier and blood-brain-barrier share a similar structure and interface with their neighbouring vasculature. Αβ deposits, (referred to as drusen) similar to senile plaques, are also observed in degenerating retinas. Localized retinal inflammation is also observed in patients with ophthalmic disorders. Recent research has shown increased levels of Αβ is associated with AMD (139) (140) and diabetic retinopathy (141). Further, anti-Αβ therapy is able to attenuate AM D pathology and protect retinal pigmented epithelium and subsequent vision loss (142) (143).
[0322] The multi factorial nature of ophthalmic disorders, such as for example, AMD, glaucoma, diabetic retinopathy, and neurodegenerative disorders, such as for example, AD, suggest that these diseases, can benefit from combinatorial therapy. Accordingly, the use of an API that can effect multiple pathways leading to establishment and progression of these disorders would be a significant advance in the treatment of such disorders.
[0323] In one embodiment, the extract of O. stamineus can prevent Αβ dependent or Αβ induced cell death (Example 33). One embodiment provides for a method of treating a neurological and/or ophthalmic disorder by preventing or slowing the progression of Αβ dependent or Αβ induced cell death in a subject in need thereof, said method comprising administering to the subject a therapeutically effective amount of an extract of O. stamineus leaves or a formulation comprising a therapeutically effective amount of an extract of O. stamineus leaves for preventing Αβ dependent or Αβ induced cell death. In one
embodiment, the neurological disorder can be a neurodegenerative disorder. In one embodiment, the neurodegenerative disorder is associated with an aging central nervous system. In one embodiment, the ophthalmic disorder is associated with an aging retina.
FORMULATIONS
[0324] The extract of O. stamineus leaves can be formulated in a variety of
formulations and manufactured into a variety of dosage forms well known in the art. In one embodiment, formulations comprising the extract of the O. stamineus leaves, can be either multiparticulate or monolithic and prepared into single or multi-administration dosage forms for oral or non-oral administration. In certain embodiments, the formulations comprising the extract of O. stamineus leaves can be manufactured into a variety of dosage forms. Non-limiting examples of dosage forms include immediate release dosage forms (oral or non-oral), modified release dosage forms (oral or non-oral), a sublingual film, a sublabial film, a buccal film, an ointment, a gel, dendrimers, an oral spray, an orally disintegrating tablet, a lozenge, an effervescent tablet, sublingual drops, a lollipop, a chewing gum, an oral solid immediate release dosage form (e.g. tablets, microspheres, granules, mini tablets, etc.), an oral modified release dosage form (e.g. tablets, microspheres, granules, mini tablets, etc.), a capsule, a gelcap, a pastille, multiparticulates (e.g., microspheres, granules, powder), a mini tablet, a caplet, an effervescent powder, a hydrogel, syrups, a medicated straw, a dry-powder inhaler, a nebulizer, a metered dose inhaler, a suppository, aerosol devices (e.g., e-cigarretes), a catheter, a vaginal tablet, a vaginal cream, a vaginal suppository, a vaginal ring, a dermal patch (e.g., a transdermal patch), ethosomes, niosomes, discosomes, phytosomes, liposomes, a lotion, a lip balm, an ointment, a cream, an emulsion, a topical spray, a nasal spray, a medicated shampoo, eye drops, an injectable, a topical emulsion, biodegradable microparticles, biodegradable microspheres, biodegradable nano- microspheres, nanoparticles, polymeric microparticles, polymeric nanoparticles, steroidal nano microparticles, steroidal microparticles, silicon microneedles, or nanostructured lipid carriers. Combinations of dosage forms are permissible.These, and other formulations, and their methods of manufacture are well known in the art and can be found in the relevant literature, for example in (144) (145) (146). Examples of specific excipients for use in formulating the various formulations are well known to those of skill and can also be found in these references as well as in the U.S. Pharmacopeia.
[0325] In one embodiment, the powder obtained at the end of the manufacturing process can be sieved through an appropriate size mesh screen to obtain a powder of substantially uniform sized particles. In certain embodiments, the sieved or unsieved powder can be encapsulated or directly compressed to form immediate release dosage forms. The powder can be encapsulated or compressed into immediate release cores. In certain embodiments, the powder can comprise one or more pharmaceutically acceptable excipients and formulated into an immediate release tablet or powder. One example of an immediate release tablet and powder comprising one or more pharmaceutically acceptable excipients is described in Example 30. In other embodiments, the immediate release cores can comprise at least one disintegrant. Non-limiting examples of disintegrants for use in the immediate release cores include croscarmellose sodium, crospovidone, alginic acid, sodium alginate, methacrylic acid DVB, cross-linked PVP, microcrystalline cellulose, polacrilin potassium, sodium starch glycolate, starch, pregelatinized starch and the like. The disintegrant can be present in an amount of from >0% to 20% of the total weight of the core. In at least one embodiment the disintegrant is selected from cross-linked
polyvinylpyrrolidone (e.g. KOLLIDON® CL), cross-linked sodium carboxymethylcellulose (e.g. Ac-Di-Sol), starch or starch derivatives such as sodium starch glycolate (e.g. EXPLOTAB®), or
combinations with starch (e.g. P IMOJEL™), swellable ion-exchange resins, such as
Amberlite IRP 88, formaldehyde-casein (e.g. ESMA SPRENG™), and mixtures thereof.
[0326] Optionally, the sieved or unsieved powder can comprise other pharmaceutically acceptable ingredients which are conventional in the pharmaceutical art and can facilitate the preparation and/or improve patient acceptability of the final dosage form as described herein. The additional inert excipients are well known to the skilled person and can be found in the relevant literature, for example in (144) (145) and the U.S. Pharmacopeia. Non- limiting examples of such excipients include diluents, lubricants, binders, granulating aids, colorants, flavourants, surfactants, pH adjusters, anti-adherents and glidants, e.g. dibutyl sebacate, ammonium hydroxide, oleic acid and colloidal silica. In certain other
embodiments, the sieved or unsieved powder can be blended with other additional inert excipients, which can improve further processing of the powder. For example, the powder can be blended with other excipients, such as for example, a lubricant, and if necessary, any additional inert excipients, such as for example a glidant, in a suitable blending apparatus. Glidants can improve the flowability of the powder. This is especially important during tablet production at high production speeds and during direct compaction.
[0327] Optionally, the powder can be granulated with pharmaceutically acceptable excipients. In certain embodiments, the sieved or unsieved powder, or granules can be formulated together with other pharmaceutically acceptable excipients and homogeneously dispersed into a matrix to form a formulation comprising a normal release matrix.
[0328] In certain embodiments, the sieved or unsieved powder, granules, immediate release, or normal release matrices can be further coated. In certain embodiments, the coat can be a suitable polymer based coat to further modulate the release of the extract of O. stamineus leaves.
[0329] Certain embodiments provide for formulations featuring a normal release matrix, the matrix comprising a therapeutically effective amount of the extract of O.
stamineus leaves, which has been suitably granulated. The normal release matrix can comprise excipients, including polymers, which do not retard the release of the extract of O. stamineus leaves from within the matrix. The normal release matrix can also contain other pharmaceutically acceptable ingredients which are conventional in the pharmaceutical art and can facilitate the preparation and/or improve patient acceptability of the final dosage form as described herein. The additional inert excipients are well known to the skilled person and can be found in the relevant literature, for example in (144) (145). Non-limiting examples of such excipients include diluents, lubricants, binders, granulating aids, colorants, flavourants, surfactants, pH adjusters, anti-adherents and glidants, e.g. dibutyl sebacate, ammonium hydroxide, oleic acid and colloidal silica. Optionally, the normal release matrix can comprise at least one disintegrant. Examples of disintegrants described for use in immediate release cores can also be used in normal release matrix and in the same amount.
[0330] In certain embodiments, the sieved or unsieved powder can be granulated together with certain pharmaceutically acceptable excipients, including polymers which can modify the release of the extract of O. stamineus leaves such that the release profile is not immediate release. Certain embodiments provide for modified release formulations featuring controlled release matrices from which the rate of release of the extract of O. stamineus leaves from the matrix is dependent at least in part upon the diffusion and/or erosion properties of excipients within the matrix. In certain embodiments, controlled
release matrices comprise a therapeutically effective amount of the extract of O. stamineus leaves and at least one pharmaceutically acceptable polymer. In certain embodiments, the pharmaceutically acceptable polymer is a pH independent polymer, pH dependent (such as for example enteric or reverse enteric types) polymer, soluble polymer, insoluble polymer, lipids, lipidic materials, or any combination thereof which when formulated together with the extract of O. stamineus leaves can slow the release of the extract of O. stamineus leaves from the matrix. Those skilled in the pharmaceutical art and the design of medicaments are aware of modified release dosage forms conventionally used in oral pharmaceutical compositions adapted for controlled release and means for their preparation. Examples of controlled release matrices are described in U.S. Pat. Nos. 6,326,027; 6,340,475; 6,905,709; 6,645,527; 6,576,260; 6,254,887; 6,306,438; 6,129,933; 5,891,471; 5,849,240; 5,965,163; 6,162,467; 5,567,439; 5,552,159; 5,510,114; 5,476,528; 5,453,283; 5,443,846; 5,403,593; 5,378,462; 5,350,584; 5,283,065; 5,273,758; 5,266,331; 5,202,128; 5,183,690; 5,178,868; 5,126,145; 5,073,379; 5,023,089; 5,007,790; 4,970,075; 4,959,208; 4,861,598; 4,844,909; 4,834,984; 4,828,836; 4,806,337; 4,801,460; 4,764,378; 4,421,736; 4,344,431; 4,343,789; 4,346,709; 4,230,687; 4,132,753; 5,591,452; 5,965,161; 5,958,452; 6,156,342; 5,395,626; 5,474,786; and 5,919,826.
[0331] Suitable excipient materials for use in controlled release matrices include, by way of example, release-resistant or controlled release materials such as hydrophobic polymers, hydrophilic polymers, lipophilic materials and mixtures thereof, and can be present in an amount from 5% to 90% by weight of the controlled release matrix. Examples of as hydrophobic polymers, hydrophilic polymers and lipophilic materials suitable for use in controlled release matrices can be found, for example, in U.S. Pat. No. 7,569,610.
[0332] In at least one embodiment, the controlled release matrix can comprise at least one binder. In certain embodiments, the binder can be water-insoluble. Examples of suitable binders have been described, for example, in U.S. Pat. No. 7,569,610. In at least one embodiment, the binder can be present in an amount of from 0.1% to 20% (e.g., 0.1%, 0.5%, 1%, 2%, 3%, 4%, 5%, 6%, 7%, 8%, 9%, 10%, 11%, 12%, 13%, 14%, 15%, 16%, 17%, 18%, 19%, or 20%) by weight of the matrix formulation.
[0333] In at least one embodiment, the controlled release matrix can comprise at least one lubricant. Non-limiting examples of suitable lubricants have been described, for example, in U.S. Pat. No. 7,569,610. The lubricant can be present in an amount of from 0 to 4% (e.g., 0%, 0.1%, 0.2%, 0.3%, 0.4%, 0.5%, 0.6%, 0.7%, 0.8%, 0.9%, 1%, 1.5%, 2%, 2.5%, 3%, 3.5%, or 4%) by weight of the controlled release matrix.
[0334] In at least one embodiment, the controlled release matrix can comprise a plasticizer. Plasticizers can also function to slow the release of the extract of O. stamineus leaves from the controlled release matrix. Non-limiting examples of suitable plasticizers have been described, for example, in U.S. Pat. No. 7,569,610. In at least one embodiment, the plasticizer can be present in an amount of from 1% to 70% by weight of the controlled release polymer in the controlled release matrix.
[0335] In at least one embodiment, the controlled release matrix can comprise at least one diluent, non-limiting examples of which have been described, for example, in U.S. Pat. No. 7,569,610. In certain embodiments, the diluent can be added in an amount so that the combination of the diluent and the active substance i.e., the extract of O. stamineus leaves, comprises up to 60% by weight of the matrix.
[0336] In at least one embodiment, the controlled release matrix can comprise a solubilizer. The solubilizer can act to increase the solubility of the extract of O. stamineus leaves. The solubilizer can be a hydrophilic surfactant, lipophilic surfactant, or mixtures thereof. The surfactant can be anionic, nonionic, cationic, zwitterionic, or any combination thereof. Examples of suitable solubilizers are well known in the art and have been described, for example, in U.S. Pat. No. 7,569,610.
[0337] In at least one embodiment, the controlled release matrix can comprise a swelling enhancer. Swelling enhancers are members of a special category of excipients that swell rapidly resulting in an increase in the size of the matrix. At lower concentrations, these excipients can be used as superdisintegrants; however, at concentrations above 5% w/w these agents can function as swelling enhancers and help increase the size of the controlled release matrix. Examples of swelling enhancers have been described, for example, in U.S. Pat. No. 7,569,610. The content of the swelling enhancer can be from 5% to 90% (e.g., 5%, 10%, 15%, 20%, 25%, 30%, 35%, 40%, 45%, 50%, 55%, 60%, 65%, 70%, 75%, 80%, 85%, or 90%) by weight of the controlled release matrix. For example, in certain embodiments the swelling enhancer is present in an amount of from 10% to 70% (e.g., 10%, 15%, 20%, 25%, 30%, 35%, 40%, 45%, 50%, 55%, 60%, 65%, or 70%), and in other embodiments from 15% to 50% (e.g., 15%, 20%, 25%, 30%, 35%, 40%, 45% or 50%) by weight of the controlled release matrix.
[0338] In at least one embodiment, the controlled release matrix can comprise additives (hereinafter referred to as "hydrophilic base") for allowing water to penetrate the matrix. In certain embodiments, the amount of water required to dissolve 1 g of the hydrophilic base is not more than 5 ml, and in other embodiments is not more than 4 ml at the temperature of 20° C ± 5° C. The higher the solubility of the hydrophilic base in water, the more effective is the base in allowing water into the controlled release matrix. Examples of the hydrophilic base are well known in the art and have been described for example in U.S. Pat. No. 7,569,610.
[0339] In at least one other embodiment, the controlled release matrix is designed to achieve zero order release of the extract of O. stamineus leaves. The kinetics of the release of the extract from a controlled release matrix is governed by a combination of different polymers with different swelling characteristics. More specifically, the extract of O.
stamineus leaves is first granulated with or encapsulated in a less swellable polymer, such as a gum. This granule is incorporated into a matrix of a more swellable, erodible polymer. The more swellable erodible polymer has a diffusion rate coefficient which is greater than the diffusion rate coefficient of the relatively less swellable polymer. Averaged over the entire period of drug release, the diffusion rate for the more swellable polymer is greater than the diffusion rate for the less swellable polymer. It is this general difference in rates of diffusion between the first and second polymers which controls the rate of release of the extract of O. stamineus leaves and allows the system to approach zero order drug delivery over the drug release period. In at least one embodiment, pectin and HPMC can be present as the more swellable polymers in ratios of between 2:7 and 4:5 and gelatin can be present as the less swellable polymer.
[0340] One embodiment, provides for a controlled release matrix comprising the extract of O. stamineus leaves incorporated within a homogeneous matrix including effective amounts of at least two polymers having opposing wettability characteristics,
wherein at least one polymer(s) is selected which demonstrates a stronger tendency towards hydrophobicity and the other polymer(s) is selected which demonstrates a stronger tendency towards hydrophilicity. In at least one embodiment, the polymer demonstrating a stronger tendency towards hydrophobicity can be EC whereas the polymer demonstrating a stronger tendency towards hydrophilicity can be HEC and/or HPMC. In one embodiment, the controlled release matrix can be encased in a coating material that prevents the burst and/or food effect associated with orally ingested medicaments. In accordance with at least one embodiment is a method for preparing a device for the controlled release of the extract of O. stamineus leaves, the method comprising blending granules comprising the extract of O. stamineus leaves with 1% to 25% (e.g., 1%, 2%, 3%, 4%, 5%, 6%, 7%, 8%, 9%, 10%, 11%, 12%, 13%, 14%, 15%, 16%, 17%, 18%, 19%, 20%, 21%, 22%, 23%, 24%, or 25%) by weight of hydrophilic polymer, and 1% to 25% (e.g., 1%, 2%, 3%, 4%, 5%, 6%, 7%, 8%, 9%, 10%, 11%, 12%, 13%, 14%, 15%, 16%, 17%, 18%, 19%, 20%, 21%, 22%, 23%, 24%, or 25%) by weight of hydrophobic polymer, adding suitable pharmaceutical excipients, surface active agents and lubricants, granulating the mixture with solvents such as isopropyl alcohol, drying the granular mixture, milling the dried mixture, adding from 5% to 70% (e.g., 5%, 10%, 15%, 20%, 25%, 30%, 35%, 40%, 45%, 50%, 55%, 60%, 65%, or 70%) by weight of ethylcellulose, adding a lubricant and optionally a glidant and compressing the granules into matrices.
[0341] In another embodiment, a swellable controlled release matrix is provided in which the extract of O. stamineus leaves is dispersed in a polymeric matrix that is water- swellable rather than merely hydrophilic, that has an erosion rate that is substantially slower than its swelling rate, and that releases the extract of O. stamineus leaves primarily by diffusion. The rate of diffusion of the extract of O. stamineus leaves out of the swellable matrix can be slowed by increasing the drug particle size, by the choice of polymer used in the matrix, and/or by the choice of molecular weight of the polymer. The swellable matrix is comprised of a relatively high molecular weight polymer that swells upon ingestion. In at least one embodiment the swellable matrix swells upon ingestion to a size that is at least twice its unswelled volume, and that promotes gastric retention during the fed mode. The swellable matrix itself is solid prior to administration and, once administered, remains undissolved in (i.e., is not eroded by) the gastric fluid for a period of time sufficient to permit the majority of the extract of O. stamineus leaves to be released during the fed mode. The rate-limiting factor in the release of the extract of O. stamineus leaves from the swellable matrix is therefore controlled diffusion of the extract of O. stamineus leaves from the swellable matrix rather than erosion, dissolving or chemical decomposition of the swellable matrix.
[0342] The water-swellable polymer forming the swellable controlled release matrix can be any polymer that is non-toxic, that swells in a dimensionally unrestricted manner upon imbibition of water, and that provides for a modified release of the extract of O.
stamineus leaves. Non-limiting examples of polymers suitable for use in the swellable controlled release matrices are well known in the art and have been described, for example, in U.S. Pat. No. 7,569,610.
[0343] The hydrophilicity and water swellability of water swellable polymers can cause the extract of O. stamineus leaves comprising the swellable controlled release matrix to swell in size in the gastric cavity due to ingress of water to achieve a size that can be retained in the stomach when introduced during the fed mode. These qualities also cause
the swellable controlled release matrix to become slippery, which provides resistance to peristalsis and further promotes their retention in the stomach. The release rate of the extract of O. stamineus leaves from the swellable controlled release matrix is primarily dependent upon the rate of water imbibition and the rate at which the extract of O.
stamineus leaves dissolves and diffuses from the swollen polymer, which in turn is related to the concentration of the extract of O. stamineus leaves in the swellable controlled release matrix. Also, because these polymers dissolve very slowly in gastric fluid, the swellable controlled release matrix maintains its physical integrity over at least a substantial period, for example in many cases at least 90% and preferably over 100% of the dosing period. The matrix will then slowly dissolve or decompose. Complete dissolution or decomposition can not occur until 24 hours or more after the intended dosing period ceases, although in most cases, complete dissolution or decomposition will occur within 10 to 24 hours after the dosing period. The amount of polymer relative to the extract of O. stamineus leaves can vary, depending on the release rate desired of the extract of O. stamineus leaves and on the polymer, its molecular weight, and excipients that can be present in the swellable controlled release matrix and is within the purview of the skilled person.
[0344] The water-swellable polymers of the swellable controlled release matrix can be used individually or in combination. Certain combinations of the water-swellable polymers can provide a more controlled release of the extract of O. stamineus leaves then when used individually. Examples include cellulose-based polymers combined with gums, such as hydroxyethyl cellulose or hydroxypropyl cellulose combined with xanthan gum. Another example is poly(ethylene oxide) combined with xanthan gum.
[0345] The release rate of the extract of O. stamineus leaves from a modified release formulation can be achieved over a wide range of the extract of O. stamineus and polymer levels, with the weight ratio of the extract of O. stamineus leaves to polymer ranging from 0.01:99.99 to 80:20.
[0346] Gastric retentive formulations can achieve at least the following: (i) render the matrix sufficiently large to cause retention in the stomach during the fed mode; (ii) localizes the release of the extract of O. stamineus leaves to the stomach and small intestine so that the drug will have its full effect without colonic degradation, inactivation, or loss of bioavailability; (iii) retard the rate of diffusion of the extract of O. stamineus leaves long enough to provide multi-hour, controlled delivery of the extract of O. stamineus leaves into the stomach.
[0347] The cores comprising the extract of O. stamineus leaves can assume the form of microparticles, tablets, or microparticles retained in capsules. In at least one embodiment the formulation comprises microparticles compressed into a packed mass for ingestion, even though the packed mass will separate into individual particles after ingestion. Conventional methods can be used for compressing the microparticles in this manner. For example, the microparticles can be placed in gelatin capsules known in the art as "hard-filled" capsules and "soft-elastic" capsules. The compositions of these capsules and procedures for filing them are known among those skilled in drug formulations and manufacture. The encapsulating material should be highly soluble so that the particles are freed and rapidly dispersed in the stomach after the capsule is ingested.
[0348] In certain embodiments, the extract of O. stamineus leaves can comprise from 40% to 99% by weight of any one of the immediate release, normal release, or controlled
release matrix dry weight. For example, in certain embodiments the extract of O. stamineus leaves is present in an amount from 70% to 95% by weight of the matrix dry weight.
[0349] In some embodiments, formulations comprising the immediate release, normal release and controlled release matrices, comprise a pore former in the matrix to influence the rate of release of the extract of O. stamineus leaves from the matrix. The pore formers can be inorganic or organic, and can be particulate in nature and include materials that can be dissolved, extracted or leached from the matrix in the environment of use. Upon exposure to fluids in the environment of use, the pore-formers can, for example, dissolve, forming channels and pores that fill with the environmental fluid. For example, the pore- formers of certain embodiments of the matrix formulations can comprise one or more water-soluble hydrophilic polymers to modify the release characteristics of the formulation. Examples of suitable hydrophilic polymers used as pore-formers are well known in the art and have been described, for example, in U.S. Pat. No. 7,569,610.
[0350] The immediate release, normal release, or controlled release matrices comprising the extract of O. stamineus leaves can be prepared by various conventional mixing, comminution and fabrication techniques clear to those skilled in the chemistry of drug formulations. Examples of such techniques include: (1) Direct compression, using appropriate punches and dies, such as those available from Elizabeth Carbide Die Company, Inc., McKeesport, Pa., USA; the punches and dies are fitted to a suitable rotary tableting press, such as the Elizabeth-Hata single-sided Hata Auto Press machine, with either 15, 18 or 22 stations, and available from Elizabeth-Hata International, Inc., North Huntington, Pa., USA; (2) Injection or compression molding using suitable molds fitted to a compression unit, such as those available from Cincinnati Milacron, Plastics Machinery Division, Batavia, Ohio, USA.; (3) Granulation followed by compression; and (4) Extrusion in the form of a paste, into a mold or to an extrudate to be cut into lengths.
[0351] In regards to the swellable controlled release matrices, when microparticles are made by direct compression, the addition of lubricants can be helpful and sometimes important to promote powder flow and to prevent capping of the microparticle (breaking of a portion of the particle) when the pressure is relieved. Non-limiting examples of suitable lubricants include magnesium stearate (in a concentration of from 0.25% to 3% by weight, and in certain embodiments less than 1% by weight, in the powder mix), and hydrogenated vegetable oil (in certain embodiments hydrogenated and refined triglycerides of stearic and palmitic acids at 1% to 5% by weight, for example in at least one embodiment at 2% by weight). Additional excipients can be added to enhance powder flowability and reduce adherence.
[0352] Certain embodiments of the swellable controlled release matrices can find utility when administered to a subject who is in the digestive state (also referred to as the postprandial or "fed" mode). The postprandial mode is distinguishable from the
interdigestive (or "fasting") mode by their distinct patterns of gastroduodenal motor activity, which determine the gastric retention or gastric transit time of the stomach contents.
[0353] The controlled release matrices of the present invention can be manufactured by methods known in the art such as those described in the patents listed above (e.g. U.S. Pat. No. 5,965,161). An example of a method of manufacturing controlled release matrices is melt-extrusion of a mixture containing the extract of O. stamineus leaves, hydrophobic polymer(s), hydrophilic polymer(s), and optionally a binder, plasticizer, and other
excipient(s) as described above. Other examples of methods of manufacturing controlled release matrices include wet granulation, dry granulation (e.g. slugging, roller compaction), direct compression, melt granulation, and rotary granulation.
[0354] Additionally, controlled release matrices, which can be compressed or placed in capsules can be produced by combining the extract of O. stamineus leaves and a
hydrophobic fusible component and/or a diluent, optionally with a release modifying agent including a water soluble fusible material or a particulate soluble or insoluble organic or inorganic material. Examples of potential hydrophobic fusible components include hydrophobic materials such as natural or synthetic waxes or oils (e.g., hydrogenated vegetable oil, hydrogenated castor oil, microcrystalline wax, Beeswax, carnauba wax and glyceyl monostearate). In at least one embodiment the hydrophobic fusible component has a melting point from 35° C. to 140° C. Examples of release modifying agents include polyethylene glycol and particulate materials such as dicalcium phosphate and lactose.
[0355] In certain embodiments, controlled release matrices can be produced by mechanically working a mixture of the extract of O. stamineus leaves, a hydrophobic fusible component, and optionally a release component including a water soluble fusible material or a particulate soluble or insoluble organic or inorganic material under mixing conditions that yield agglomerates, breaking down the agglomerates to produce controlled release seeds having desired release properties; and optionally adding more carrier or diluent and repeating the mixing steps until controlled release matrices having desired release properties are obtained. These particles can also be size separated (e.g. by sieving and encapsulated in capsules or compressed into a matrix).
[0356] The amount of the hydrophobic fusible material used in the foregoing methods can range from 10% to 90% by weight. Mixers useful in such methods are known and include conventional high-speed mixers with stainless steel interiors. For example, a mixture can be processed until a bed temperature of 40°C or higher is realized, and the mixture achieves a cohesive granular texture comprising desired particle sizes.
[0357] As noted, if the mixture contains agglomerates, they can be broken down using conventional methods to produce a mixture of powder and particles of the desired size which, can be size-separated using a sieve, screen or mesh of the appropriate size. This material can be returned to a high-speed mixer and further processed as desired until the hydrophobic fusible materials begin to soften/melt, and optionally additional hydrophobic material can be added and mixing continued until particles having a desired size range are obtained. Still further, particles comprising the extract of O. stamineus leaves can be produced by melt processing as known in the art and combined into capsules or compressed into matrices.
[0358] The extract of O. stamineus leaves can be present in a therapeutically effective amount of from 0.1% to 99% by weight of the cores. For example, in certain embodiments the extract of O. stamineus leaves is present in an amount of from 0.1% to 90%, in other embodiments from 5% to 90%, in still other embodiments from 10% to 80%, and in even still other embodiments from 25% to 80% by weight of the core. A core can further comprise at least one other therapeutic agent. In certain embodiments, the one other therapeutic agent is an anti-angiogenic drug (e.g., bevacizumab, girentuximab, imatinib, dasatinib,
ramucirumab, axitinib, nilotinib, cabozantinib, ceritinib, lenvatinib, pazopanib, nintedanib, regorafenib, sorafenib, sunitinib, vandetanib, vatalanib, cetuximab, panitumumab,
trastuzumab, axitinib, erlotinib, temsirolimus, everolimus, sirolimus, ziv-aflibercept, interferon alfa, lenalidomide, palomid 529, thalidomide, TAS-102, rhEndostatin, AKB-977, isothiocyanates (e.g., 6-(Methylsulfinyl)hexyl isothiocyanate), extracts of Wasabia japonica, nitrogen mustard, nitrogen mustard-N-oxide hydrochloride, chlorambutyl,
cyclophosphamide, ifosfamide, thiotepa, carboquone, improsulfan tosylate, busulfan, nimustine hydrochloride, mitobronitol, melphalan, dacarbazine, ranimustine, estramustine phosphate sodium, triethylenemelamine, carmustine, lomustine, streptozocin, pipobroman, etoglucid, carboplatin, cisplatin, miboplatin, nedaplatin, oxaliplatin, altretamine, ambamustine, dibrospidium hydrochloride, fotemustine, prednimustine, pumitepa, ribomustin, temozolomide, treosulphan, trophosphamide, zinostatin stimalamer, carboquone, adozelesin, cystemustine, bizelesin, mercaptopurine, fenofibrate, 6- mercaptopurine riboside, thioinosine, methotrexate, enocitabine, cytarabine, cytarabine ocfosfate, ancitabine hydrochloride, 5-FU drugs, aminopterine, leucovorin calcium, tabloid, butocine, folinate calcium, levofolinate calcium, cladribine, emitefur, fludarabine, gemcitabine, hydroxycarbamide, pentostatin, piritrexim, idoxuridine, mitoguazone, thiazophrine, ambamustine, actinomycin-D, actinomycin-C, mitomycin-C, chromomycin-A3, bleomycin hydrochloride, bleomycin sulfate, peplomycin sulfate, daunorubicin
hydrochloride, doxorubicin hydrochloride, aclarubicin hydrochloride, pirarubicin
hydrochloride, epirubicin hydrochloride, neocarzinostatin, mithramycin, sarcomycin, carzinophilin, mitotane, zorubicin hydrochloride, mitoxantrone hydrochloride, idarubicin hydrochloride, etoposide phosphate, vinblastine sulfate, vincristine sulfate, vindesine sulfate, teniposide, paclitaxel, docetaxel, vinorelbine, picibanil, krestin, sizofiran, lentinan, ubenimex, interferons, interleukins, macrophage colony-stimulating factor, granulocyte colony-stimulating factor, erythropoietin, lymphotoxin, BCG vaccine, Corynebacterium parvum, levamisole, polysaccharide K, procodazole, alitretinoin, imiquimod, polyphenon E, vismodegib, sonidegib, pegaptanib, ranibizumab, sonepcizumab, volociximab, afilbercept, conbercept, fumagillin, JSM6427, AL-78898A, ARC1905, Bevasiranib, siRNA 027, siRNA PF04523655, AdGVPEDF.llD, RetinoStat, sFltOl, MA09-hRPE, PF-05206388, iPS-derived RPE sheet, AMDCELL, CD34+ BMSC, corticosteroid implants; antihistamines (e.g.,
dimenhydrinate, diphenhydramine, chlorpheniramine and dexchlorpheniramine maleate); analgesics (e.g., aspirin, codeine, morphine, dihydromorphone, oxycodone, etc.); nonsteroidal anti-inflammatory agents (e.g., NSAIDS, salicylate, aspirin, difunisal, salicylic acid, salsalate, propionic acid derivatives, ibuprofen, dexibuprofen, naproxen, fenoprofen, ketoprofen, dexketoprofen, flurbiprofen, oxaprozin, loxoprofen, acetic acid derivatives, indomethacin, tolmetin, sulindac, etodolac, ketorolac, diclofenac, aceclofenac, principal metabolite of nabumetone, enolic acid derivatives, piroxicam, meloxicam, tenoxicam, droxicam, lornoxicam, phenylbutazone, anthranilic acid derivatives, mefenamic acid, meclofenamic acid, flufenamic acid, tolfenamic acid, selective COX-2 inhibitors, celecoxib, parecoxib, lumiracoxib, etoricoxib, firocoxib, sulfonanilides, nimesulide, clonixine, licofelone, H-harpagide, corticosteroids, prednisone, Cortisol, prednisone, methylprednisolone, fludrocortisone, isoflupredone, triamicinolone, triamicinolone acetonide, dexamethasone, betamethasone, flumethasone); anti-emetics (e.g., metoclopramide); anti-epileptics (e.g., phenytoin, meprobamate and nitrezepam); antitussive agents and expectorants (e.g., codeine phosphate); antihyperglycemics (e.g., alpha-glucosidase inhibitors (e.g., acarbose), biguanides (e.g., metformin), DPP-4 inhibitors (e.g., alogliptin, linagliptin, sitagliptin,
saxagliptin), GLP-1 receptor agonists (e.g., albiglutide, exenatide, liraglutide), insulin and its analogues (e.g., bolus insulins, basal insulins, premixed insulins), insulin secretagogues (e.g., sulfonylureas, meglitinides), SGLT2 inhibitors (e.g., canagliflozin, dapagliflozin,
empagliflozin), TZDs (e.g., pioglitazone, rosiglitazone), and weight loss agents that inhibit lipase (e.g., orlistat)); anti-asthmatics (e.g. theophylline), antacids; anti-spasmodics (e.g. atropine, scopolamine); diuretics (e.g., ethacrynic acid, bendrofluazide); anti-hypotensives (e.g., propranolol, clonidine); antihypertensives (e.g, diuretics (e.g., chlorthalidone, chlorothiazide, furosemide, hydrochlorothiazide, indapamide, metolazone, amiloride hydrochloride, spironolactone, triamterene, bumetanide), beta-blockers (e.g., acebutolol, atenolol, betaxolol, bisoprolol fumarate, carteolol, metoprolol, nadolol, penbutolol, pindolol, propranolol, sotalol, timolol), ACE inhibitors (e.g., benazepril, captopril, enalapril, fosinopril, Lisinopril, moexipril, perindopril, quinapril, ramipril, trandolapril), Angiotensin II receptor blockers (e.g., candesartan, eprosartan, irbesartan, losartan, telmisartan, valsartan), calcium channel blockers (e.g., amlodipine, bepridil, diltiazem, felodipine, isradipine, nicardipine, nifedipine, nisoldipine, verapamil), alpha blockers (e.g., doxazosin, prazosin, terazosin), alpha-2 receptor agonists (e.g., methyldopa), central agonists (e.g., methyldopa, clonidine, guanabenz, guanfacine), peripheral adrenergic inhibitors (e.g., guanadrel, guanethidine, reserpine), and vasodilators (e.g., nifedipine, papaverine, diltiazem, nicardipine, hydralazine, minoxidil)); bronchodilators (e.g., albuterol); steroids (e.g., hydrocortisone, triamcinolone, prednisone); antibiotics (e.g., tetracycline); anti-hemorrhoidals; hypnotics; psychotropics; anti-diarrheals, mucolytics; sedatives; decongestants; laxatives; vitamins; stimulants (including appetite suppressants such as phenylpropanolamine); neuroprotective agents or anti-neurodegenerative agents (e.g., dabigatran, apixaban, rivaroxaban, aspirin, carbidopa- levodopa, dopamine agonists (e.g., pramipexole, ropinirole, rotigotine, apomorphine), MAO- B inhibitors (e.g., selegiline, rasagiline), COMT inhibitors (e.g., entacapone, tolcapone), anticholinergics (e.g., benztropine, trihexyphenidyl), amantadine, cholinesterase inhibitors (e.g., donepezil, galantamine, rivastigmine), antioxidants, curcumin, crocin, erythropoietin, omega-3 fatty acids, lithium, minocycline, nicotine, pyrroloquinoline quinone, resveratrol, vinpocetine, progesterone, statins, noopept, L-theanine, estrogen, caspase inhibitors, cannabinoids, bacopa monnieri, anti-protein aggregation agents (e.g., sodium 4- phenylbutyrate, trehalose, and polyQ-binding peptide), acetylcysteine, acetyl-L-carnitine, caffeine, and memantine); anti-acne agents; agents used to treat rosacea; anesthetics; anorectals; anti-fungals; anti-microbials; scabicides; pediculicides; antiperspirants;
antipruritics; antipsoriatic agents; antiseborrheic agents; biologically active proteins and peptides; burn treatment agent; cauterizing agent; depigmenting agents; depilatories;
diaper rash treatment agents; enzymes; hair growth stimulants; hair growth retardants including DFMO and its salts and analogs; hemostatics; keratolytics; canker sore treatment agents; cold sore treatment agents; dental and periodontal treatment agents;
photosensitizing actives; dermal protectant/barrier agents; sunburn treatment agents; sunscreens; transdermal actives; nasal actives; vaginal actives; wart treatment agents;
wound treatment agents, wound healing agents; as well as pharmaceutically acceptable salts, hydrates, solvates, or prodrug forms of the same. Combinations are permissible, providing administration of the combinations are not contraindicated. The above list is not meant to be exclusive.
[0359] In certain embodiments, the immediate release, normal release matrix or
controlled release matrix cores can be coated with at least one functional or non-functional coat, or an immediate release coating optionally comprising the extract of O. stamineus leaves or another drug. Functional coatings include by way of example controlled release polymeric coatings, enteric polymeric coatings, moisture barrier coats, taste masked coates, and coats that preclude dose dumping in specific media such as alcohol. Non-functional coatings are coatings that do not affect drug release but which affect other properties (e.g., they can enhance the chemical, biological, or the physical appearance of the final dosage form).
[0360] In one embodiment, the cores comprising the extract of O. stamineus leaves can be coated with a moisture barrier to imdpede or retard absorption of moisture and maintain stability and hence prolong shelf life of the extract of O. stamineus leaves. The moisture barrier can be applied directly onto the sieved or unsieved powder, granules, an immediate release core, a normal release matrix core, or a controlled release matrix core.
[0361] The moisture barrier typically comprises an enteric polymer (e.g. acrylic polymer), a permeation enhancer and optionally a plasticizer.
[0362] In certain embodiments, the enteric polymer is an acrylic polymer. For example, the acrylic polymer can be a methacrylic acid copolymer type C (poly(methacrylic acid, methyl methacrylate) 1:1) available commercially under the trade name EUD AGIT® (e.g. Eudragit L 30 D-55). The methacrylic acid copolymer can be present in an amount, which can vary from 1% to 3% of the matrix dry weight and from 55% to 70% of the moisture barrier dry weight.
[0363] It is known in the art that methacrylic acid copolymers can become brittle, and that coatings that contain methacrylic acid copolymers could be made more elastic and pliable by the addition of a plasticizer. In certain embodiments, the moisture barrier coat comprises a plasticizer. Non-limiting examples of plasticizers useful for the moisture barrier coat described herein are well known in the art and have been described, for example, in U.S. Pat. No. 7,569,610. The plasticizer can be present in an amount which can vary from 0.2% to 0.5%. For example, in certain embodiments the plasticizer is present in an amount of from 0.2% to 0.4% of the matrix dry weight. With respect to the moisture barrier itself, the plasticizer, if present, can be present in an amount of from 1% to 30% by weight of the moisture barrier dry weight. It is well known in the art that depending on the intended main function, excipients to be used in formulations are subcategorized into different groups. However, one excipient can affect the properties of an API or the formulation in a series of ways, and many substances used in pharmaceutical formulations can therefore be described as multifunctional. Thus, in one embodiment, the polyethylene glycol used as a plasticizer, or in combination with another other plasticizer(s) for the moisture barrier can serve not only to increase the hydrophilicity of the moisture barrier, but can also act as a glidant.
[0364] The moisture barrier can further comprise a permeation enhancer that can increase its hydrophilicity, and can also act as a glidant. The permeation enhancers are well known in the art and have been described, for example, in U.S. Pat. No. 7,569,610. In at least one embodiment of the invention the permeation enhancer is silicon dioxide (e.g. SYLOID® 244FP). The amount of permeation enhancer can vary from 0.5% to 1% (e.g., 0.5, 0.55, 0.6, 0.65, 0.7, 0.75, 0.8, 0.85, 0.9, 0.95, or 1%) by weight of the matrix dry weight or from 25% to 30% (e.g., 25, 25.5, 26, 26.5, 27, 27.5, 28, 29.5, or 30%) by weight of the moisture barrier dry weight.
[0365] The moisture barrier as used herein, if present, typically does not function as an enteric coat. Even though the methacrylic acid copolymer, EUDRAGIT® L30D-55, is used in enteric coating formulations in the art, its functionality is formulation dependent and on the quantity of the material applied. As is known in the art, an enteric coating is applied where a drug can be destroyed or inactivated by gastric juice or where the drug can irritate the gastric mucosa. To meet the requirements for an enteric coat, the test as described in the USP (method A or B) stipulates that after 2 hours in acidic media (0.1N HCI), no individual values of at least six experiments exceed 10% of the active drug dissolved and not less than 75% of the active drug dissolved at 45 minutes in pH 6.8. The moisture barrier typically does not meet this requirement for the following reasons: (1) to obtain enteric integrity with a film containing EUDRAGIT® L30D-55, a weight gain of between 6% to 8% based on the dry polymer per dosage unit is recommended. To function as a moisture barrier, the amount of EUDRAGIT® L30D-55 applied onto the matrix cores should not be more than 6%, and in at least one embodiment, should not be more than 3%, (2) if enteric integrity would be required, the dissolution test for the finished product (i.e., the moisture barrier coated cores) at the 2 hour time point would not stipulate a limit of no more than 10%, and (3) analytical tests performed on these coatings indicate that the coatings do not meet all the test requirements as an enteric coated product as defined by USP test methods.
[0366] In at least one embodiment, the granules, immediate release, normal release or controlled release matrix cores can each be coated with a controlled release polymeric coating (or control-releasing coat) comprising an acrylic polymer. Suitable acrylic polymers are well known in the art and have been described, for example, in U.S. Pat. No. 7,569,610.
[0367] In at least one embodiment polymerizable quaternary ammonium compounds can be employed in the control releasing coat. Examples of suitable polymerizable quaternary ammonium compounds are well known in the art and have been described, for example, in U.S. Pat. No. 7,569,610.
[0368] In at least one embodiment the acrylic polymer can comprise one or more ammonio methacrylate copolymers. Ammonio methacrylate copolymers (such as those sold under the Trademark EUDRAGIT® RS and RL) are described in National Formulary (NF) XVII as fully polymerized copolymers of acrylic and methacrylic acid esters with a low content of quaternary ammonium groups. To obtain a desirable dissolution profile for a given therapeutically active agent, such as the extract of O. stamineus leaves, two or more ammonio methacrylate copolymers having differing physical properties can be incorporated. For example, it is known that by changing the molar ratio of the quaternary ammonium groups to the neutral (meth)acrylic esters, the permeability properties of the resultant coating can be modified.
[0369] In other embodiments, the control releasing coat can further comprise a polymer whose permeability is pH dependent, such as anionic polymers synthesized from methacrylic acid and methacrylic acid methyl ester. Such polymers are commercially available, e.g., from Rohm Pharma GmbH under the tradename EUDRAGIT® L and
EUDRAGIT® S. The ratio of free carboxyl groups to the esters is known to be 1:1 in
EUDRAGIT® L and 1:2 in EUDRAGIT® S. EUDRAGIT® L is insoluble in acids and pure water, but becomes increasingly permeable above pH 5.0. EUDRAGIT® S is similar, except that it becomes increasingly permeable above pH 7. The hydrophobic acrylic polymer coatings can also include a polymer which is cationic in character based on dimethylaminoethyl
methacrylate and neutral methacrylic acid esters (such as EUDRAGIT® E, commercially available from Rohm Pharma). The hydrophobic acrylic polymer coatings of the present invention can further include a neutral copolymer based on poly (meth)acrylates, such as EUDRAGIT® NE (NE=neutral ester), commercially available from Rohm Pharma. EUDRAGIT® NE 30D lacquer films are insoluble in water and digestive fluids, but permeable and swellable.
[0370] In at least one other embodiment, the control releasing coat comprises a dispersion of poly (ethylacrylate, methyl methacrylate) 2:1 (KOLLICOAT® EMM 30 D, BASF).
[0371] In at least one other embodiment, the control releasing coat can comprise a polyvinyl acetate stabilized with polyvinylpyrrolidone and sodium lauryl sulfate such as KOLLICOAT® SR30D (BASF). The dissolution profile can be altered by changing the relative amounts of different acrylic resin lacquers included in the coating. Also, by changing the molar ratio of polymerizable permeability-enhancing agent (e.g., the quaternary ammonium compounds) to the neutral (meth)acrylic esters, the permeability properties (and thus the dissolution profile) of the resultant coating can be modified.
[0372] In at least one embodiment, the control releasing coat can comprise ethylcellulose, which can be used as a dry polymer (such as ETHOCEL®, Dow Coming) solubilised in organic solvent prior to use, or as an aqueous dispersion. One suitable commercially-available aqueous dispersion of ethylcellulose is AQUACOAT® (FMC Corp., Philadelphia, Pa., U.S.A.). AQUACOAT® can be prepared by dissolving the ethylcellulose in a water-immiscible organic solvent and then emulsifying the same in water in the presence of a surfactant and a stabilizer. After homogenization to generate submicron droplets, the organic solvent is evaporated under vacuum to form a pseudolatex. The plasticizer is not incorporated in the pseudolatex during the manufacturing phase. Thus, prior to using the same as a coating, the AQUACOAT® can be intimately mixed with a suitable plasticizer prior to use. Another suitable aqueous dispersion of ethylcellulose is commercially available as SURELEASE® (Colorcon, Inc., West Point, Pa., U.S.A.). This product can be prepared by incorporating plasticizer into the dispersion during the manufacturing process. A hot melt of a polymer, plasticizer (e.g. dibutyl sebacate), and stabilizer (e.g. oleic acid) is prepared as a homogeneous mixture, which is then diluted with an alkaline solution to obtain an aqueous dispersion which can be applied directly onto substrates.
[0373] In one embodiment, the control releasing coat can comprise an extended release semipermeable coat comprising a water-insoluble, water-permeable film-forming polymer, optionally a water-soluble polymer, and optionally a plasticizer.
[0374] Non-limiting examples of water-insoluble, water-permeable film-forming polymers useful for the extended release semipermeable coat include cellulose ethers, cellulose esters, and polyvinyl alcohol. For example, the water-insoluble, water-permeable film forming polymers can be the ethyl celluloses, and can be selected from the following: ethyl cellulose grades PR100, PR45, PR20, PR10 and PR7 (ETHOCEL®, Dow), and any combination thereof. The amount of the water-insoluble water-permeable film-forming polymer can vary from 1% to 12% (e.g., 1%, 2%, 3%, 4%, 5%, 6%, 7%, 8%, 9%, 10%, 11% or 12%) by weight of the core dry weight. Non-limiting examples of water-soluble polymers useful for the extended release semipermeable coat are well known in the art and have been described, for example, in U.S. Pat. No. 7,569,610. The amount of water-soluble polymer can vary from 1.5% to 10% (e.g., 1.5%, 2%, 2.5%, 3%, 3.5%, 4%, 4.5%, 5%, 5.5%, 6%,
6.5%, 7%, 7.5%, 8%, 8.5%, 9%, 9.5% or 10%) by weight of the core dry weight. With respect to the control-releasing coat itself, in certain embodiments the amount of water-soluble polymer present is from 25% to 55% (e.g., 25%, 30%, 35%, 40%, 45%, 50% or 55%) by weight of the extended release semipermeable coat dry weight.
[0375] In certain embodiments, the extended release semipermeable coat can further comprise a plasticizer. The use of plasticizers is optional, and the can be added to film coating formulations to modify the physical properties of a polymer to make it more usable during manufacturing. Plasticizers can be high boiling point organic solvents used to impart flexibility to otherwise hard or brittle polymeric materials. Plasticizers generally cause a reduction in the cohesive intermolecular forces along the polymer chains resulting in various changes in polymer properties including a reduction in tensile strength, and increase in elongation and a reduction in the glass transition or softening temperature of the polymer. The amount and choice of the plasticizer can affect the hardness of a tablet and can even affect its dissolution or disintegration characteristics, as well as its physical and chemical stability. Certain plasticizers can increase the elasticity and/or pliability of a coat, thereby decreasing the coat's brittleness. Once the dosage form is manufactured, certain plasticizers can function to increase the hydrophilicity of the coat(s) and/or the core of the dosage form in the environment of use (in-vitro or in-vivo). Examples of plasticizers that can be used in extended release semipermeable coats are well known in the art and have been described, for example, in U.S. Pat. No. 7,569,610. It is contemplated and within the scope of the invention, that a combination of plasticizers can be used. The amount of plasticizer for the extended release semipermeable coat can vary in an amount of from 0.5% to 4% (e.g., 0.5, 0.6, 0.7, 0.8, 0.9, 1, 1.5, 2, 2.5, 3, 3.5, or 4%) by weight of the core dry weight.
[0376] The ratio of water-insoluble water-permeable film forming polymer to plasticizer to water-soluble polymer for the extended release semipermeable coat can vary from 3:1:4 to 5:1:2. For certain embodiments, the ratio of the water-insoluble water- impermeable film-forming polymer to plasticizer to water-soluble polymer can be from 7:2:6 to 19:5:18. In at least one embodiment the ratio of water-insoluble water-permeable film forming polymer to plasticizer to water-soluble polymer can be 13:4:12.
[0377] The skilled person will appreciate that controlling the permeability and/or the amount of coating applied to the cores can control the release of the extract of O. stamineus leaves from within the cores. The rate or release of the extract of O. stamineus leaves can be altered by varying the ratio of the water-insoluble, water-permeable film-forming polymer to plasticizer to water-soluble polymer and/or the quantity of coating applied to the core. A more extended release can be obtained with a higher amount of water-insoluble, water- permeable film forming polymer. The addition of other excipients to the core, as described herein, can also alter the effectiveness of the extended release semipermeable coat. For example, if it is desired that the core further comprises an expanding agent, the amount of plasticizer in the extended release semipermeable coat could be increased to make the coat more pliable, as the pressure exerted on a less pliable coat by the expanding agent could rupture the coat. Further, the proportion of the water-insoluble water-permeable film forming polymer and water-soluble polymer can also be altered depending on whether a faster or slower dissolution and/or release profile is desired.
[0378] In certain embodiments, the controlled release coat can comprise an aqueous dispersion of a neutral ester copolymer without any functional groups, a poly glycol having a
melting point greater than 55° C, and one or more pharmaceutically acceptable excipients ("aqueous controlled release coat"); wherein said coating composition is coated onto the dosage form and cured at a temperature at least equal to or greater than the melting point of the poly glycol. The aqueous controlled release coating formulation is quite versatile in that it can be easily manipulated to obtain the desired drug release profile. In certain such embodiments, the aqueous controlled release coat comprises an aqueous dispersion of an ethylcellulose, a poly glycol having a melting point greater than 55° C, and one or more pharmaceutically acceptable excipients; wherein said coating composition is coated onto the cores and cured at a temperature at least equal to or greater than the melting point of the poly glycol. Non-limiting examples of aqueous dispersions of an ethylcellulose include SURELEASE® (Colorcon, Inc., West Point, Pa., U.S.A.), and AQUACOAT® (FMC Corp.,
Philadelphia, Pa., U.S.A.). Non-limiting examples of neutral ester copolymers without any functional groups that can be used in this control-releasing coat include EUDRAGIT® NE30D, EUDRAGIT® NE40D (Rohm America LLC), and mixtures thereof. In at least one embodiment, the polymer is Eudragit NE30D, which can be present in an amount of from 1% to 35% (e.g., 1, 2, 3, 4, 5, 6, 7, 8, 9, 10, 12, 14, 16, 18, 20, 22, 24, 26, 28, 30, 32 or 35%) by weight of the aqueous controlled release coat, depending on the controlled release profile desired.
Hydrophilic agents can also be included in the aqueous controlled release coat to promote wetting of the coat when in contact with gastrointestinal fluids. Non-limiting examples of such hydrophilic agents include hydrophilic water soluble polymers such as hydroxypropyl methylcellulose (HPMC), hydroxypropyl cellulose (HPC) and combinations thereof. In at least one embodiment, HPMC can be the hydrophilic water soluble polymer. If hydrophilic agents are to be included in the coat composition, the agents can be present in an amount from 0.1% to 10% (e.g., 0.1, 0.2, 0.3, 0.4, 0.5, 0.6, 0.7, 0.8, 0.9, 1, 1.5, 2, 2.5, 3, 3.5, 4, 4.5, 5, 5.5, 6, 6.5, 7, 7.5, 8, 8.5, 9, 9.5 or 10%) by weight of the coating composition.
[0379] The aqueous controlled release coat can also comprise a polyglycol with a melting point of greater than 55° C. Non-limiting examples of the polyglycol include polyethylene glycol 6000, polyethylene glycol 8000, polyethylene glycol 10000, polyethylene glycol 20000, and mixtures thereof. In at least one embodiment, the poly glycol is polyethylene glycol 8000. The poly glycol can be present in an amount of from 0.1% to 5% by weight of the coat. Other examples of suitable polyglycol derivatives having a melting point of at least 55°C include, but are not limited to, Poloxamer 188, Poloxamer 338, Poloxamer 407, Polyethylene Oxides, Polyoxyethylene Alkyl Ethers, and Polyoxyethylene Stearates.
[0380] In at least one embodiment, the cores can be coated with polymers to facilitate mucoadhesion within the gastrointestinal tract. Non-limiting examples of polymers that can be used for mucoadhesion include carboxymethylcellulose, polyacrylic acid, CARBOPOL™, POLYCARBOPHIL™, gelatin and other natural or synthetic polymers.
[0381] In at least one embodiment, the cores, comprising the extract of O. stamineus leaves can each be coated with at least one taste-masking coating. The taste-masking coating can mask the taste of the extract of O. stamineus leaves in the cores or in the coats comprising the extract of the O. stamineus leaves. In at least one embodiment the taste- masking coating formulations can contain polymeric ingredients. Suitable polymeric ingredients comprising taste-masking coatings are well known in the art and have been described, for example, in U.S. Pat. No. 7,569,610. The taste-masking coatings can be applied to the matrices from one or more organic or aqueous solvent solutions or suspensions. In at
least one embodiment, the organic solvents that can be used to apply the taste-masking coatings include one or more of acetone, lower alcohols such as EtOH, isopropanol and alcohol/water mixtures, chlorinated hydrocarbons, and the like. Devices used to coat the matrices of the invention with a taste-masking coating include those conventionally used in pharmaceutical processing, such as fluidized bed coating devices. The control-releasing coatings applied to the matrices can contain ingredients other than the cellulosic polymers. One or more colorants, flavourants, sweeteners, can also be used in the taste-masking coating.
[0382] Any one of the coatings described herein can comprise a colorant. Colorants in the film coat formula can be water-insoluble colors (pigments). Pigments have certain advantages over water-soluble colors in that they tend to be more chemically stable towards light, provide better opacity and covering power, and optimize the impermeability of a given film to water vapor. Non-limiting examples of suitable colorants include iron oxide pigments, titanium dioxide, and aluminum lakes. Mixtures are operable. In at least one embodiment the pigment is titanium dioxide. The pigment or colorant can be present in an amount of from 0.1% to 10% (e.g., 0.1, 0.2, 0.3, 0.4, 0.5, 0.6, 0.7, 0.8, 0.9, 1, 2, 3, 4, 5, 6, 7, 8, 9, or 10%) by weight of the coat composition.
[0383] In certain embodiments, flavourants can be used in the coatings described herein, which can also function to taste-mask the extract of O. stamineus leaves. Examples of flavourants include natural and synthetic flavoring liquids. An illustrative list of such flavourants includes volatile oils, synthetic flavor oils, flavoring aromatics, oils, liquids, oleoresins and extracts derived from plants, leaves, flowers, fruits, stems and combinations thereof (e.g., citric oils, such as lemon, orange, grape, lime and grapefruit, and fruit essences, including apple, pear, peach, grape, strawberry, raspberry, cherry, plum, pineapple, apricot, or other fruit flavors). Other useful flavourants include aldehydes and esters, such as benzaldehyde (cherry, almond); citral, i.e., alpha-citral (lemon, lime); neral, i.e., beta-citral (lemon, lime); decanal (orange, lemon); aldehyde C-8 (citrus fruits); aldehyde C-9 (citrus fruits); aldehyde C-12 (citrus fruits); tolyl aldehyde (cherry, almond); 2,6- dimethyloctanal (green fruit); 2-dodenal (citrus mandarin); mixtures thereof and the like.
[0384] In certain embodiments, the coatings described herein can comprise sweeteners, which can also function as taste masking agents. Examples of such sweeteners include glucose (corn syrup), dextrose, invert sugar, fructose, and mixtures thereof (when not used as a carrier); saccharin and its various salts, such as sodium salt; dipeptide sweeteners such as aspartame; dihydrochalcone compounds, glycyrrhizin; Steva Rebaudiana (Stevioside); chloro derivatives or sucrose such as sucralose; and sugar alcohols such as sorbitol, mannitol, xylitol, and the like. Also contemplated are hydrogenated starch hydrolysates and the synthetic sweeteners such as 3,6-dihydro-6-methyl-l-l-l,2,3- oxathiazin-4-l-2,2-dioxide, particularly the potassium salt (acesulfame-K), and sodium and calcium salts thereof. The sweeteners can be used alone or in any combination thereof.
[0385] In some embodiments, any one of the functional or nonfunctional coats described herein can comprise a pore former to influence the rate of release of the extract of O. stamineus leaves from the core. The pore formers can be inorganic or organic, and can be particulate in nature and include materials that can be dissolved, extracted or leached from the coating in the environment of use. Upon exposure to fluids in the environment of use, the pore-formers can dissolve and form pores or channels that fill with the
environmental fluid. Non-limiting examples of pore formers suitable for use in the controlled release coats described herein include the pore formers described above for use in the immediate release, normal release or controlled release matrices.
[0386] Any one of the functional or non-functional coats described herein can further comprise at least one pharmaceutically acceptable excipient. The excipients can include but are not limited to anti-tacking agents, emulsifying agents, antifoaming agents, flavourants, colourants, etc. It is known in the art that depending on the intended main function, excipients can affect the properties of the coat in a series of ways, and many substances used in coat formulations can thus be described as multifunctional. A skilled person will know, based on his/her technical knowledge, which pharmaceutically acceptable excipients are suitable for the desired control releasing coat composition.
[0387] The tackiness of polymeric films is a factor for the coating of solid dosage forms and for the subsequent curing step (post coating thermal treatment). During coating with either cellulosic or acrylic polymers, sometimes an unwanted, and in other times irreversible agglomeration of several granules or beads or, in the worst case, of the complete batch, can occur, especially at higher product processing temperatures. Accordingly, the addition of anti-tacking agents to coating formulations can be desirable. The anti-tacking agents which can be used include but are not limited to adipic acid, magnesium stearate, calcium stearate, zinc stearate, hydrogenated vegetable oils, sterotex, glyceryl monostearate, talc, sodium benzoate, sodium lauryl sulfate, magnesium lauryl sulfate, and mixtures thereof. In at least one embodiment, talc can be the anti-tacking agent. Talc can also function as a wetting agent. Mixtures of anti-tacking agents are operable. The amount of anti-tacking agent in coat composition can be in the range from 1% to 15% (e.g., 1, 2, 3, 4, 5, 6, 7, 8, 9, 10, 11, 12 or 13%) by weight of the control-releasing coating dispersion.
[0388] The anti-foaming agents, which can be included in the coat compositions include silicone oil, simethicone, and mixtures thereof. In at least one embodiment, simethicone can be the anti-foaming agent. The anti-foaming agent can be present in an amount of up to 0.5% (e.g., 0, 0.1, 0.2, 0.3, 0.4, or 0.5%) by weight of the coat composition.
[0389] The emulsifying agent(s) (also called emulsifiers or emulgents) can be included to facilitate emulsification during manufacture of the coat compositions described herein, and to provide emulsion stability during the shelf-life of the product. Non-limiting examples of emulsifying agents include naturally occurring materials and their semi-synthetic derivatives, such as the polysaccharides, as well as glycerol esters, cellulose ethers, sorbitan esters and polysorbates. Mixtures are operable. The emulsifying agent(s) can be present in an amount of up to 0.5% (e.g., 0, 0.1, 0.2, 0.3, 0.4, or 0.5%) by weight of the coat composition.
[0390] In certain embodiments, the coats described herein can comprise the extract of O. stamineus leaves or another drug for immediate release. Examples of other drugs, include, without limitation, anti-angiogenics, anti-histamines, analgesics, non-steroidal anti- inflammatory agents, anti-emetics, anti-epileptics, anti-tussive agents and expectorants, antihyperglycemics, anti-asthmatics, antacids, anti-spasmodics, diuretics, anti-hypotensives, antihypertensives, bronchodilators, steroids, anti-biotics, anti-hemorrhoidals, hypnotics, psychotropics, anti-diarrheals, mucolytics, sedatives, decongestants, laxatives, vitamins, stimulants, neuroprotective agents anti-neurodegenerative agents, anti-acne agents, anti- fungals, anti-microbials, biologically active proteins and peptides, enzymes, Combinations of
other drugs are permissible, providing administration of the combinations are not contraindicated. The above list is not meant to be exclusive.
[0391] Methods of manufacturing the coats and applying the coats to cores are well known in the art and can be found, for example in (144).
[0392] The coats described herein can be used individually or in combination depending on the desired release rate. Also, in the manufacture of embodiments that have a moisture barrier and/or taste masking coat, the controlled release coat is dried before the moisture barrier and/or taste-masking coat is applied. The coats described herein are not exclusive.
[0393] The cores, either coated or uncoated, can be formulated into monolithic or multiparticulate dosage forms. In certain embodiments, the cores, either coated or uncoated, can be formulated into tablets, mini tablets (which can be encapsulated), microparticles (which can be encapsulated), or filled into sachets. Capsules, for example, can be filled with a combination of immediate release and controlled release microparticles or mini tablets. Capsules can also be filled with a combination of microparticles comprising the extract of O. stamineus leaves and microparticles comprising another therapeutic agent.
[0394] In certain embodiments, the pharmaceutically acceptable excipient comprises β-Cyclodextrin. Thus, certain embodiments provide for formulations comprising a therapeutically effective amount of the extract of O. stamineus leaves and β-cyclodextrin. In certain embodiments, the ratio of the extract of the O. stamineus leaves to β-Cyclodextrin is from 1:0.5 to 1:6 (wt/wt) (e.g., 1:0.5, 1:1, 1:1.5, 1:2, 1:2.5, 1:3, 1:3.5, 1:4, 1:4.5, 1:5, 1:5.5, or 1:6). In certain embodiments, the β-Cyclodextrin is at least 0.5 times (wt/wt) the amount of the extract of O. stamineus leaves. In certain embodiments, the β-Cyclodextrin is 2.5 times (wt/wt) the amount of the extract of O. stamineus leaves.
[0395] In certain embodiments, this formulation can be formulated into granules, immediate release, normal matrix, or controlled release matrix cores, each of which can optionally be coated with any one or more of the coats described herein.
[0396] In certain embodiments, the formulations comprise a therapeutically effective amount of the extract of O. stamineus leaves and a soluble polymer. In certain
embodiments, the soluble polymer is poly(ethylene glycol), polyvinylpyrrolidone, polyvinyl alcohol, polyacrylic acid, polyacrylamides, N-(2-Hydroxypropyl) methacrylamide, divinyl ether-maleic anhydride, polyoxazoline, polyphosphates, polyphosphazenes, xanthan gum, pectins, chitosan derivatives, dextran, carrageenan, guar gum, cellulose ethers, hyaluronic acid, albumin, starch, starch based derivatives, or any combination thereof. In certain embodiments, the ratio of the extract of the O. stamineus leaves to the soluble polymer is 1:1 (wt/wt). In certain embodiments, the soluble polymer can be polyvinylpyrrolidone.
[0397] In certain embodiments, the formulations comprise a therapeutically effective amount of the extract of O. stamineus leaves and a poloxamer. Non-limiting examples of suitable poloxamers include PLURONIC
® 10R5, PLURONIC
® 17R2, PLURONIC
® 17R4, PLURONIC
® 25R2, PLURONIC
® 25R4, PLURONIC
® 31R1, PLURONIC
® F 108 Cast Solid Surfacta, PLURONIC
® F 108 NF, PLURONIC
® F 108 Pastille, PLURONIC
® F 108 Prill, PLURONIC
® F 108NF Prill Poloxamer 338, PLURONIC
® F 127, PLURONIC
® F 127 Prill, PLURONIC
® F 127 NF, PLURONIC
® F 127 NF 500 BHT Prill, PLURONIC
® F 127 NF Prill Poloxamer 407, PLURONIC
® F 38, PLURONIC
® F 38 Pastille, PLURONIC
® F 68, PLURONIC
® F 68 Pastille, PLURONIC
® F 68 LF Pastille, PLURONIC
® F 68 NF, PLURONIC
® F 68 NF Prill Poloxamer 188, PLURONIC
® F 68 Prill,
PLURONIC
® F 77, PLURONIC
® F 77 Micropastille, PLURONIC
® F 87, PLURONIC
® F 87 NF, PLURONIC
® F 87 NF Prill Poloxamer 237, PLURONIC
® F 87 Prill, PLURONIC
® F 88, PLURONIC
® F 88 Pastille, PLURONIC
® F 88 Prill, PLURONIC
® F 98, PLURONIC
® F 98, PLURONIC
® F 98 Prill, PLURONIC
® L 10, PLURONIC
® L 101, PLURONIC
® L 121, PLURONIC
® L 31, PLURONIC
® L 35, PLURONIC
® L 43, PLURONIC
® L 44, PLURONIC
® L 61, PLURONIC
® L 62, PLURONIC
® L 62 LF, PLURONIC
® L 62D, PLURONIC
® L 64, PLURONIC
® L 81, PLURONIC
® L 92, PLURONIC
® L44 NF INH surfactant Poloxamer 124, PLURONIC
® N 3, PLURONIC
® P 103, PLURONIC
® P 104, PLURONIC
® P 105, PLURONIC
® P 123 Surfactant, PLURONIC
® P 65, PLURONIC
® P 84, PLURONIC
® P 85, and combinations thereof. In certain embodiments, the ratio of the extract of the O. stamineus leaves to the poloxamer is 1:1 (wt/wt). In at least one embodiment, the poloxamer can be PLU RON IC
® F 68
In at least one other embodiment, the poloxamer can be PLURONIC
® F 127
[0398] In certain embodiments, a therapeutically effective amount of the extract of O. stamineus leaves can be formulated together with a combination of a soluble polymer and a poloxamer. In certain embodiments, the ratio of the extract of O. stamineus leaves to the soluble polymer to the poloxamer is 2:1:1 (wt/wt/wt). In certain embodiments, the soluble polymer can be polyvinylpyrrolidone and the poloxamer can be PLURONIC® F 68,
PLURONIC® F 127, or any combination thereof. In certain embodiments, the poloxamer can be PLURONIC® F 68. In certain other embodiments, the poloxamer can be PLURONIC® F 127.
[0399] In certain embodiments, the formulations can comprise a combination of a therapeutically effective amount of the extract of the O. stamineus leaves, a soluble polymer and a first and second poloxamer, wherein the first and second poloxamers are different and wherein the ratio of said extract to the soluble polymer to the first poloxamer to the second poloxamer can be 2:1:1:1 (wt/wt/wt/wt). In at least one embodiment, the soluble polymer can be polyvinylpyrrolidone, the first poloxamer can be PLURONIC® F 68 and the second poloxamer can be PLURONIC® F 127.
[0400] Certain embodiments for manufacturing formulations comprising the extract of O. stamineus leaves in combination with at least one poloxamer and PVP is illustrated in Example 31.
[0401] In certain embodiments, the formulations can comprise: (a) a therapeutically effective amount of the extract of the O. stamineus leaves, (b) an effervescent couple, (c) an anti-caking agent, and (d) a taste masking agent. In certain other embodiments, the formulation comprises, by weight based on the total weight of the formulation, (a) 8% - 17% extract of the O. stamineus leaves (e.g., 8, 8.5, 9, 9.5, 10, 10.5, 11, 11.5, 12, 12.5, 13, 13.5, 14, 14.5, 15, 15.5, 16, 16.5 or 17%), (b) 30% - 80% effervescent couple (e.g., 30, 35, 40, 45, 50, 55, 60, 65, 70, 75, or 80%), (c) 0.5% - 2% anti-caking agent (e.g., 0.5, 0.6, 0.7, 0.8, 0.9, 1, 1.1, 1.2, 1.3, 1.4, 1.5, 1.6, 1.7, 1.8, 1.9 or 2%),and (d) 14% - 50% taste masking agent (e.g., 14, 16, 18, 20, 22, 24, 26, 28, 30, 32, 34, 36, 38, 40, 42, 44, 46, 48, or 50%). In certain embodiments, the effervescent couple comprises, an acidic component and an alkaline component. Non-limiting examples of the acidic component include anhydrous citric acid, tartaric acid, sodium gluconate, trisodium citrate, fumaric acid, malic acid, adipic acid, or any combination thereof. Non-limiting examples of the alkaline component include anhydrous sodium, potassium, calcium bicarbonates, sodium glycine carbonates, or any combination thereof. In certain embodiments, the effervescent couple can be anhydrous sodium bicarbonate and anhydrous citric acid. Non-limiting examples of the anti-caking agent
include magnesium aluminometasilicate, tricalcium phosphate, powdered cellulose, magnesium stearate, sodium bicarbonate, sodium ferrocyanide, potassium ferrocyanide, calcium ferrocyanide, bone phosphate, sodium silicate, silicon dioxide, calcium silicate, magnesium trisilicate, talcum powder, sodium aluminosilicate, potassium aluminium silicate, calcium aluminosilicate, bentonite, aluminium silicate, stearic acid, polydimethylsiloxane, or any combination thereof. In certain embodiments, the anti-caking agent can be magnesium aluminometasilicate. Non-limiting examples of the taste masking agent is chosen from monosaccharides, disaccharides, sugar alcohols, polydextrose, dextrates, maltodextrin, sugar substitutes, cyclodextrins, flavouring agents, or any combination thereof. In certain embodiments, the taste masking agent can be a combination of β-cyclodextrin, sucralose, and citron flavouring.
[0402] In certain embodiments, the formulations can comprise, by weight based on the total weight of the formulation, (a) 8.3% of the extract of O. stamineus leaves, 75% effervescent couple, 1.5% anti-caking agent, and 15.2% taste masking agent. In certain embodiments, the effervescent couple comprises 33% sodium bicarbonate and 42% citric acid, the anti-caking agent can be magnesium aluminometasilicate, and the taste-masking agent comprises 8.6%, β-cyclodextrin, 5% citron flavouring and 1.6% sucralose.
[0403] In certain other embodiments, the formulations can comprise, by weight based on the weight of the total formulation, (a) 16.5% of the extract of O. stamineus leaves, (b), 35.5% effervescent couple, (c) 1% anti-caking agent, and (d) 47% taste-masking agent. In certain embodiments, the effervescent couple comprises 8.3% sodium bicarbonate and 27.2% citric acid, the anti-caking agent can be magnesium aluminometasilicate, and the taste masking agent comprises, 41% β-cyclodextrin, 5% citron flavouring and 1% sucralose.
[0404] In one embodiment, the method of manufacturing an effervescent formulation comprising the extract of O. stamineus leaves is illustrated in Example 30.
[0405] In certain embodiments, the formulations can comprise from 100 mg - 2000 mg the extract of the O. stamineus leaves (e.g., 100, 125, 150, 175, 200, 225, 250, 275, 300, 325, 350, 375, 400, 425, 450, 475, 500, 525, 550, 575, 600, 625, 650, 675, 700, 725, 750, 775, 800, 825, 850, 875, 900, 925, 950, 975, 1000, 1025, 1050, 1075, 110, 1125, 1150, 1175, 1200, 1225, 1250, 1275, 1300, 1325, 1350, 1375, 1400, 1425, 1450, 1475, 1500, 1525, 1550, 1575, 1600, 1625, 1650, 1675, 1700, 1725, 1750, 1775, 1800, 1825, 1850, 1875, 1900, 1925, 1950, 1975, or 2000 mg). In certain embodiments, the formulations comprise 250 mg - 1000 mg (e.g., 250, 260, 270, 280, 290, 300, 310, 320, 330, 340, 350, 360, 370, 380, 390, 400, 410, 420, 430, 440, 450, 460, 470, 480, 490, 500, 510, 520, 530, 540, 550, 560, 670, 580, 590, 600, 610, 620, 630, 640, 650, 660, 670, 680, 690, 700, 710, 720, 730, 740, 750, 760, 770, 780, 790, 800, 810, 820, 830, 840, 850, 860, 870, 880, 890, 900, 910, 920, 930, 940, 950, 960, 970, 980, 990, or 1000 mg) of the extract of O. stamineus leaves. In certain embodiments, the formulations comprise 250 mg of the extract of the O. stamineus leaves. In certain other embodiments, the formulations comprise 1000 mg of the extract of the O. stamineus leaves.
[0406] In one embodiment, the pharmacokinetics of an effervescent tablet and powder comprising the extract of O. stamineus leaves is described in Example 32.
[0407] In one embodiment, the extract of O. stamineus leaves can be formulated for topical applications comprising a variety of suitable vehicles for delivery of the extract of O. stamineus leaves. The topical applications can be pharmaceutical or cosmeceutical in nature. Non-limiting examples of suitable vehicles for delivery of the extract include emulsions (e.g.,
oil-in-water, water-in-oil, silicon-in-water, water-in-silicon, water-in-oil-in-water, oil-in- water, oil-in-water-in-oil, oil-in-water-in-silicon, etc.), creams, lotions, solutions (both aqueous and hydroalcoholic), anhydrous bases (such as lipsticks and powders), gels, ointments, pastes, milks, liquids, aerosols, sprays, solid forms, or eye jellies. Variations and other appropriate vehicles will be apparent to the skilled person and are appropriate for use with the extract of O. stamineus leaves described herein. In certain aspects, the
concentrations and combinations of the ingredients can be selected in such a way that the combinations are chemically compatible and do not form complexes which precipitate from the finished product.
[0408] In the context of the topical formulations comprising a therapeutically effective amount of the extract of O. stamineus leaves, the Cosmetic and Toiletry Fragrance
Association's (CTFA) International Cosmetic Ingredient Dictionary and Handbook (2008), 12th Edition, describes a wide variety of non-limiting cosmetic ingredients that can be used in the context of the topical formulations described herein. Examples of these ingredient classes include: fragrances (artificial and natural), dyes and color ingredients, adsorbents, emulsifiers, stabilizers, lubricants, solvents, moisturizers (including, e.g., emollients, humectants, film formers, occlusive agents, and agents that affect the natural moisturization mechanisms of the skin), water-repellants, UV absorbers (physical and chemical absorbers such as paraminobenzoic acid ("PABA") and corresponding PABA derivatives, titanium dioxide, zinc oxide, etc.), essential oils, vitamins (e.g., A, B, C, D, E, and K), trace metals (e.g., zinc, calcium and selenium), anti-irritants (e.g., steroids and nonsteroidal antiinflammatories), botanical extracts (e.g., aloe vera, chamomile, cucumber extract, ginkgo biloba, ginseng, and rosemary), anti-microbial agents, antioxidants (e.g., BHT and tocopherol), chelating agents (e.g., disodium EDTA and tetrasodium EDTA), preservatives (e.g., methylparaben and propylparaben), pH adjusters (e.g., sodium hydroxide and citric acid), absorbents (e.g., aluminum starch octenylsuccinate, kaolin, corn starch, oat starch, cyclodextrin, talc, and zeolite), skin bleaching and lightening agents (e.g., hydroquinone and niacinamide lactate), humectants (e.g., glycerin, propylene glycol, butylene glycol, pentylene glycol, sorbitol, urea, and manitol), exfoliants (e.g., alpha-hydroxyacids, and beta- hydroxyacids such as lactic acid, glycolic acid, and salicylic acid; and salts thereof) waterproofing agents (e.g., magnesium/aluminum hydroxide stearate), skin conditioning agents (e.g., aloe extracts, allantoin, bisabolol, ceramides, dimethicone, hyaluronic acid, and dipotassium glycyrrhizate), thickening agents (e.g., substances which that can increase the viscosity of a formulation such as carboxylic acid polymers, crosslinked polyacrylate polymers, polyacrylamide polymers, polysaccharides, and gums), and silicon containing compounds (e.g., silicon oils and polyorganosiloxanes).
[0409] In the context of the topical formulations described herein, certain
embodiments comprising a therapeutically effective amount of the extract of O. stamineus leaves can additionally comprise sunscreen agents, which include chemical and physical sunblocks. UV absorption agents that can be used in combination with the topical formulations include chemical and physical sunblocks. Non-limiting examples of chemical sunblocks that can be used include para-aminobenzoic acid (PABA), PABA esters (glyceryl PABA, amyldimethyl PABA and octyldimethyl PABA), butyl PABA, ethyl PABA, ethyl dihydroxypropyl PABA, benzophenones (oxybenzone, sulisobenzone, benzophenone, and benzophenone-1 through 12), cinnamates (octyl methoxycinnamate, isoamyl p-
methoxycinnamate, octylmethoxy cinnamate, cinoxate, diisopropyl methyl cinnamate, DEA- methoxycinnamate, ethyl diisopropylcinnamate, glyceryl octanoate dimethoxycinnamate and ethyl methoxycinnamate), cinnamate esters, salicylates (homomethyl salicylate, benzyl salicylate, glycol salicylate, isopropylbenzyl salicylate, etc.), anthranilates, ethyl urocanate, homosalate, octisalate, dibenzoylmethane derivatives (e.g., avobenzone), octocrylene, octyl triazone, digalloy trioleate, glyceryl aminobenzoate, lawsone with dihydroxyacetone, ethylhexyl triazone, dioctyl butamido triazone, benzylidene malonate polysiloxane, terephthalylidene dicamphor sulfonic acid, disodium phenyl dibenzimidazole tetrasulfonate, diethylamino hydroxybenzoyl hexyl benzoate, bis diethylamino hydroxybenzoyl benzoate, bis benzoxazoylphenyl ethylhexylimino triazine, drometrizole trisiloxane, methylene bis- benzotriazolyl tetramethylbutylphenol, and bis-ethylhexyloxyphenol methoxyphenyltriazine, 4-methylbenzylidenecamphor, and isopentyl 4-methoxycinnamate. Non-limiting examples of physical sunblocks include, kaolin, talc, petrolatum and metal oxides (e.g., titanium dioxide and zinc oxide). Compositions of the present invention can have UVA and UVB absorption properties. The compositions can have a sun protection factor (SPF) of 2, 3, 4, 56, 7, 8, 9, 10, 11, 12, 13, 14, 15, 20, 25, 30, 35, 40, 45, 50, 55, 60, 70, 80, 90 or more, or any integer therein.
[0410] In certain embodiments, topical formulations comprising a therapeutically effective amount of the extract of O. stamineus leaves can comprise one or more moisturizing agents. Non-limiting examples of moisturizing agents that can be used with the topical formulations described herein include amino acids, chondroitin sulfate, diglycerin, erythritol, fructose, glucose, glycerin, glycerol polymers, glycol, 1,2,6-hexanetriol, honey, hyaluronic acid, hydrogenated honey, hydrogenated starch hydrolysate, inositol, lactitol, maltitol, maltose, mannitol, natural moisturizing factor, PEG-15 butanediol, polyglyceryl sorbitol, salts of pyrollidone carboxylic acid, potassium PCA, propylene glycol, sodium glucuronate, sodium PCA, sorbitol, sucrose, trehalose, urea, xylitol, acetylated lanolin, acetylated lanolin alcohol, acrylates/ClO-30 alkyl acrylate crosspolymer, acrylates copolymer, alanine, algae extract, aloe barbadensis, aloe-barbadensis extract, aloe barbadensis gel, althea officinalis extract, aluminum starch octenylsuccinate, aluminum stearate, apricot (prunus armeniaca) kernel oil, arginine, arginine aspartate, arnica montana extract, ascorbic acid, ascorbyl palmitate, aspartic acid, avocado (persea gratissima) oil, barium sulfate, barrier sphingolipids, butyl alcohol, beeswax, behenyl alcohol, beta- sitosterol, BHT, birch (betula alba) bark extract, borage (borago officinalis) extract, 2-bromo- 2-nitropropane-l,3-diol, butcher's broom (ruscus aculeatus) extract, butylene glycol, calendula officinalis extract, calendula officinalis oil, candelilla (euphorbia cerifera) wax, canola oil, caprylic/capric triglyceride, cardamon (elettaria cardamomum) oil, carnauba (copernicia cerifera) wax, carrageenan (chondrus crispus), carrot (daucus carota sativa) oil, castor (ricinus communis) oil, ceramides, ceresin, ceteareth-5, ceteareth-12, ceteareth-20, cetearyl octanoate, ceteth-20, ceteth-24, cetyl acetate, cetyl octanoate, cetyl palmitate, chamomile (anthemis nobilis) oil, cholesterol, cholesterol esters, cholesteryl
hydroxystearate, citric acid, clary (salvia sclarea) oil, cocoa (theobroma cacao) butter, coco- caprylate/caprate, coconut (cocos nucifera) oil, collagen, collagen amino acids, corn (zea mays) oil, fatty acids, decyl oleate, dextrin, diazolidinyl urea, dimethicone copolyol, dimethiconol, dioctyl adipate, dioctyl succinate, dipentaerythrityl
hexacaprylate/hexacaprate, DMDM hydantoin, DNA, erythritol, ethoxydiglycol, ethyl
linoleate, eucalyptus globulus oil, evening primrose (Oenothera biennis) oil, fatty acids, fructose, gelatin, geranium maculatum oil, glucosamine, glucose glutamate, glutamic acid, glycereth-26, glycerin, glycerol, glyceryl distearate, glyceryl hydroxystearate, glyceryl laurate, glyceryl linoleate, glyceryl myristate, glyceryl oleate, glyceryl stearate, glyceryl stearate SE, glycine, glycol stearate, glycol stearate SE, glycosaminoglycans, grape (vitis vinifera) seed oil, hazel (corylus americana) nut oil, hazel (corylus avellana) nut oil, hexylene glycol, honey, hyaluronic acid, hybrid safflower (carthamus tinctorius) oil, hydrogenated castor oil, hydrogenated coco-glycerides, hydrogenated coconut oil, hydrogenated lanolin, hydrogenated lecithin, hydrogenated palm glyceride, hydrogenated palm kernel oil, hydrogenated soybean oil, hydrogenated tallow glyceride, hydrogenated vegetable oil, hydrolyzed collagen, hydrolyzed elastin, hydrolyzed glycosaminoglycans, hydrolyzed keratin, hydrolyzed soy protein, hydroxylated lanolin, hydroxyproline, imidazolidinyl urea, iodopropynyl butylcarbamate, isocetyl stearate, isocetyl stearoyl stearate, isodecyl oleate, isopropyl isostearate, isopropyl lanolate, isopropyl myristate, isopropyl palmitate, isopropyl stearate, isostearamide DEA, isostearic acid, isostearyl lactate, isostearyl neopentanoate, jasmine (jasminum officinale) oil, jojoba (buxus chinensis) oil, kelp, kukui (aleurites moluccana) nut oil, lactamide M EA, laneth-16, laneth-10 acetate, lanolin, lanolin acid, lanolin alcohol, lanolin oil, lanolin wax, lavender (lavandula angustifolia) oil, lecithin, lemon (citrus medica limonum) oil, linoleic acid, linolenic acid, macadamia ternifolia nut oil, magnesium stearate, magnesium sulfate, maltitol, matricaria (chamomilla recutita) oil, methyl glucose sesquistearate, methylsilanol PCA, microcrystalline wax, mineral oil, mink oil, mortierella oil, myristyl lactate, myristyl myristate, myristyl propionate, neopentyl glycol dicaprylate/dicaprate, octyldodecanol, octyldodecyl myristate, octyldodecyl stearoyl stearate, octyl hydroxystearate, octyl palmitate, octyl salicylate, octyl stearate, oleic acid, olive (olea europaea) oil, orange (citrus aurantium dulcis) oil, palm (elaeis guineensis) oil, palmitic acid, pantethine, panthenol, panthenyl ethyl ether, paraffin, PCA, peach (prunus persica) kernel oil, peanut (arachis hypogaea) oil, PEG-8 C12-18 ester, PEG-15 cocamine, PEG-150 distearate, PEG-60 glyceryl isostearate, PEG-5 glyceryl stearate, PEG-30 glyceryl stearate, PEG-7 hydrogenated castor oil, PEG-40 hydrogenated castor oil, PEG-60 hydrogenated castor oil, PEG-20 methyl glucose sesquistearate, PEG40 sorbitan peroleate, PEG-5 soy sterol, PEG-10 soy sterol, PEG-2 stearate, PEG-8 stearate, PEG-20 stearate, PEG-32 stearate, PEG40 stearate, PEG-50 stearate, PEG-100 stearate, PEG-150 stearate,
pentadecalactone, peppermint (mentha piperita) oil, petrolatum, phospholipids, polyamino sugar condensate, polyglyceryl-3 diisostearate, polyquatemrnium-24, polysorbate 20, polysorbate 40, polysorbate 60, polysorbate 80, polysorbate 85, potassium myristate, potassium palmitate, potassium sorbate, potassium stearate, propylene glycol, propylene glycol dicaprylate/dicaprate, propylene glycol dioctanoate, propylene glycol dipelargonate, propylene glycol laurate, propylene glycol stearate, propylene glycol stearate SE, PVP, pyridoxine dipalmitate, quaternium-15, quaternium-18 hectorite, quaternium-22, retinol, retinyl palmitate, rice (oryza sativa) bran oil, NA, rosemary (rosmarinus officinalis) oil, rose oil, safflower (carthamus tinctorius) oil, sage (salvia officinalis) oil, salicylic acid, sandalwood (santalum album) oil, serine, serum protein, sesame (sesamum indicum) oil, shea butter (butyrospermum parkii), silk powder, sodium chondroitin sulfate, sodium hyaluronate, sodium lactate, sodium palmitate, sodium PCA, sodium polyglutamate, sodium stearate, soluble collagen, sorbic acid, sorbitan laurate, sorbitan oleate, sorbitan palmitate, sorbitan
sesquioleate, sorbitan stearate, sorbitol, soybean (glycine soja) oil, sphingolipids, squalane, squalene, stearamide MEA-stearate, stearic acid, stearoxy dimethicone,
stearoxytrimethylsilane, stearyl alcohol, stearyl glycyrrhetinate, stearyl heptanoate, stearyl stearate, sunflower (helianthus annuus) seed oil, sweet almond (prunus amygdalus dulcis) oil, synthetic beeswax, tocopherol, tocopheryl acetate, tocopheryl linoleate, tribehenin, tridecyl neopentanoate, tridecyl stearate, triethanolamine, tristearin, urea, vegetable oil, water, waxes, wheat (triticum vulgare) germ oil, and ylang ylang (cananga odorata) oil. Combinations of the above moisturizing agents are permissible.
[0411] In certain embodiments, the topical compositions comprising a therapeutically effective amount of the extract of O. stamineus leaves can comprise one or more antioxidants. Non-limiting examples of antioxidants that can be used with the topical formulations described herein include acetyl cysteine, ascorbic acid polypeptide, ascorbyl dipalmitate, ascorbyl methylsilanol pectinate, ascorbyl palmitate, ascorbyl stearate, BHA, BHT, t-butyl hydroquinone, cysteine, cysteine HCI, diamylhydroquinone, di-t- butylhydroquinone, dicetyl thiodipropionate, dioleyl tocopheryl methylsilanol, disodium ascorbyl sulfate, distearyl thiodipropionate, ditridecyl thiodipropionate, dodecyl gallate, erythorbic acid, esters of ascorbic acid, ethyl ferulate, ferulic acid, gallic acid esters, hydroquinone, isooctyl thioglycolate, kojic acid, magnesium ascorbate, magnesium ascorbyl phosphate, methylsilanol ascorbate, natural botanical antioxidants such as green tea or grape seed extracts, nordihydroguaiaretic acid, octyl gallate, phenylthioglycolic acid, potassium ascorbyl tocopheryl phosphate, potassium sulfite, propyl gallate, quinones, rosmarinic acid, sodium ascorbate, sodium bisulfite, sodium erythorbate, sodium metabisulfite, sodium sulfite, superoxide dismutase, sodium thioglycolate, sorbitol furfural, thiodiglycol, thiodiglycolamide, thiodiglycolic acid, thioglycolic acid, thiolactic acid, thiosalicylic acid, tocophereth-5, tocophereth-10, tocophereth-12, tocophereth-18, tocophereth-50, tocopherol, tocophersolan, tocopheryl acetate, tocopheryl linoleate, tocopheryl nicotinate, tocopheryl succinate, and tris(nonylphenyl)phosphite.
[0412] In certain embodiments, the topical formulations comprising a therapeutically effective amount of the extract of O. stamineus leaves can comprise one or more structuring agents. Structuring agents assist in providing rheological characteristics to the topical formulations to contribute to the formulation's stability. In other aspects, structuring agents can also function as an emulsifier or surfactant. Non-limiting examples of structuring agents include stearic acid, palmitic acid, stearyl alcohol, cetyl alcohol, behenyl alcohol, stearic acid, palmitic acid, the polyethylene glycol ether of stearyl alcohol having an average of about 1 to about 21 ethylene oxide units, the polyethylene glycol ether of cetyl alcohol having an average of about 1 to about 5 ethylene oxide units, and mixtures thereof.
[0413] In certain embodiments, the topical formulations comprising a therapeutically effective amount of the extract of O. stamineus leaves can comprise one or more emulsifiers. Emulsifiers can reduce the interfacial tension between phases and improve the formulation and stability of an emulsion. The emulsifiers can be nonionic, cationic, anionic, and zwitterionic emulsifiers (See U.S. Pat. Nos. 5,011,681; 4,421,769; 3,755,560). Non- limiting examples of emulsifiers for use in topical formulations include esters of glycerin, esters of propylene glycol, fatty acid esters of polyethylene glycol, fatty acid esters of polypropylene glycol, esters of sorbitol, esters of sorbitan anhydrides, carboxylic acid copolymers, esters and ethers of glucose, ethoxylated ethers, ethoxylated alcohols, alkyl
phosphates, polyoxyethylene fatty ether phosphates, fatty acid amides, acyl lactylates, soaps, TEA stearate, DEA oleth-3 phosphate, polyethylene glycol 20 sorbitan monolaurate (polysorbate 20), polyethylene glycol 5 soya sterol, steareth-2, steareth-20, steareth-21, ceteareth-20, PPG-2 methyl glucose ether distearate, ceteth-10, polysorbate 80, cetyl phosphate, potassium cetyl phosphate, diethanolamine cetyl phosphate, polysorbate 60, glyceryl stearate, PEG-100 stearate, and mixtures thereof.
[0414] In certain embodiments, the topical formulations comprising a therapeutically effective amount of the extract of O. stamineus leaves can comprise one or more silicon containing compounds. Non-limiting examples of silicon containing compounds include any member of a family of polymeric products whose molecular backbone is made up of alternating silicon and oxygen atoms with side groups attached to the silicon atoms. By varying the— Si— O— chain lengths, side groups, and crosslinking, silicons can be synthesized into a wide variety of materials. They can vary in consistency from liquid to gel to solids. The silicon containing compounds that can be used in the context of the topical formulations described herein are those known to a person of ordinary skill. Non-limiting examples include silicon oils (e.g., volatile and non-volatile oils), gels, and solids. In one embodiment, the silicon containing compound includes a silicon oil such as a
polyorganosiloxane. Non-limiting examples of polyorganosiloxanes include dimethicone, cyclomethicone, polysilicon-11, phenyl trimethicone, trimethylsilylamodimethicone, stearoxytrimethylsilane, or mixtures of these and other organosiloxane materials in any given ratio to achieve the desired consistency and application characteristics depending upon the intended application (e.g., to a particular area such as the skin, hair, or eyes). A "volatile silicon oil" includes a silicon oil having a low heat of vaporization, i.e. normally less than about 50 cal per gram of silicon oil. Non-limiting examples of volatile silicon oils include: cyclomethicones such as Dow Corning 344 Fluid, Dow Corning 345 Fluid, Dow
Corning 244 Fluid, and Dow Corning 245 Fluid, Volatile Silicone 7207 (Union Carbide Corp., Danbury, Conn.); low viscosity dimethicones, i.e. dimethicones having a viscosity of about 50 est or less (e.g., dimethicones such as Dow Corning 200-0.5 est Fluid). The Dow Corning Fluids are available from Dow Corning Corporation, Midland, Mich. Cyclomethicone and dimethicone are described in the Third Edition of the CTFA Cosmetic Ingredient Dictionary (incorporated by reference) as cyclic dimethyl polysiloxane compounds and a mixture of fully methylated linear siloxane polymers end-blocked with trimethylsiloxy units, respectively. Other non-limiting volatile silicon oils that can be used in the context of the present invention include those available from General Electric Co., Silicon Products Div., Waterford, N.Y. and SWS Silicons Div. of Stauffer Chemical Co., Adrian, Mich.
[0415] In certain embodiments, the topical formulations comprising a therapeutically effective amount of the extract of O. stamineus leaves can comprise one or more essential oils. Non-limiting examples of essential oils include oils derived from herbs, flowers, trees, and other plants. Non-limiting examples of essential oils that can be used in the topical formulations described herein include sesame oil, macadamia nut oil, tea tree oil, evening primrose oil, Spanish sage oil, Spanish rosemary oil, coriander oil, thyme oil, pimento berries oil, rose oil, anise oil, balsam oil, bergamot oil, rosewood oil, cedar oil, chamomile oil, sage oil, clary sage oil, clove oil, cypress oil, eucalyptus oil, fennel oil, sea fennel oil, frankincense oil, geranium oil, ginger oil, grapefruit oil, jasmine oil, juniper oil, lavender oil, lemon oil, lemongrass oil, lime oil, mandarin oil, marjoram oil, myrrh oil, neroli oil, orange oil, patchouli
oil, pepper oil, black pepper oil, petitgrain oil, pine oil, rose otto oil, rosemary oil, sandalwood oil, spearmint oil, spikenard oil, vetiver oil, wintergreen oil, or ylang ylang. Other essential oils known to the skilled person are also contemplated as being useful within the context of the topical formulations described herein.
[0416] In certain embodiments, the topical formulations comprising a therapeutically effective amount of the extract of O. stamineus leaves can comprise one or more thickening agents. Thickening agents, including thickener or gelling agents, include substances that can increase the viscosity of a topical formulation. Thickeners include those that can increase the viscosity of a topical formulation without substantially modifying the efficacy of the active ingredient within the formulation. Thickeners can also increase the stability of the topical formulations described herein. Non-limiting examples of thickening agents that can be used in the topical formulations described herein include carboxylic acid polymers, crosslinked polyacrylate polymers, polyacrylamide polymers, polysaccharides, and gums. Examples of carboxylic acid polymers include crosslinked compounds containing one or more monomers derived from acrylic acid, substituted acrylic acids, and salts and esters of these acrylic acids and the substituted acrylic acids, wherein the crosslinking agent contains two or more carbon-carbon double bonds and is derived from a polyhydric alcohol (see U.S. Pat. Nos. 5,087,445; 4,509,949; 2,798,053; CTFA International Cosmetic Ingredient Dictionary, Fourth edition, 1991, pp. 12 and 80). Examples of commercially available carboxylic acid polymers include carbomers, which are homopolymers of acrylic acid crosslinked with allyl ethers of sucrose or pentaerythritol (e.g., Carbopol™ 900 series from B. F. Goodrich). Non-limiting examples of crosslinked polyacrylate polymers include cationic and nonionic polymers. Examples are described in U.S. Pat. Nos. 5,100,660; 4,849,484; 4,835,206; 4,628,078;
4,599,379. Non-limiting examples of polyacrylamide polymers (including nonionic polyacrylamide polymers including substituted branched or unbranched polymers) include polyacrylamide, isoparaffin and laureth-7, multi-block copolymers of acrylamides and substituted acrylamides with acrylic acids and substituted acrylic acids. Non-limiting examples of polysaccharides include cellulose, carboxymethyl hydroxyethylcellulose, cellulose acetate propionate carboxylate, hydroxyethylcellulose, hydroxyethyl ethylcellulose, hydroxypropylcellulose, hydroxypropyl methylcellulose, methyl hydroxyethylcellulose, microcrystalline cellulose, sodium cellulose sulfate, and mixtures thereof. Another example is an alkyl substituted cellulose where the hydroxy groups of the cellulose polymer is hydroxyalkylated (preferably hydroxy ethylated or hydroxypropylated) to form a
hydroxyalkylated cellulose which is then further modified with a C10-C30 straight chain or branched chain alkyl group through an ether linkage. Typically, these polymers are ethers of C10-C30 straight or branched chain alcohols with hydroxyalkylcelluloses. Other useful polysaccharides include scleroglucans comprising a linear chain of (1-3) linked glucose units with a (1-6) linked glucose every three unit. Non-limiting examples of gums that can be used include acacia, agar, algin, alginic acid, ammonium alginate, amylopectin, calcium alginate, calcium carrageenan, carnitine, carrageenan, dextrin, gelatin, gellan gum, guar gum, guar hydroxypropyltrimonium chloride, hectorite, hyaluronic acid, hydrated silica, hydroxypropyl chitosan, hydroxypropyl guar, karaya gum, kelp, locust bean gum, natto gum, potassium alginate, potassium carrageenan, propylene glycol alginate, sclerotium gum, sodium carboxymethyl dextran, sodium carrageenan, tragacanth gum, xanthan gum, and mixtures thereof.
[0417] In certain embodiments, the topical formulations comprising a therapeutically effective amount of the extract of O. stamineus leaves can comprise honey. Honey is a natural product that has been used widely for its therapeutic effects for centuries. While the chemical composition of honey is dependent on the plant on which the bee feeds, honey is rich in therapeutic compounds, and all natural honey contains flavonoids (e.g., apigenin, pinocembrin, kaempferol, quercetin, galangin, chrysin and hesperetin), phenolic acids (e.g., ellagic, caffeic, p-coumaric and ferulic acids), ascorbic acid, tocopherols, catalase (CAT), superoxide dismutase (SOD), reduced glutathione (GSH), Millard reaction products and peptides, which work together synergistically to provide a therapeutic effect (147). Honey has been shown to expedite wound healing, and have anti-microbial, anti-inflammatory, antioxidant, anti-mutagenic, anti-tumor, and antidiabetic activity (148). Honey is normally named after the geographical location where the honey is produced, the floral source of the honey or the tree or plant on which the hive is found. While any type of honey can be used in the formulating the topicals described herein, honey with a high number and amount of therapeutic ingredients is preferred. The honey can be multifloral or unifloral. Non-limiting examples of the type of honey that can be used in the topical formulations described herein include, Manuka honey, pasture honey, jelly bush honey, African jungle honey, and Tualang honey. Combinations of honey can be used in the topical formulations described herein. In certain embodiments, the topical formulations described herein can comprise from 1% - 5% (e.g., 1, 1.2, 1.4, 1.6, 1.8, 2, 2.2, 2.4, 2.6, 2.8, 3, 3.2, 3.4, 3.6, 3.8, 4, 4.2, 4.6, 4.8, or 5%) by weight based on the total weight of the formulation. In certain embodiments, Tualang honey, a Malaysian multifloral honey produced by the rock bee (Apis dorsata), which builds hives high up in the branches of Tualang tree (Koompassia excelsa) is preferred. Tualang honey has been shown to have higher phenolics, flavonoids, and 5-(hydroxymethyl) furfural (HM F) and is also more effective as an antibiotic in the treatment of burn wounds compared to Manuka honey (148), likely by increasing the number of fibroblasts and decreasing the number of inflammatory cells at the wound site (149).
[0418] Certain embodiments provide for formulations comprising the extract of O. stamineus leaves that can be incorporated into a variety of nanoparticle based formulations. Examples of various nanoparticles that can be used for formulations comprising the extract of O. stamineus leaves, include, but are not limited to, nano liposomal formulations, dendrimers, Poly (Lactic-co-glycolic-acid) (PLGA), niosomes, emulsions, and microspheres. Non-limiting examples of nano liposomal formulations include, nano liposomes, phytosomes, and ethosomes. Emulsions refer to microemulsions (nanoemulsions) and sub- microemulsions (lipid emulsions). Other examples of nanoparticles include nanospheres, nanocapsules, solid lipid nanoparticles, and nanostructured lipid carriers. The various nanoparticles, their use in the delivery of plant extracts, and methods of manufacturing them have been described and reviewed in the prior art (150) (151) (152) (153). In certain embodiments, the nanoparticles comprise the extract of O. stamineus leaves in combination with at least one other therapeutic agent. In certain embodiments, the other therapeutic agent is a monotherapeutic agent, a plant extract, an animal extract, or any combination thereof.
[0419] In certain embodiments, the nanoparticles comprising at least the extract of O. stamineus leaves can be incorporated into topical formulations. In certain embodiments, the nanoparticles incorporated into a topical formulation can be nano liposomes, ethosomes, or
phytosomes or combinations thereof.
[0420] In certain embodiments, the formulations comprise nano liposomal formulations. Liposomes are spherical micro-vesicles surrounded by one or more bilayer phospholipid membranes enclosing an internal aqueous core comprising a pharmaceutical cargo. There are various types of phospholipids that can be used in preparation of liposomes, including phosphatidylcholine, phosphotidylserine, phosphotidylethanolamine, and phosphatidylinositol. Various methods for preparation of nano liposomes are well known in the art. Nano liposomes are one of the nanoparticles that can be used as drug delivery systems to improve selectivity of targeting of drugs to a specific target, especially for anti-cancer treatments, which leads to high efficiency and safety of drugs with sustainable drug release. The size of nano liposomes most suitable for drug delivery can be from 100 to 200 nm in diameter. Nano liposome formulations comprising a macerated extract of O. stamineus leaves have been described in (154) (155). One embodiment of a nano liposome comprising an extract of O. stamineus leaves is described in Example 15.
[0421] In certain embodiments, the nanoparticles comprise ethosomes. Ethosomes are nano-vesicles comprising, phospholipid, EtOH, a therapeutic agent, and water. Ethosomes are modified nano liposomes, which entrap an aqueous EtOH solution of the desired therapeutic agent, and are well suited for the delivery of a wide variety of therapeutic agents particularly via the skin. Ethosomes are "soft" nano-vesicles formed from
phospholipids in the presence of water and EtOH (alcohol) or glycols (polyols). The size of the vesicles depends on the ratio of the water to alcohol and on the phospholipid concentration. In topical formulations prior to application on skin, ethosomes do not change their size since the ratio of the solvents remains constant. However, when applied onto skin, evaporation of the solvents results in a change in the ratio of the solvents, which leads to a fusion of the ethosomes until a film is formed on the skin surface. Permeation enhancers increase the permeability of the skin, allowing therapeutic agents to cross the skin effectively. EtOH is an effective permeation enhancer and ethosomes have a high EtOH content ranging from 20% - 50% (wt/wt) of the ethosome. Thus, ethosomes, due to their high EtOH content, are useful for the delivery of a wide variety of therapeutic agents, including the delivery of therapeutic agents that are diverse in their composition (e.g., plant and/or animal extracts) through skin. Example of other penetration enhancers include N- Decylmethyl sulfoxide, dimethyl sulfoxide, Tween 80, Tween, 60, Tween, 20, Oleic acid, 1- menthol, sodium stearate, sodium cholate, deoxycholic acid, sodium deoxycholate, sodium taurocholate, polyethylene glycol 4000, Hexadecyltrimethylammonium bromide, Cremophor EL-35, Cremophor h-40, Spans 80, Spans 60, Spans 40, Spans 20, Skin-penetrating and cell- entering (SPACE) peptide, and sodium dodecyl sulfate. A variety of phospholipids can be used in the formation of ethosomes. Non-limiting examples of phospholipids that can be used in the formation of ethosomes include phosphatidylserine; phosphatidylcholine (e.g., granules comprising 90% phosphatidylcholine from soybean; powder comprising 90% hydrogenated phosphatidylcholine from soybean; powder comprising hydrogenated phospholipids from soybean comprising 70% phosphatidylcholine; a mixture comprising 70% - 80% phosphatidylcholine, a dry residue comprising up to 6% lysophosphatidylcholine, up to 4% cephalin, and up to 6% phosphatidic acid, up to 6% natural oils and sterol, and 20 % to 30% EtOH; a powder comprising 99% l,2-Dipalmitoyl-roc-glycero-3-phosphocholine;
phosphatidylcholine from soybean in the form of agglomerates; phosphatidylcholine content
(50%-75%) from soybean; agglomerates from egg yolk comprising 82% phosphatidylcholine; soybean/egg yolk lyophilized powder comprising 99% 1,2-Diacyl-sn- glycero-3-phosphocholine; synthetic powder comprising 99% l-Hexadecanoyl-2-(9Z- octadecenoyl)-sn-glycero-3-phosphocholine; phosphatidic acid; phosphatidylethanolamine (e.g, bovine/sheep brain f lyophilized powder comprising 98% 3-sn-
Phosphatidylethanolamine; A/-(Succinimidyloxy-glutaryl)-l-a-phosphatidylethanolamine, 1- palmitoyl-2-oleoyl); phosphatidylglycol; l,2-Dipalmitoyl-sn-glycero-3-phospho-(l'-roc- glycerol) sodium salt in the form of a powder; l,2-Dioleoyl-3-trimethylammonium-propane (chloride salt) in the form of a powder or EtOH solution; lecithin from soy purified phosphatidylcholine, concentration 45%, rich in linoleic acid (65%) and palmitic acid (~20%) in the form of a solid wax; and hydrogenated phosphatidylcholine. The concentration of the phospholipids can range between 0.5% - 10% wt/wt (e.g., 0.5, 0.6, 0.7, 0.8, 0.9, 1, 1.5, 2, 2.5, 3, 3.5, 4, 4.5, 5, 5.5, 6, 6.5, 7, 7.5, 8, 8.5, 9, 9.5 or 10%) of the ethosome. The source of the phospholipids can be egg, soybean, semi-synthetics, and synthetics. Cholesterol ranging from 0.1% - 1% wt/wt (e.g., 0.1, 0.2, 0.3, 0.4, 0.5, 0.6, 0.7, 0.8, 0.9 or 1%) of the ethosome can also be incorporated into the ethosomes. Examples of alcohols that can be used include EtOH and isopropyl alcohol. Examples of glycols include propylene glycol and 2-(2- ethoxyethoxy)ethanol. 2-(2-ethoxyethoxy)ethanol is sold under the trade name Transcutol ® and its variations Transcutol® P, Transcutol® V, Transcutol® HP, and Transcutol® CG by Gattefosse (Saint-Priest, France). The concentration of alcohol in the final product can range from 20% - 50% (e.g., 20, 22, 24, 26, 28, 30, 32, 34, 36, 38, 40, 42, 44, 46, 48, or 50%). The concentration of the non-aqueous phase (i.e., the alcohol and glycol combination) can range from 22% - 70% (e.g., 22, 24, 26, 28, 30, 32, 34, 36, 38, 40, 42, 44, 46, 48, 50, 52, 54, 56, 58, 60, 62, 64, 66, 68 or 70%). Nonionic surfactants can be combined with the phospholipids in the formation of ethosomes. Non-limiting examples of such non-ionic surfactants include polyethylene glycol-alkyl ethers. Cationic lipids e.g., coco amides, POE alkyl amines, dodecylamine, and cetrimide. Examples of ethosomes are described in US Pat. No.
5,540,934; (151) (156) (157) (158) (159) (160). There are at least four (4) methods of manufacturing ethosomes, commonly referred to in the prior art as the Hot Method, Cold Method, Classic Mechanical Dispersion Method, and the Classic Method. These methods of manufacturing ethosomes have been described, for example, in (156) (157) (159) (160), and US. Pat. No. 5,540,934. In one embodiment, ethosomes comprise the extract of O.
stamineus leaves, a phospholipid (e.g., phosphatidylcholine) and cholesterol. The ratio of cholesterol to phospholipid can be 1:12 (wt/wt), the ratio of the cholesterol to the extract of O. stamineus leaves can be 1:2 (wt/wt), and the ratio of the extract of O. stamineus leaves to the phospholipid can be 1:6 (wt/wt). One embodiment for manufacturing ethosomes comprising the extract of O. stamineus leaves is illustrated in Example 27. Example 27 also demonstrates the use of ethososmes comprising a therapeutically effective amount of the extract of O. stamineus leaves and a sophorolipid for the treatment of melanoma. Another embodiment for manufacturing ethosomes comprising the extract of O. stamineus leaves and use of the ethosomes for the treatment of melanoma is illustrated in Example 28. In certain embodiments, the ethosomes comprising the extract of O. stamineus leaves can be formulated into dosage forms, examples of which include gels, ointments, pastes, milks, liquids, aerosols, sprays, solid forms, or eye jellies.
[0422] In certain embodiments, the phospholipids in the ethosomes can be substituted
with sophorolipids (SLs). SLs are biosurfactant glycolipid compounds that are synthesized by a select number of non-pathogenic Candida species (e.g., Candida gropengiesseri, Candida magnoliae and Candida bombicola). SLs are amphiphilic molecules composed of hydrophilic moiety, a sophorose disaccharide (2'-0- -D-glucopyranosyl- -D-glycopyranose), linked to the hydrophobic moiety, a long chain of fatty acid. SLs are produced as complex mixtures comprising both free acid and lactone forms. SLs are naturally synthesized with a preference for the lactonic form, which are more hydrophobic, and have been reported to have better biocidal activities. The anti-cancer, anti-microbial, immune-modulatory, anti-viral and spermicidal activity of SLs have been reviewed by de Oliveira et al. (161). SLs can also be produced using palm oil as the substrate (162). Palm-based SLs have also shown antimicrobial (162) (163) and anti-angiogenic activity (164). Given these activities of SLs, it is believed, without being held to any one theory, that the combination of the extract of O. stamineus leaves and SLs can provide ethosome formulations with synergistic anti-microbial and anti-cancer activities. Accordingly, in one embodiment, the ethosome formulations comprise the extract of O. stamineus leaves and at least one SL. In one embodiment, the SL can be obtained from microbial cultivation. In one embodiment, the SL can be palm based. In one embodiment, the SL can be in its free acid or lactonic form. In one embodiment, the SL can comprise hydroxyl fatty acid distribution incorporated in non, mono- and diacetylated sophorolipids either in their free acid or lactonic form as disclosed in US6,596,265. In one embodiment, the SL can be a medium chain SL as disclosed in US 8,530,206. In one embodiment, the SL can be open chained as disclosed in US patent publication no.
20060199244. The amount of the SLs in ethosomes comprising the extract of O. stamineus leaves can range between 0.5% - 10% wt/wt (e.g., 0.5, 0.6, 0.7%, 0.8, 0.9, 1, 1.5, 2, 2.5, 3, 3.5, 4, 4.5, 5, 5.5, 6, 6.5, 7, 7.5, 8, 8.5, 9, 9.5 or 10%) of the ethosome. Cholesterol ranging from 0.1% - 1% wt/wt (e.g., 0.1, 0.2, 0.3, 0.4, 0.5, 0.6, 0.7, 0.8, 0.9 or 1%) of the ethosome can also be incorporated into ethosomes comprising SLs and the extract of O. stamineus leaves. Examples of alcohols that can be used include EtOH and isopropyl alcohol. Examples of glycols include propylene glycol and 2-(2-ethoxyethoxy)ethanol. 2-(2- ethoxyethoxy)ethanol is sold under the trade name Transcutol ® and its variations
Transcutol® P, Transcutol® V, Transcutol® HP, and Transcutol® CG by Gattefosse (Saint- Priest, France). The concentration of alcohol in the ethosome comprising the SL and extract of O. stamineus leaves can range from 20% - 50% (e.g., 20, 22, 24, 26, 28, 30, 32, 34, 36, 38, 40, 42, 44, 46, 48, or 50%). The concentration of the non-aqueous phase (i.e., the alcohol and glycol combination) can range from 22% - 70% (e.g., 20, 22, 24, 26, 28, 30, 32, 34, 36, 38, 40, 42, 44, 46, 48, 50, 52, 54, 56, 58, 60, 62, 64, 66, 68 or 70%). In one embodiment, the ratio of the extract of O. stamineus leaves to the SL can be 1:2 (wt/wt). The methods for manufacturing ethosomes comprising the extract of O. stamineus leaves and SLs is the same as that described for the manufacture of ethosomes comprising the extract of O. stamineus leaves and phospholipids. A typical method for the manufacture of ethosomes comprising the extract of O. stamineus leaves and SLs is described in Example 27. Ethosomes comprising a therapeutically effective amount of the extract of O. stamineus leaves and SLs are well suited for the manufacture of topical dosage forms. One embodiment for the use of a topical formulation comprising ethosomes manufactured with a sophorolipid for the treatment of melanoma is demonstrated in Example 27, Table 58A. One embodiment for the use of a topical formulation comprising ethosomes manufactured with a sophorolipid for promoting
wound healing Is demonstrated in Example 27, Table 58B.
[0423] In certain embodiments, the nanoparticles comprise phytosomes. Unlike ethosomes, which are primarily suited for transdermal delivery of therapeutic agents, phytosomes can be used for both transdermal delivery and oral delivery of therapeutic agents. Most phytochemical constituents of plants are chemically polar and hence water soluble. However, phytochemicals are poorly absorbed due to their large molecular size, and hence are poorly absorbed by passive diffusion or are poorly lipid soluble. Unlike ethosomes and nano liposomes, which entrap a solution of a therapeutic agent, phytosomes form molecular complexes with chemical constituents of the plant and/or animal extracts to produce lipid compatible nanostructures, thereby improving their absorption and bioavailability of the phytochemical payload. The phospholipid comprising the phytosome and the chemical constituents comprising the plant and/or animal extract form a molecular complex via hydrogen bonds (165). Non-limiting examples of phospholipids for use in the preparation of phytosomes include soy lecithin, phosphatidylcholine,
phosphatidylethanolamine, phosphatidylserine, in which acyl group can be same or different and mostly derived from palmitic, stearic, oleic and linoleic acid, or any combination thereof. The ratio of the phospholipid to the therapeutic agent (e.g., extract of O. stamineus leaves) can be at least 0.5:1. Ratios greater than 0.5:1 are permissible (e.g., 1:1, 2:1, 3:1, 4:1, 5:1, 6:1, etc.) In one embodiment, the ratio of the phospholipid to the therapeutic agent (e.g., the extract of O. stamineus leaves) is 1:1. Description of phytosomes and methods of manufacturing phytosomes have been reviewed or described in (151) (165) (166) (167),US Pat. No. 5,118,671; 6,297,218; 6,818,233; WO2012063198A1, and WO2011045732A2.
Certain embodiments provide for phytosomes comprising the extract of O. stamineus leaves alone or in combination with other plant extracts, animal extracts, or monotherapeutic agents. One embodiment for manufacturing phytosomes comprising the extract of O.
stamineus leaves is illustrated in Example 27. In one embodiment, the phytosomes comprise the extract of O. stamineus leaves and a phospholipid. In one embodiment, the ratio of the extract of O. stamineus leaves to the phospholipid is 1:1 (wt/wt). In one embodiment, 20% of the phytosome comprises EtOH. In one embodiment, the phytosomes have a diameter in the range of 25 - 100nm.
[0424] In certain embodiments, the phytosomes comprising the extract of O.
stamineus leaves can be formulated into any immediate release or modified release dosage form (e.g., an immediate release dosage form (oral or non-oral), a modified release dosage form (oral or non-oral), a sublingual film, a sublabial film, a buccal film, an ointment, a gel, dendrimers, an oral spray, an orally disintegrating tablet, a lozenge, an effervescent tablet, sublingual drops, a lollipop, a chewing gum, a solid immediate release oral dosage form (e.g. tablets, microspheres, granules, mini tablets, etc.), a modified release oral dosage form (e.g. tablets, microspheres, granules, mini tablets, etc.), a capsule, a gelcap, a pastille, multiparticulates (e.g., microspheres, granules, powder), a mini tablet, a caplet, an effervescent powder, a hydrogel, syrups, a medicated straw, a dry-powder inhaler, a nebulizer, a metered dose inhaler, a suppository, dendrimers, a catheter, a vaginal tablet, a vaginal cream, a vaginal suppository, a vaginal ring, a dermal patch, a transdermal patch, ethosomes, niosomes, discosomes, phytosomes, liposomes, a lotion, a lip balm, an ointment, a cream, an emulsion, a topical spray, a nasal spray, a medicated shampoo, eye drops, an injectable, a topical emulsion, biodegradable microparticles, biodegradable
microspheres, biodegradable nano-microspheres, nanoparticles, polymeric microparticles, polymeric nanoparticles, steroidal nano microparticles, steroidal microparticles, silicon microneedles, and nanostructured lipid carriers.
[0425] In one embodiment, the extract of O. stamineus leaves can be incorporated into dendrimers. Dendrimers, or hyperbranched polymers, are synthetic polymeric
nanostructures having a unique spherical architecture with a central core that branches out and ends in polyvalent surface groups. The size and functionality of the dendrimer can be controlled by the number of branch reactions and the surface functionality provided by using different surface groups. Accordingly, the size and surface of dendrimer
nanostructures can be customized for the entrapment and delivery of the desired therapeutic agent and can be engineered to control pharmacokinetics and targeting for oral, mucosal, transdermal, or parenteral administration (168). The entrapment by the dendrimer allows both hydrophobic and hydrophilic molecules to be entrapped in a single dendrimer structure. Dendrimers with combinations of therapeutic agents are permissible. Accordingly, certain embodiments provide for dendrimers comprising the extract of O. stamineus leaves alone or in combination with other plant extracts, animal extracts, or monotherapeutic agents. Non-limiting examples of dendrimers that can be used include poly(amidoamine) (PAMAM), poly(propyleneimine) (PPI or DAB), poly(ethyleneimine) (PEL),
poly(etherhydroxylamine) (PEHAM), and derivatized hyperbranched polyglycerols (dHPGs), and have been described in (168), WO 2007149500 A2, U.S. Pat. No. 9,186,410 and
9,346,029.
[0426] As described herein, angiogenesis is a complex process under the control of both pro-angiogenic and anti-angiogenic factors. A tipping of the balance towards pro- angiogenesis can lead to abnormal vascular growth, which can result in a variety of angiogenesis related disorders described herein. However, in certain conditions, such as for example during the treatment of wounds, cuts, gunshot wounds, abrasions, surgical wounds, reconstructive surgery, diaper rash, eczema, burns, and other dermatological conditions requiring repair, it is advantageous to promote angiogenesis, cell migration, and
proliferation, and hence promote wound healing. This knowledge, together with the fact that angiogenesis and inflammation are intricately linked, can be used advantageously to formulate therapies for the treatment of certain disorders, primarily for dermal conditions that require wound healing, such that the formulation has a higher amount of a
therapeutically effective amount of pro-angiogenic factors and an effective amount of a therapeutic agent which can minimize inflammation. Such topical formulations promote angiogenesis sufficient for healing wounds, yet prevent abnormal vascular growth, and reduce or inhibit inflammation. Extracts of certain plants or animals can promote wound healing. One example of such an extract is derived from the Snakehead murrel (Channa striata) fish, a freshwater fish commonly found in Africa and parts of Asia, including
Indonesia and Malaysia. Hypoalbuminemia is a condition most often associated with post- operative patients, postpartum mothers or patients with severe wounds, and extracts of Channa striata have been shown to increase levels of albumin and accelerate the process of wound healing in these patients (169) (170). The ability of extracts of Channa striata to increase serum albumin has been attributed to striatin (DLBS0333), a bioactive protein fraction isolated from Channa striata (170).
[0427] In certain embodiments, topical formulations that require wound healing, can
comprise combinations of therapeutic agents comprising the extract of O. stamineus leaves present in an amount that is not anti-angiogenic, but is anti-inflammatory. In certain embodiments, at low concentrations and/or in combination with other plant and/or animal extracts which are strongly pro-angiogenic, the extract of O. stamineus leaves can have a predominantly anti-inflammatory effect. Accordingly, in certain embodiments, particularly in embodiments comprising the topical formulations described herein, the amount of the extract of O. stamineus leaves can comprise from 0.5% - 10% (e.g., 0.5, 0.6, 0.7, 0.8, 0.9, 1, 1.5, 2, 2.5, 3, 3.5, 4, 4.5, 5, 5.5, 6, 6.5, 7, 7.5, 8, 8.5, 9, 9.5, or 10%) by weight based on the total weight of the formulation.
[0428] One embodiment features a topical formulation for promoting wound healing, comprising, by weight based on the total weight of the formulation, (a) 0.5% - 10% (e.g., 0.5, 0.55, 0.6, 0.65, 0.7, 0.75, 0.8, 0.85, 0.9, 0.95, 1, 1.5, 2, 2.5, 3, 3.5, 4, 4.5, 5, 5.5, 6, 6.5, 7, 7.5, 8, 8.5, 9, 9.5, or 10%) of the extract of O. stamineus leaves comprising <0.2% (wt/wt of the extract of O. stamineus leaves) TMF, (b) 8% - 10% of virgin coconut oil (e.g., 8, 8.1, 8.2, 8.3, 8.4, 8.5, 8.6, 8.7, 8.8, 8.9, 9, 9.1, 9.2, 9.3, 9.4, 9.5, 9.6, 9.7, 9.8, 9.9 or 10%), (c) 10% - 15% of cetyl alcohol (e.g., 10, 10.2, 10.4, 10.6, 10.8, 11, 11.2, 11.4, 11.6, 11.8, 12, 12.2, 12.4, 12.6, 12.8, 13, 13.2, 13.4, 13.6, 13.8, 14, 14.2, 14.4, 14.6, 14.8, or 15%), (d) 0.5% - 1% of vitamin E (e.g., 0.5, 0.6, 0.7, 0.8, 0.9 or 1%), (e) 35% - 60% purified water (e.g., 35, 38, 40, 42, 44, 46, 48, 50, 52, 54, 56, 58 or 60%), (f) l% - 5% Malaysian Tualang honey (e.g., 1, 1.2, 1.4, 1.6, 1.8, 2, 2.2, 2.4, 2.6, 2.8, 3, 3.2, 3.4, 3.6, 3.8, 4, 4.2, 4.6, 4.8, or 5%), (g) 15% - 22% bee's wax (e.g., 15, 15.5 16, 16.5 17, 17.5, 18, 18.5, 19, 19.5, 20, 20.5, 21, 21.5 or 22%), and (h) 5% - 10% of Channa striata fish extract (e.g., 5, 5.5, 6, 6.5, 7, 7.5, 8, 8.5, 9, 9.5 or 10%) such that the total weight percent of (a) + (b) + (c) + (d) + (e) + (f) + (g) + (h) is 100%. In certain embodiments, component (a) can comprise 0.5% - 10% (e.g., 0.5, 0.55, 0.6, 0.65, 0.7, 0.75, 0.8, 0.85, 0.9, 0.95, 1, 1.5, 2, 2.5, 3, 3.5, 4, 4.5, 5, 5.5, 6, 6.5, 7, 7.5, 8, 8.5, 9, 9.5, or 10%) of the extract of O. stamineus leaves comprising <0.2% (wt/wt of the extract of O. stamineus leaves) TMF. In certain embodiments, component (a) can comprise 0.5% - 10% (e.g., 0.5, 0.55, 0.6, 0.65, 0.7, 0.75, 0.8, 0.85, 0.9, 0.95, 1, 1.5, 2, 2.5, 3, 3.5, 4, 4.5, 5, 5.5, 6, 6.5, 7, 7.5, 8, 8.5, 9, 9.5, or 10%) of the extract of O. stamineus leaves comprising <0.1% (wt/wt of the extract of O. stamineus leaves) TMF. In certain embodiments, component (a) can comprise 0.5% - 10% (e.g., 0.5, 0.55, 0.6, 0.65, 0.7, 0.75, 0.8, 0.85, 0.9, 0.95, 1, 1.5, 2, 2.5, 3, 3.5, 4, 4.5, 5, 5.5, 6, 6.5, 7, 7.5, 8, 8.5, 9, 9.5, or 10%) of the extract of O. stamineus leaves comprising <0.1% (wt/wt of the extract of O. stamineus leaves) TMF. In certain embodiments, this formulation can be formulated into any one or more of the nanotechnology structures described herein including ethosomes, phytosomes and/or dendrimers and incorporated into emulsions (e.g., oil-in-water, water-in-oil, silicon-in-water, water-in-silicon, water-in-oil-in-water, oil-in- water, oil-in-water-in-oil, oil-in-water-in-silicon, etc.), creams, lotions, solutions (both aqueous and hydro-alcoholic), anhydrous bases (such as lipsticks and powders), gels, ointments, pastes, milks, liquids, aerosols, sprays, solid forms, or eye jellies.
[0429] In one embodiment, a topical formulation comprising the extract of O.
stamineus leaves, virgin coconut oil, cetyl alcohol, vitamin E, purified water, Malaysian Tualang Honey, bee's wax, and Channa striata fish extract can further comprise, by weight based on the total weight of the topical formulation, TMF at greater that 0.1%. In other embodiments, the formulation can further comprise TMF, by weight based on the total weight of the formulation, from 0.1% - 2% (e.g., 0.11, 0.15, 0.2, 0.25, 0.3, 0.35, 0.4, 0.45,
0.5, 0.55, 0.6, 0.65, 0.7, 0.75, 0.8, 0.85, 0.9, 0.95, 1, 1.1, 1.2, 1.3, 1.4, 1.5, 1.6, 1.7, 1.8, 1.9, or 2%). In certain embodiments, this formulation can be formulated into any one or more of the nanotechnology structures described herein including ethosomes, phytosomes and/or dendrimers and incorporated into emulsions (e.g., oil-in-water, water-in-oil, silicon-in-water, water-in-silicon, water-in-oil-in-water, oil-in-water, oil-in-water-in-oil, oil-in-water-in-silicon, etc.), creams, lotions, solutions (both aqueous and hydro-alcoholic), anhydrous bases (such as lipsticks and powders), gels, ointments, pastes, milks, liquids, aerosols, sprays, solid forms, or eye jellies.
[0430] One embodiment for the method of manufacture of a topical formulation comprising the extract of O. stamineus leaves in combination with an extract of Channa striata fish and the wound healing properties of the combination is demonstrated in Example 29. The efficacy of the topical formulation in promoting various aspects of wound healing are shown in Figs. 10-15.
[0431] One embodiment features a topical formulation for promoting wound healing comprising a sophorolipid and a therapeutically effective amount of the extract of O.
stamineus leaves. In one embodiment, the efficacy of the topical formulation is
demonstrated in Example 27, Table 58B.
[0432] Certain embodiments comprise liquid preparations for oral administration comprising the extract of O. stamineus leaves. Such liquid preparations can be in the form of solutions, syrups or suspensions, or a dry product for reconstitution with water or another suitable vehicle before use. Such liquid preparations can be prepared by conventional means with pharmaceutically acceptable additives such as suspending agents, emulsifying agents, non-aqueous vehicles, and preservatives. Specific additives are well known to those of skill and are listed in places such as the U.S. Pharmacopeia and in (144), (145) or (146).
[0433] For administration by inhalation, formulations comprising the extract of O. stamineus leaves can be delivered in the form of an aerosol spray in a pressurized package or as a nebulizer, with use of excipients such as suitable propellants and additives. In the case of a pressurized aerosol, the dosage unit can be determined by providing a valve to deliver a metered dose. Specific additives for formulating inhalable formulations are well known to those of skill and are listed in places such as the U.S. Pharmacopeia and in and in (144), (145) or (146).
[0434] Parenterally administered formulations comprising the extract of O. stamineus leaves can formulated to allow for injection, either as a bolus or as a continuous infusion. In certain embodiments, the extract of O. stamineus leaves or formulations comprising the extract of O. stamineus leaves can be manufactured as unitary dosage forms or multi dose units, such as for example, in hermetically sealed glass ampules or other pharmaceutically acceptable, colored/tinted (including, for example, amber containers) or clear containers. In certain embodiments, the contents of said container can be reconstituted with either sterile water or other pharmaceutically acceptable aqueous solution (e.g., physiological saline) and introduced into an IV bag for intravenous administration. The formulations for injection can be in the form of powders, granules, suspensions, solutions, or emulsions, in either oily or aqueous vehicles including the various nanotechnology structures described herein. They can also contain formulatory agents such as suspending agents, stabilizing agents, and/or dispersing agents. Specific examples of formulating agents for parenteral injection are found in the U.S. Pharmacopeia.
[0435] In additional embodiments, the extract of O. stamineus leaves can be formulated for enteral administration. The formulations for enteral administration can be manufactured as described for parenteral administration, however, for enteral
administration, the formulations, can be delivered to a subject, preferably a human, via a suitable tube. Such tubes are well known in the art. For example, tubes that end in the stomach are called "gastric" tubes or "G tubes". A tube that ends in the initial segment of the small bowel (or small intestine), the duodenum, is called a duodenal tube. A tube inserted into the jejunum, the next section of the small bowel, is called a "J tube" or "jejunal tube". If a tube is inserted through the nose, it is called a "nasal" tube. A gastric tube inserted through the nose is called a "nasogastric tube" or "NG tube". Tubes inserted through the mouth are called "oral tubes". An "orogastric tube" or "OG tube" is a gastric tube that is inserted through the mouth. An "OJ tube" is a small bowel feeding tube (ending in the Jejunum) that is inserted through the mouth.
[0436] For rectal administration or vaginal administration, formulations for use comprising the extract of O. stamineus leaves can be formulated as suppositories, creams, gels, or retention enemas.
[0437] The extract of O. stamineus leaves can be formulated to include food compositions (functional foods), beverage compositions, over the counter, and dietary supplements. The extract of O. stamineus leaves can be added to various foods to be consumed simultaneously. Examples of food include, but are not limited to, confectionery such as sweets (candies, jellies, jams, etc.), gums, bean pastes, baked confectioneries or molded confectioneries (cookies, biscuits, etc.), steamed confectioneries, cacao or cacao products (chocolates and cocoa), frozen confectioneries (ice cream, ices, etc.), beverages (fruit juice, soft drinks, carbonated beverages), health drinks, health bars, and tea (green tea, black tea, etc.).
[0438] The dietary supplements can be in liquid form (e.g., solutions, syrups or suspensions) or can be in the form of a product for reconstitution with water or any other suitable liquid before use. Such liquid preparations can be prepared by conventional means such as a tea, health beverage, dietary shake, liquid concentrate, or liquid soluble tablet, capsule, pill, or powder such that the beverage can be prepared by dissolving the liquid soluble tablet, capsule, pill, or powder within a liquid and consuming the resulting beverage. Alternatively, the dietary supplements can take the form of tablets or capsules prepared by conventional means and optionally including other dietary supplements including vitamins, minerals, other herbal supplements, binding agents, fillers, lubricants, disintegrants, or wetting agents, as those discussed herein. The tablets can be coated as described herein. In one embodiment, the dietary supplement can take the form of a capsule, powder, or granule to be dissolved in a liquid for oral consumption.
[0439] Certain embodiments provide for functional foods comprising the extract of O. stamineus leaves either alone or in combination with other therapeutic agents (e.g., plant extracts, animal extracts, monotherapeutic agents, vitamins and/or minerals). The extract can be added to foods, which can then be consumed either alone or as part of a dietary treatment in addition to the other modes of administration of the formulations described herein as prescribed by a health professional.
[0440] In certain embodiments, the functional food can be in the form of edible or drinkable compositions, e.g., foodstuffs such as chewable or edible bars, confectionary
products (e.g., chocolate bars), cookies, juice drinks, baked or simulated baked goods (e.g., brownies), biscuits, lozenges or chewing gum. Examples of chewable or edible bars include chocolate bars or energy bars.
[0441] In certain embodiments, the functional foods can also be in the form of, for example, butter, margarine, bread, cake, milk shakes, ice cream, yogurt and other fermented milk products.
[0442] In certain embodiments, the functional food can also be in the form of a liquid to be sprayed on meats, salads or other foods.
[0443] Other forms of the functional foods can be breakfast cereals, such as for example, grain flakes, muesli, bran, oatmeal.
[0444] When the functional food product is in a drinkable form, the formulations described herein can be added directly to the drink, such as for example plain milk, flavored milk, fermented milk products or juices.
[0445] When the functional food is in the form of a solid edible product, the formulations comprising the extract of O. sfomineus leaves can be first formulated into an appropriate formulation (e.g., powders, granules nanostructures, or liquids), and can subsequently be either sprayed onto the solid edible product or mixed into the ingredients when manufacturing the edible product. The powders, granules, or nanostructures can be formulated to provide immediate release or modified release of the extract of O. stamineus leaves.
[0446] Certain embodiments provide for the use of kits. For instance, the extract of O. stamineus leaves or a formulation comprising the extract of O. stamineus leaves can be included in a kit. A kit can include a container. Containers can include a bottle, an ampule, a metal tube, a laminate tube, a plastic tube, a dispenser, a pressurized container, a barrier container, a package, a compartment, a lipstick container, a compact container, cosmetic pans that can hold cosmetic compositions, or other types of containers such as injection or blow-molded plastic containers into which the dispersions, formulations, desired bottles, dispensers, or packages are retained. The kit and/or container can include indicia on its surface. The indicia, for example, can be a word, a phrase, an abbreviation, a picture, or a symbol. A kit can also include instructions for using the kit and/or formulations. Instructions can include an explanation of how to apply, use, and maintain the formulations. The containers in the kit can dispense a pre-determined amount of a formulation comprising the extract of O. stamineus leaves. In other embodiments, the container can be squeezed (e.g., metal, laminate, or plastic tube) to dispense a desired amount of the formulation. The formulation can be dispensed as a spray, foam, an aerosol, a liquid, a fluid, or a semi-solid. The containers can have spray, pump, or squeeze mechanisms.
METHODS OF TREATMENT
[0447] Based on the various examples and experiments described herein, the extract of O. stamineus leaves or formulations comprising the extract of O. stamineus leaves either alone or in combination with other plant extracts, animal extracts, monotherapeutic agents, or combinations thereof can treat a variety of physiological disorders. In one embodiment, the extract of O. stamineus leaves or formulations comprising the extract of O. stamineus leaves has an anti-angiogenic activity , anti-inflammatory activity, antihypertensive activity, antihyperglycemic activity, antioxidant activity, anti-neurodegenerative activity,
neuroprotective activity, anti-pyretic activity, anti-gout activity, anti-microbial activity, antilithiatic activity, anti-ulcerogenic activity , anti-asthenic activity, anti-cachexic activity, or any combination thereof.
[0448] In one embodiment, the extract of O. stamineus leaves comprises an anti- angiogenic activity.
[0449] For example, in one embodiment, the extract of O. stamineus leaves can inhibit the proliferation and/or migration of endothelial cells. In another embodiment, the extract of O. stamineus leaves can inhibit the invasiveness of cancer cells. In one embodiment, the extract of O. stamineus leaves can inhibit capillary tube formation by endothelial cells. In one embodiment, the extract of O. stamineus leaves can inhibit neovascularization. In one other embodiment, the extract of O. stamineus leaves can inhibit the aggregation of cancer cells to form solid tumors. In one embodiment, the extract of O. stamineus leaves can modulate expression and/or activity of pro-angiogenic and/or anti-angiogenic factors such that the extract of O. stamineus leaves has an anti-angiogenic activity. In one embodiment, the extract of O. stamineus leaves can inhibit the expression and/or activity of factors that promote angiogenesis. In one embodiment, the extract of O. stamineus leaves can increase expression and/or activity of factors that inhibit angiogenesis. In one embodiment, the factor is a pro-angiogenic factor, anti-angiogenic factor, cytokine or combinations thereof. In one other embodiment, the factor is a pro-angiogenic factor, anti-angiogenic factor, chemokine, interleukin, interferon, lymphokine, tumor necrosis factor, growth factor, hormone, or any combination thereof. In one embodiment, the extract of O. stamineus leaves can downregulate the expression and/or activity of a receptor for a pro-angiogenic factor. In certain such embodiments, the receptor for the pro-angiogenic factor can be a receptor for a growth factor, hormone, chemokine, interleukin, interferon, lymphokine, tumor necrosis factor, or any combination thereof. In one embodiment, the extract of the O. stamineus leaves can up-regulate the expression and/or activity of a receptor for an anti- angiogenic factor. In certain such embodiments, the receptor for the anti-angiogenic factor can be a receptor for a growth factor, hormone, chemokine, interleukin, interferon, lymphokine, tumor necrosis factor, or any combination thereof.
[0450] In one embodiment, the extract of O. stamineus leaves can inhibit the expression and/or activity of VEGF, EGF, FGF, TGFot, NGF, IL-2, IL-7, TNF , or any
combination thereof. In one embodiment, the extract of O. stamineus leaves can inhibit expression and/or activity of a receptor for VEGF, EGF, FGF, TGFot, NGF, IL-2, IL-7, TNF , or any combination thereof. In one embodiment, the extract of O. stamineus leaves can increase expression and/or activity of GM-CSF, IFN-ot, IFN-β, or any combination thereof. In one embodiment, the extract of O. stamineus leaves can increase the expression and/or activity of a receptor for GM-CSF (CD116), IFN-ot, IFN-β, or any combination thereof. In one embodiment, the extract of O. stamineus leaves can inhibit expression of a gene HIF-la, WNT, KDR, COX2, or any any combination thereof. In one embodiment, the extract of O. stamineus leaves can inhibit further growth of tumors in a tumor bearing subject.
[0451] Based on at least the above embodiments, it will be apparent to the person that the extract of O. stamineus leaves can inhibit steps that are involved in angiogenesis, and hence can be used to treat an angiogenesis associated disorder.
[0452] Accordingly, one embodiment provides for a method of treating an
angiogenesis associated disorder in a subject in need thereof, said method comprising,
administering to the subject a therapeutically effective amount of the extract of O.
stamineus leaves or a formulation comprising a therapeutically effective amount of the extract of O. stamineus leaves for treating the angiogenesis associated disorder.
[0453] One embodiment provides for a method of inhibiting angiogenesis in a subject in need thereof, said method comprising, administering to the subject a therapeutically effective amount of the extract of O. stamineus leaves or a formulation comprising a therapeutically effective amount of the extract of O. stamineus leaves for modulating the expression and/or activity of a factor or plurality of factors such that the factor or plurality of factors inhibits or downregulates angiogenesis. For example, in embodiments where the extract of O. stamineus leaves modulates expression of a factor or plurality of factors such that the factor or plurality of factors inhibits angiogenesis, the level of expression and/or activity of the anti-angiogenic factors is sufficiently higher than the expression and/or activity of the pro-angiogenic factors, such that the overall effect of the extract of O.
stamineus leaves results in an inhibition of angiogenesis, and hence can treat an
angiogenesis associated disorder.
[0454] One embodiment provides for a method of treating an angiogenesis associated disorder in a subject in need thereof, said method comprising, administering to the subject a therapeutically effective amount of an extract of O. stamineus leaves or a formulation comprising a therapeutically effective amount of the extract of O. stamineus leaves such that the extract of O. stamineus leaves inhibits or downregulates the expression and/or activity of a factor or plurality of factors that promote angiogenesis. In certain such embodiments, the factor or plurality of factors is/are pro-angiogenic factors, cytokines, or any combination thereof. In certain embodiments, the cytokine is a chemokine, interleukin, interferon, lymphokine, tumor necrosis factor, or any combination thereof.
[0455] Certain embodiments provide for a method of treating an angiogenesis associated disorder in a subject in need thereof, said method comprising administering to the subject a therapeutically effective amount of the extract of O. stamineus leaves or a formulation comprising a therapeutically effective amount of the extract of O. stamineus leaves for downregulating the expression and/or activity of a receptor for a pro-angiogenic factor. In certain such embodiments, the receptor for the pro-angiogenic factor is a receptor for a growth factor, a hormone, a chemokine, an interleukin, an interferon, a lymphokine, a tumor necrosis factor, or any combination thereof.
[0456] One embodiment provides for a method of treating an angiogenesis associated disorder in a subject in need thereof, said method comprising, administering to the subject a therapeutically effective amount of the extract of O. stamineus leaves or a formulation comprising a therapeutically effective amount of the extract of O. stamineus leaves such that the extract of O. stamineus leaves treats the angiogenesis associated disorder by downregulating the expression and/or activity of VEGF, EGF, bFGF, TGF-ot, NGF , TNF , IL-2, IL-7, or any combination thereof.
[0457] One embodiment provides for a method of treating an angiogenesis associated disorder in a subject in need thereof, said method comprising, administering to the subject a therapeutically effective amount of the extract of O. stamineus leaves or a formulation comprising a therapeutically effective amount of the extract of O. stamineus leaves such that the extract of O. stamineus leaves downregulates expression and/or activity of a receptor for VEGF, EGF, FGF, TGFot, NGF, TNF , IL-2, IL-7 and any combination thereof.
[0458] Certain embodiments provide for a method of treating an angiogenesis associated disorder in a subject in need thereof, said method comprising, administering to the subject a therapeutically effective amount of the extract of O. stamineus leaves or a formulation comprising a therapeutically effective amount of the extract of O. stamineus leaves such that the extract of O. stamineus leaves up-regulates the expression and/or activity of a factor or plurality of factors that inhibit angiogenesis. In certain such embodiments, the factor or plurality of factors is/are anti-angiogenic factors, cytokines, or any combination thereof. In certain embodiments, the cytokine is a chemokine, interleukin, interferon, lymphokine, tumor necrosis factor, or any combination thereof.
[0459] Certain embodiments provide for a method of treating an angiogenesis associated disorder in a subject in need thereof, said method comprising, administering to the subject a therapeutically effective amount of the extract of O. stamineus leaves or a formulation comprising a therapeutically effective amount of the extract of O. stamineus leaves for up-regulating the expression and/or activity of a receptor for an anti-angiogenic factor. In certain such embodiments, the receptor for the anti-angiogenic factor is a receptor for a growth factor receptor, a hormone receptor, a chemokine receptor, an interleukin receptor, an interferon receptor, a lymphokine receptor, a tumor necrosis factor receptor, or any combination thereof.
[0460] One embodiment provides for a method of treating an angiogenesis associated disorder in a subject in need thereof, said method comprising, administering to the subject a therapeutically effective amount of an extract of O. stamineus leaves or a formulation comprising a therapeutically effective amount of the extract of O. stamineus leaves such that the extract of O. stamineus leaves up-regulates the expression and/or activity of GM-CSF, I FN-ot, IFN-β, or any combination thereof.
[0461] One embodiment provides for a method of treating an angiogenesis associated disorder in a subject in need thereof, said method comprising, administering to the subject a therapeutically effective amount of an extract of O. stamineus leaves or a formulation comprising a therapeutically effective amount of the extract of O. stamineus leaves such that the extract of O. stamineus leaves up-regulates the expression and/or activity of a receptor for GM-CSF (CD116), IFN-ot, I FN-β, or any combination thereof.
[0462] In one embodiment, the angiogenesis associated disorder is a tumorigenic disease, non-tumorigenic disease, or any combination thereof.
[0463] In one embodiment, the tumorigenic disease is any solid tumor, blood-borne cancer, or any combination thereof. One example of a solid tumor is any tumor beyond 2mm in diameter. Other non-limiting examples of solid tumors include, melanomas, sarcomas, adenocarcinomas, lymphomas, blastomas, skin cancers, and brain tumors.
[0464] Melanomas are cancers that start in melanocytes. Examples of melanomas include, without limitation, superficial spreading melanoma, nodular melanoma, lentigo maligna melanoma, acral lentiginous melanoma, mucosal melanoma, malignant melanoma, and ocular melanoma.
[0465] Sarcomas are cancers arising from connective tissue. Examples of sarcomas include, without limitation, osteosarcoma, angiosarcoma (more commonly referred to as hemangiosarcoma), epithelioid sarcoma, fibrosarcoma, Kaposi's sarcoma, liposarcoma, leiomyosarcoma, lymphangiosarcoma, neurofibrosarcoma, rhabdomyosarcoma, Ewing's sarcoma, and gastrointestinal stromal tumor.
[0466] Adenocarcinomas are cancers derived from epithelial cells of glandular tissues. Examples of adenocarcinomas include, without limitation, breast, prostate, lung, pancreas, ovarian, endometrium, testicles and colon carcinoma.
[0467] Blastomas are cancers derived from immature precursor cells or embryonic tissue. Examples of blastomas include, without limitation, retinoblastoma, neuroblastoma, hepatoblastoma, medulloblastoma, nephroblastoma, pancreatoblastoma, pleuropulmonary blastoma and glioblastoma multiforme.
[0468] Skin cancers can be divided into three main types i.e., basal-cell carcinoma, squamous-cell carcinoma, and malignant melanoma.
[0469] Brain tumors are categorized as primary or secondary. A primary brain tumor originates in the brain. Examples of primary brain tumors include, without limitation, gliomas, astrocytomas, oligodendroglial tumors, glioblastomas, meningiomas,
schwannomas, pituitary tumors, pineal gland tumors, ependymomas, craniopharyngiomas, primary brain lymphomas, primary central nervous system lymphomas, and primary germ cell tumors. Secondary brain tumors, also known as a metastatic brain tumors, occurs when cancer cells spread to the brain from another organ, such as lung or breast. Examples of tumors originating from other organs have been described herein.
[0470] Lymphomas are a group of blood cell tumors that develop from lymphocytes. Non-limiting examples of lymphomas include Hodgkin's lymphomas and non-hodgkin's lymphomas. The World Health Organization, however, includes two other categories as types of lymphoma - multiple myeloma and immunoproliferative diseases. Examples of immunoproliferative diseases include, without limitation, Wiskott-Aldrich syndrome, B-cell lymphomas, T-cell lymphomas, and follicular lymphoma.
[0471] Blood-borne cancers, or leukemias, are cancers of the blood cells. Non-limiting examples of such cancers include, acute lymphoblastic leukemia (ALL), acute myeloid leukemia (AML), chronic lymphocytic leukemia (CLL) and chronic myeloid leukemia (CML). Less common types of leukemia include, for example, hairy cell leukemia (HCL), T-cell prolymphocytic leukemia (T-PLL), large granular lymphocytic leukemia and adult T-cell leukemia, which is caused by human T-lymphotropic virus, a virus similar to HIV.
[0472] One embodiment features a method of treating a tumorigenic disease in a subject in need thereof, said method comprising, administering to the subject a
therapeutically effective amount of the extract of O. stamineus leaves or a formulation comprising a therapeutically effective amount of the extract of O. stamineus leaves such that the extract of O. stamineus leaves downregulates expression of a gene HIF-la, WNT, KDR, COX2, or any combination thereof.
[0473] Examples of non-tumorigenic diseases include, without limitation, retinopathies (e.g., diabetic retinopathy (171) (172) (173) (174), retinopathy of prematurity (previously referred to as retrolental fibroplasia) (172) (175), proliferative sickle cell retinopathy (176) and proliferative vitreoretinopathy (174)), corneal graft rejection (177), neovascular glaucoma (also referred to as hemorrhagic glaucoma, thrombotic glaucoma, congestive glaucoma, rubeotic glaucoma, and diabetic hemorrhagic glaucoma) (178), epidemic keratoconjunctivitis (179), atopic keratitis (180), superior limbic keratitis, pterygium (181) (182), Sjogren's syndrome (183), acne rosace (184) (185), phylectenulosis, syphilis (186), mycobacterial infections (187), infectious diseases wherein pathogens express angiogenic factors, such as for example, in Orf disease (188), infectious diseases wherein pathogens
induce angiogenic programs, such as for example, in certain Human Papilloma Virus (HPV) associated Infections (189), infectious diseases wherein pathogens transform endothelial cells (e.g., Kaposi's sarcoma (190)), lipid degeneration (191), gastrointestinal ulcers (192), oncolytic herpes simplex virus infections (180) (193), Herpes zoster infections (180), protozoan infections (194), Kaposi's sarcoma (190), chemical burns (182), Mooren's ulcer (182), Terrien's marginal degeneration (195), marginal keratolysis, trauma, osteoarthritis (e.g., non-inflammatory arthritis, inflammatory arthritis (rheumatoid arthritis), synovitis (synovial angiogenesis) (196) (197) (198) (199), systemic lupus (200) (201), polyarteritis nodosa (202), Wegener's sarcoidosis (203), Stevens-Johnson disease (182) (195), macular degeneration (e.g., Exudative (Wet), Nonexudative (Dry) Age-related Macular Degeneration (AM D) (172) (173) (204) (205)), Stargardt's disease (205), sickle cell anemia (206), interstitial lung diseases (e.g., sarcoidosis and idiopathic interstitial pneumonias (207)), corneal neovascularization (172) (e.g., in trachoma (208) and pseudoxanthoma elasticum (209)), Paget's disease of the vulva and breast (210), Paget's disease of the bone (211) (212), retinal vein occlusion (172) (213), chronic uveitis (214), chronic vitritis (155), Lyme's disease (182), Eales' disease (215), Behcet's disease (216), diseases related to choroidal neovascularization (205) (217), inflammatory bowel disease (e.g., Crohn's disease and ulcerative colitis) (218) (219) (220) (221), asthma (222), arterial/venous malformations (e.g., vascular
dysmorphogenesis) (205) (223), DiGeorge Syndrome (224), hereditary hemorrhagic telangiectasia (HHT) (also known as Osler-Weber- endu disease) (225), hemangiomas (226), obesity (227), cataracts (204), inflammatory skin diseases (e.g., psoriasis, dermatitis, warts, blistering disease) (228), periodontal disease (229) (230), peritoneal adhesions (231), endometriosis (232) (233) (234) (235), ocular neovascular disease (236) (237) (238), diseases related to female reproductive organs (e.g. dysfunctional uterine bleeding, ovarian hyperstimulation syndrome, polycystic ovary syndrome, myometrial fibroids (uterine leiomyomas) and adenomyosis (235) (239), diabetes (92) (93) (94) (95) (240) (241) (242) (243) (244), atherosclerosis (245), Bartonellosis (246), angiogenesis of the endocrine glands (247), (e.g., primary hyperparathyroidism (248), secondary hyperparathyroidism (249), and tertiary hyperparathyroidism (250), pyogenic granulomas (251), keloids (251), acoustin neuroma (also referred to as vestibular schwannomas) (252), and pulmonary hypertension (253) (254). Other non-tumorigenic diseases can include, for example, pars planitis, chronic retinal detachment, hyperviscosity syndromes, post-laser complications, abnormal proliferation of fibrovascular or fibrous tissue, diseases caused by chronic inflammation, infections causing retinitis or choroiditis, presumed ocular histoplasmosis, Best's disease and diseases associated with rubeosis (neovascularization of the angle).
[0474] One embodiment provides for a method of treating an angiogenesis associated disorder in a subject in need thereof, said method comprising, administering to the subject a therapeutically effective amount of the extract of O. stamineus leaves or a formulation comprising a therapeutically effective amount of the extract of O. stamineus leaves in combination with a therapeutically effective amount of one other therapeutic agent for the treatment of an angiogenesis associated disorder. In certain embodiments, the one other therapeutic agent for the treatment of an angiogenesis associated disorder can be a standard therapeutic agent for a certain type of an angiogenesis associated disorder. Non- limiting examples of the one other therapeutic agent for the treatment of an angiogenesis associated disorder that can be used in combination with the extract of O. stamineus leaves
include bevacizumab, girentuximab, imatinib, dasatinib, ramucirumab, axitinib, nilotinib, cabozantinib, ceritinib, lenvatinib, pazopanib, nintedanib, regorafenib, sorafenib, sunitinib, vandetanib, vatalanib, cetuximab, panitumumab, trastuzumab, axitinib, erlotinib, temsirolimus, everolimus, sirolimus, ziv-aflibercept, interferon alfa, lenalidomide, palomid 529, thalidomide, TAS-102, rhEndostatin, AKB-977, isothiocyanates, nitrogen mustard, nitrogen mustard-N-oxide hydrochloride, chlorambutyl, cyclophosphamide, ifosfamide, thiotepa, carboquone, improsulfan tosylate, busulfan, nimustine hydrochloride, mitobronitol, melphalan, dacarbazine, ranimustine, estramustine phosphate sodium, triethylenemelamine, carmustine, lomustine, streptozocin, pipobroman, etoglucid, carboplatin, cisplatin, miboplatin, nedaplatin, oxaliplatin, altretamine, ambamustine, dibrospidium hydrochloride, fotemustine, prednimustine, pumitepa, ribomustin, temozolomide, treosulphan, trophosphamide, zinostatin stimalamer, carboquone, adozelesin, cystemustine, bizelesin, mercaptopurine, fenofibrate, 6-mercaptopurine riboside, thioinosine, methotrexate, enocitabine, cytarabine, cytarabine ocfosfate, ancitabine hydrochloride, 5-FU drugs, aminopterine, leucovorin calcium, thioguanine, butocine, folinate calcium, levofolinate calcium, cladribine, emitefur, fludarabine, gemcitabine, hydroxycarbamide, pentostatin, piritrexim, idoxuridine, mitoguazone, thiazophrine, ambamustine, actinomycin-D, actinomycin-C, mitomycin-C, chromomycin-A3, bleomycin hydrochloride, bleomycin sulfate, peplomycin sulfate, daunorubicin
hydrochloride, doxorubicin hydrochloride, aclarubicin hydrochloride, pirarubicin hydrochloride, epirubicin hydrochloride, neocarzinostatin, mithramycin, sarcomycin, carzinophilin, mitotane, zorubicin hydrochloride, mitoxantrone hydrochloride, idarubicin hydrochloride, etoposide phosphate, vinblastine sulfate, vincristine sulfate, vindesine sulfate, teniposide, paclitaxel, docetaxel, vinorelbine, picibanil, krestin, sizofiran, lentinan, ubenimex, interferons, interleukins, macrophage colony-stimulating factor, granulocyte colony-stimulating factor, erythropoietin, lymphotoxin, BCG vaccine, Corynebacterium parvum, levamisole, polysaccharide K, procodazole, alitretinoin, imiquimod, polyphenon E, vismodegib, sonidegib, pegaptanib, ranibizumab, sonepcizumab, volociximab, afilbercept, conbercept, fumagillin, JSM6427, AL-78898A, ARC1905, Bevasiranib, siRNA 027, siRNA PF04523655, AdGVPEDF.llD, RetinoStat, sFltOl, MA09-hRPE, PF-05206388, iPS-derived RPE sheet, AMDCELL, CD34+ BMSC, corticosteroid implants, and combinations thereof. This list is not exclusive.
[0475] One embodiment provides for a method of decreasing the size of an existing capillary network in a subject in need thereof, wherein the growth and maintenance of the network depends on angiogenesis, said method comprising, administering to the subject a therapeutically effective amount of the extract of O. stamineus leaves or a formulation comprising a therapeutically effective amount of the extract of O. stamineus leaves for decreasing the size of an existing capillary network the growth and maintenance of which is dependent on angiogenesis. In one embodiment, the capillary network is associated with a tumorigenic disease, a non-tumorigenic disease, or any combination thereof. Non-limiting examples of tumorigenic and non-tumorigenic diseases have been described herein.
[0476] In one embodiment, the capillary network is associated with a tumor.
Accordingly, one embodiment features a method of inhibiting or slowing the growth of a preexisting tumor in a subject in need thereof, said method comprising, administering to the subject a therapeutically effective amount of the extract of O. stamineus leaves or a
formulation comprising a therapeutically effective amount of the extract of O. stamineus leaves for inhibiting or slowing the growth of the preexisting tumor. Thus, one embodiment provides for a method of providing progression free cancer survival of a subject diagnosed with the cancer, said method comprising, administering to the subject a therapeutically effective amount of the extract of O. stamineus leaves or a formulation comprising a therapeutically effective amount of the extract of O. stamineus leaves for the progression free survival from cancer in the subject.
[0477] In one embodiment, the capillary network is associated with corneal neovascularization. Accordingly, one embodiment features a method of inhibiting or slowing corneal neovascularization in a subject in need thereof, said method comprising, administering to the subject a therapeutically effective amount of the extract of O.
stamineus leaves or a formulation comprising a therapeutically effective amount of the extract of O. stamineus leaves for inhibiting or slowing corneal neovascularization.
[0478] In one embodiment, the capillary network is associated with retinal neovascularization. Accordingly, one embodiment features a method of inhibiting or slowing retinal neovascularization in a subject in need thereof, said method comprising, administering to the subject a therapeutically effective amount of the extract of O.
stamineus leaves or a formulation comprising a therapeutically effective amount of the extract of O. stamineus leaves for inhibiting or slowing retinal neovascularization. A related embodiment provides for a method of treating a retinopathy in a subject in need thereof, said method comprising, administering to the subject a therapeutically effective amount of the extract of O. stamineus leaves or a formulation comprising a therapeutically effective amount of the extract of O. stamineus leaves for the treatment of the retinopathy.
[0479] In one embodiment, the capillary network is associated with adipose fat tissue, wherein decreasing the capillary network decreases or inhibits the growth of the adipose fat tissue. Accordingly, one embodiment features a method of treating a subject diagnosed with diabetes, obesity, hyperglycemia, or any combination thereof, said method comprising, administering to the subject a therapeutically effective amount of the extract of O.
stamineus leaves or a formulation comprising a therapeutically effective amount of the extract of O. stamineus leave for the treatment of diabetes, obesity, hyperglycemia, or any combination thereof. One embodiment provides for a method of maintaining a healthy blood glucose level in a subject in need thereof, said method comprising, administering to the subject a therapeutically effective amount of the extract of O. stamineus leaves or a formulation comprising a therapeutically effective amount of the extract of O. stamineus leaves for maintaining healthy blood glucose levels.
[0480] In one embodiment, the extract of O. stamineus leaves can reduce multidrug resistance. Accordingly, one embodiment features a method for reducing multidrug resistance in a subject in need thereof, said method comprising, administering to the subject a therapeutically effective amount of the extract of O. stamineus leaves or a formulation comprising a therapeutically effective amount of the extract of O. stamineus leaves for reducing multidrug resistance.
[0481] One embodiment provides for a method of treating an angiogenesis associated disorder in a subject in need thereof, said method comprising, administering to the subject a therapeutically effective amount of the extract of O. stamineus leaves or a formulation comprising a therapeutically effective amount of the extract of O. stamineus leaves for
reducing multidrug resistance. In one embodiment, the angiogenesis associated disorder is a tumorigenic disease, a non-tumorigenic disease, or any combination thereof.
[0482] It is believed that because of the ability of the extract of O. stamineus leaves to reduce multidrug resistance of a cell, chemotherapy or long term treatment with standard therapy in combination with the extract of O. stamineus leaves will reduce resistance of ongoing chemotherapy or standard therapy for a physiological disorder, thus making the chemotherapy or standard therapy more efficacious. Thus, one embodiment provides for a method of enhancing the sensitivity of a tumor to a chemotherapeutic agent in a subject undergoing chemotherapy, said method comprising, administering to the subject a therapeutically effective amount of the extract of O. stamineus leaves or a formulation comprising a therapeutically effective amount of the extract of O. stamineus leaves prior to and/or during chemotherapy or in combination with standard therapy for enhancing the sensitivity of the tumor to the chemotherapeutic or standard therapeutic agent.
[0483] One embodiment provides for a method of treating an angiogenesis associated disorder in a subject in need of such treatment, said method comprising, administering to the subject a therapeutically effective amount of the extract of O. stamineus leaves or a formulation comprising a therapeutically effective amount of the extract of O. stamineus leaves as a neoadjuvant for the treatment of the angiogenesis associated disorder. In another embodiment, a method is provided for the treatment of an angiogenesis associated disorder in a subject in need thereof, said method comprising administering to the subject a therapeutically effective amount of the extract of O. stamineus leaves or a formulation comprising the extract of O. stamineus leaves as an adjuvant for the treatment of the angiogenesis associated disorder. In one embodiment, the angiogenesis associated disorder can be a tumorigenic disease. In one embodiment, the angiogenesis associated disorder can be a non-tumorigenic disease. In one embodiment, the tumorigenic disease is a solid tumor. In one embodiment, the tumorigenic disease is a blood-borne tumor.
[0484] In one embodiment, the extract of the O. stamineus leaves or formulations comprising the extract of the O. stamineus leaves can inhibit or downregulate the activity of CA9. CA9 has been shown to promote acidification of the extracellular environment, which promotes breakdown and remodelling of the extracellular matrix, and in turn contributes to the neovascularization process and metastasis of tumors. Accordingly, inhibiting or downregulating the activity of CA9 can treat an angiogenesis associated disorder by preventing the acidification of the extracellular environment and reducing intracellular pH to below 7, which would induce apoptosis and eventual necrosis of the tumor. Thus, one embodiment provides for a method of treating an angiogenesis associated disorder in a subject in need thereof, said method comprising, administering to the subject a
therapeutically effective amount of the extract of O. stamineus leaves or a formulation comprising a therapeutically effective amount of the extract of O. stamineus leaves for treating the angiogenesis associated disorder by inhibiting or downregulating the activity of CA9.
[0485] One embodiment provides for a method of treating a tumorigenic disease in a subject in need thereof, said method comprising, administering to the subject a
therapeutically effective amount of the extract of O. stamineus leaves or a formulation comprising a therapeutically effective amount of the extract of O. stamineus leaves for treating the tumorigenic disease by inhibiting or downregulating the activity of CA9.
[0486] In one embodiment, the extract of O. stamineus leaves comprises antiinflammatory activity. Thus, one embodiment provides for a method of inhibiting or downregulating the expression and/or activity of a proinflammatory factor or a plurality of proinflammatory factors in a subject in need thereof, said method comprising, administering to the subject a therapeutically effective amount of the extract of O. stamineus leaves or a formulation comprising a therapeutically effective amount of the extract of O. stamineus leaves for inhibiting and/or downregulating the expression and/or activity of the
proinflammatory factor or plurality of proinflammatory factors. In one such embodiment, the proinflammatory factor is a growth factor, a hormone, a chemokine, an interleukin, an interferon, a lymphokine, a tumor necrosis factor, or any combination thereof.
[0487] One embodiment provides for a method of inhibiting or downregulating the expression and/or activity of a receptor for a proinflammatory factor or a plurality of receptors for a plurality of proinflammatory factors in a subject in need thereof, said method comprising, administering to the subject a therapeutically effective amount of the extract of O. stamineus leaves or a formulation comprising a therapeutically effective amount of the extract of O. stamineus leaves for inhibiting and/or downregulating the expression and/or activity of the receptor or plurality of receptors for the proinflammatory factor or plurality of proinflammatory factors. In one such embodiment, the receptor for the proinflammatory factor is a growth factor receptor, a hormone receptor, a chemokine receptor, an interleukin receptor, an interferon receptor, a lymphokine receptor, a tumor necrosis factor receptor, or any combination thereof.
[0488] One embodiment provides for a method of treating inflammation or an inflammatory related disorder in a subject in need thereof, said method comprising, administering to the subject a therapeutically effective amount of the extract of O.
stamineus leaves or a formulation comprising a therapeutically effective amount of the extract of O. stamineus leaves for the treatment of inflammation or an inflammatory related disorder.
[0489] One embodiment provides for a method of inhibiting or downregulating the expression and/or activity of IL-1, IL-6, IL-8, TNF-a, COX-1, COX-2, or any combination thereof, in a subject in need thereof, said method comprising, administering to the subject a therapeutically effective amount of the extract of the O. stamineus leaves or a formulation comprising a therapeutically effective amount of the extract of the O. stamineus leaves for downregulating the expression and/or activity of IL-1, IL-6, IL-8, TNF-a, COX-1, COX-2 or any combination thereof. In certain embodiments, IL-1, IL-6, IL-8, TNF-a, COX-1, COX-2, or any combination thereof has proinflammatory activity.
[0490] One embodiment provides for a method of inhibiting or downregulating the expression and/or activity of a receptor for IL-1, IL-6, IL-8, TNF-a, or any combination thereof, in a subject in need thereof, said method comprising, administering to the subject a therapeutically effective amount of the extract of the O. stamineus leaves or a formulation comprising a therapeutically effective amount of the extract of the O. stamineus leaves for downregulating the expression and/or activity of a receptor for IL-1, IL-6, IL-8, TNF-a, or any combination thereof.
[0491] Non-limiting examples of an inflammatory related disorder includes asthma, chronic peptic ulcer, tuberculosis, chronic periodontitis, colitis, ulcerative colitis, Crohn's disease, chronic sinusitis, chronic active hepatitis, acne vulgaris, autoimmune diseases, celiac
disease, diabetes mellitus type 1, Graves disease, inflammatory bowel disease, multiple sclerosis, psoriasis, rheumatoid arthritis, and systemic lupus erythematosus,
autoinflammatory diseases (also known as periodic fever syndromes or auto inflammatory syndromes), chronic prostatitis, diverticulitis, glomerulonephritis, hidradenitis suppurativa, hypersensitivities, allergies, interstitial cystitis, otitis, pelvic inflammatory disease, reperfusion injury, rheumatic fever, sarcoidosis, transplant rejection, vasculitis,
atherosclerosis, myopathies, leukocyte defects, inflammation resulting from certain drugs or exogenous chemical compounds, cancer, HIV, AIDS, or any combination thereof.
[0492] Another embodiment contemplates a method of treating inflammation or an inflammatory related disorder in a subject, said method comprising, administering the extract of the O. stamineus leaves or formulations comprising the extract of the O.
stamineus leaves in combination with therapeutically effective amount of another therapeutic agent for the treatment of inflammation or an inflammatory related disorder. In certain embodiments, the other therapeutic agent can be a standard therapeutic agent for the treatment of a certain type of inflammation or inflammatory related disorder. Non- limiting examples of therapeutic agents for the treatment of inflammation include NSAIDS, salicylate, aspirin, diflunisal, salicylic acid, salsalate, propionic acid derivatives, ibuprofen, dexibuprofen, naproxen, fenoprofen, ketoprofen, dexketoprofen, flurbiprofen, oxaprozin, loxoprofen, acetic acid derivatives, indomethacin, tolmetin, sulindac, etodolac, ketorolac, diclofenac, aceclofenac, principal metabolite of nabumetone, enolic acid derivatives, piroxicam, meloxicam, tenoxicam, droxicam, lornoxicam, phenylbutazone, anthranilic acid derivatives, mefenamic acid, meclofenamic acid, flufenamic acid, tolfenamic acid, selective COX-2 inhibitors, celecoxib, parecoxib, lumiracoxib, etoricoxib, firocoxib, sulfonanilides, nimesulide, clonixine, licofelone, H-harpagide, corticosteroids, prednisone, Cortisol, prednisone, methylprednisolone, fludrocortisone, isoflupredone, triamcinolone, triamcinolone acetonide, dexamethasone, betamethasone, flumethasone, or any combination thereof.
[0493] As has been described herein, angiogenesis and inflammation are intricately linked and feed off each other. Inflammation sustains angiogenesis by the secretion of several factors (e.g., interferons, cytokines, chemokines, growth factors) by immune cells that act on endothelial cells either directly or indirectly. In turn, angiogenesis sustains inflammation by providing the necessary nutrients and oxygen to the cells present at sites of inflammation. Thus, in one embodiment, the anti-inflammatory activity of the extract of O. stamineus leaves would inherently enhance treatment of an angiogenesis associated disorder. Accordingly, one embodiment features a method of treating an angiogenesis associated disorder in a subject in need thereof, said method comprising, administering to the subject a therapeutically effective amount of the extract of O. stamineus leaves or a formulation comprising a therapeutically effective amount of the extract of O. stamineus leaves in combination with a therapeutically effective amount of an anti-inflammatory agent for the treatment of the angiogenesis associated disorder.
[0494] In one embodiment, the extract of O. stamineus leaves comprises antioxidant activity. As described herein, oxidative stress, which results in the production of OS, causes damage to essential cellular functions and is implicated as one cause in physiological disorders such as inflammation, cancer, atherosclerosis, aging, ischemic injury and neurodegenerative diseases. Thus, in one embodiment, the antioxidant activity of the
extract of O. stamineus leaves can treat atherosclerosis, aging, ischemic injury and neurodegenerative diseases and inherently enhance treatment of an angiogenesis associated disorder, inflammation or an inflammatory related disorder. One embodiment, therefore, provides for a method of increasing the antioxidant activity in a subject in need thereof, said method comprising, administering to the subject a therapeutically effective amount of the extract of O. stamineus leaves or a formulation comprising a therapeutically effective amount of the extract of O. stamineus leaves for increasing antioxidant activity in the subject. Another embodiment features a method of treating an angiogenesis associated disorder, an inflammatory or an inflammatory related disorder, atherosclerosis, ischemic injury or a neurodegenerative disease by increasing the antioxidant activity in a subject in need thereof, said method comprising, administering to the subject a therapeutically effective amount of the extract of O. stamineus leaves or a formulation comprising a therapeutically effective amount of the extract of O. stamineus leaves for treating an angiogenesis associated disorder, an inflammatory or an inflammatory related disorder, atherosclerosis, ischemic injury or a neurodegenerative disease by increasing the antioxidant activity in the subject.
[0495] One other embodiment provides for a method of treating a skin condition comprising, topically applying to skin in need thereof a therapeutically effective amount of the extract of O. stamineus leaves or a formulation comprising a therapeutically effective amount of the extract of O. stamineus leaves, wherein the extract or formulation increases the antioxidant activity in the skin. Non-limiting examples of skin conditions include dry skin, flaky skin, chapped skin, pruritus, spider veins, lentigo, age spots, senile purpura, keratosis, melasma, blotches, nodules, sun damaged skin, dermatitis (including, but not limited to seborrheic dermatitis, nummular dermatitis, contact dermatitis, atopic dermatitis, exfoliative dermatitis, perioral dermatitis, and stasis dermatitis), psoriasis, folliculitis, rosacea, acne, impetigo, erysipelas, erythrasma, eczema, sun burns, burned skin, open wounds, skin- inflammatory skin conditions, exposure to UV light, age, irradiation, chronic sun exposure, environmental pollutants, air pollution, wind, cold, heat, chemicals, disease pathologies, smoking, lack of nutrition, and skin cancer (including, but not limited to basal- cell carcinoma, squamous-cell carcinoma, and malignant melanoma). The topical formulation can be a cosmeceutical.
[0496] One embodiment provides for a method of treating a skin condition comprising, topically applying to skin in need thereof a therapeutically effective amount of the extract of O. stamineus leaves or a formulation comprising a therapeutically effective amount of the extract of O. stamineus leaves in combination with a therapeutically effective amount of another antioxidant. A related embodiment provides for a method of treating a skin condition comprising, topically applying to skin in need thereof a topical formulation comprising a therapeutically effective amount of the extract of O. stamineus leaves or a formulation comprising a therapeutically effective amount of the extract of O. stamineus leaves, in combination with a therapeutically effective amount of another antioxidant and a therapeutically effective amount of an anti-inflammatory agent. The topical formulation can be a cosmeceutical.
[0497] One embodiment provides for a method of treating a skin condition comprising topically applying to skin in need thereof a topical formulation comprising a therapeutically effective amount of the extract of O. stamineus leaves or a formulation comprising a
therapeutically effective amount of the extract of O. stamineus leaves to reduce
inflammation in combination with a therapeutically effective amount of another plant and/or animal extract which promotes angiogenesis. In one embodiment, the other plant and/or animal extract is a plant extract. In one embodiment, the other plant and/or animal extract is an animal extract. In one embodiment, the animal extract can be an extract of Channa striata fish. The topical formulation can be cosmeceutical.
[0498] The extract of O. stamineus leaves comprises blood-glucose lowering activity. Thus, one embodiment provides for a method of lowering blood glucose in a subject in need thereof, said method comprising, administering to the subject a therapeutically effective amount of the extract of O. stamineus leaves or a formulation comprising a therapeutically effective amount of the extract of O. stamineus leaves for lowering blood glucose. One embodiment features a method of treating diabetes, obesity, hyperglycemia, or any combination thereof in a subject in need thereof, said method comprising, administering to the subject a therapeutically effective amount of the extract of O. stamineus leaves or a formulation comprising the extract of O. stamineus leaves for the treatment of diabetes, obesity, hyperglycemia, or any combination thereof.
[0499] One embodiment, features a method of lowering blood glucose in a subject in need thereof, said method comprising, administering to the subject a therapeutically effective amount of the extract of O. stamineus leaves or a formulation comprising a therapeutically effective amount of the extract of O. stamineus leaves in combination with a therapeutically effective amount of another active agent for lowering blood glucose. In one embodiment, the other therapeutic agent for lowering blood glucose can be a standard therapeutic agent for the use of lowering blood glucose. Non-limiting examples of other therapeutic agents for lowering blood glucose include alpha-glucosidase inhibitors (e.g., acarbose), biguanides (e.g., metformin), DPP-4 inhibitors (e.g., alogliptin, linagliptin, sitagliptin, saxagliptin), GLP-1 receptor agonists (e.g., albiglutide, exenatide, liraglutide), insulin and its analogues (e.g., bolus insulins, basal insulins, premixed insulins), insulin secretagogues (e.g., sulfonylureas, meglitinides), SGLT2 inhibitors (e.g., canagliflozin, dapagliflozin, empagliflozin), TZDs (e.g., pioglitazone, rosiglitazone), weight loss agents that inhibit lipase (e.g., orlistat), or any combination thereof.
[0500] The extract of O. stamineus leaves can inhibit or downregulate the expression and/or activity of ACE-I. Thus, one embodiment provides for a method of inhibiting or downregulating the expression and/or activity of ACE-I in a subject in need thereof, said method comprising, administering to the subject a therapeutically effective amount of the extract of O. stamineus leaves or a formulation comprising a therapeutically effective amount of the extract of O. stamineus leaves for inhibiting or downregulating the activity of ACE-I. As described herein, ACE-I regulates arterial blood pressure and electrolyte balance by triggering vasoconstriction of blood vessels and degrades bradykinin, which is a potent vasodilator in the AAS. Therefore, inhibition of ACE-I is a promising target for regulation and treatment of high blood pressure. Accordingly, one embodiment provides for a method of treating hypertension in a subject in need thereof, said method comprising, administering to the subject a therapeutically effective amount of the extract of O. stamineus leaves or a formulation comprising a therapeutically effective amount of the extract of O. stamineus leaves for treating hypertension by inhibiting or downregulating the expression or activity of ACE-I. Certain embodiments feature a method of inhibiting or downregulating the activity of
ACE-I in a subject in need thereof, said method comprising, administering a therapeutically effective amount of the extract of O. stamineus leaves or a formulation comprising a therapeutically effective amount of the extract of O. stamineus leaves in combination with a therapeutically effective amount of another active agent that inhibits or downregulates ACE- I activity. In a related embodiment, a method is provided for the treatment of hypertension in a subject in need thereof, said method comprising, administering to said subject a therapeutically effective amount of the extract of O. stamineus leaves or a formulation comprising the extract of O. stamineus leaves in combination with a therapeutically effective amount of another antihypertensive agent for treating hypertension. In one embodiment, the other antihypertensive agent can be a standard therapeutic agent for the use of treating hypertension. Non-limiting examples of other antihypertensive active agents or active agents that inhibit or downregulate ACE-I activity include thiazide diuretics (e.g., hydrochlorothiazide, chlorthalidone), beta blockers (e.g., acebutolol, atenolol), angiotensin- converting enzyme inhibitors (e.g., lisinopril, captopril), angiotensin II receptor blockers (e.g., candesartan, losartan), calcium channel blockers (e.g., diltiazem, amlodipine), renin inhibitors (e.g., aliskiren), alpha blockers (e.g., doxazosin, prazosin), alpha-beta blockers (e.g., carvedilol, labetalol), centrally-acting agents (e.g., clonidine, guanfacine, methyldopa) , vasodilators (e.g., hydralazine, minoxidil), aldosterone antagonists (e.g., spironolactone, eplerenone), or any combination thereof.
[0501] The extract of O. stamineus leaves can inhibit or downregulate the expression and/or activity of AChE. Thus, one embodiment provides for a method of inhibiting or downregulating AChE activity in a subject in need thereof, said method comprising, administering to the subject a therapeutically effective amount of the extract of O.
stamineus leaves or a formulation comprising the extract of O. stamineus leaves for inhibiting or downregulating AChE activity. As described herein, neurodegenerative diseases, particularly those affected by the cholinergic system, are characterized neurochemical^ by a consistent deficit in cholinergic neurotransmission. The aim of therapies for the treatment of such neurodegenerative diseases has been to target inhibition of AChE, thereby enabling accumulation of acetylcholine in the synaptic cleft and neuromuscular junction, which then allows for prolonged activation of post-synaptic neurons or contraction of muscle.
Accordingly, inhibition of AChE activity can treat neurological disorders. Thus, one embodiment provides a method for the treatment of a neurological disorder in a subject in need thereof, said method comprising, administering to the subject a therapeutically effective amount of the extract of O. stamineus leaves or a formulation comprising a therapeutically effective amount of the extract of O. stamineus leaves for the treatment of the neurological disorder by inhibiting or downregulating the expression of AChE activity. Non-limiting examples of neurological disorders include, AD, PD, dementia, DLB, movement disorders (e.g., myasthenia gravis), and ALS. Certain embodiments feature a method of inhibiting or downregulating AChE activity in a subject in need thereof, said method comprising, administering to the subject a therapeutically effective amount of the extract of O. stamineus leaves or a formulation comprising the extract of O. stamineus leaves for inhibiting or downregulating AChE activity in combination with another active agent which inhibits or downregulates AChE activity. Certain other embodiments feature a method of treating a neurodegenerative disorder in a subject, said method comprising, administering to the subject a therapeutically effective amount of the extract of O. stamineus leaves or a
formulation comprising a therapeutically effective amount of the extract of O. stamineus leaves in combination with another therapeutic agent for the treatment of the
neurodegenerative disorder. Non-limiting examples of AChE inhibitors or therapeutic agents for the treatment of neurodegenerative disorders include dabigatran, apixaban, rivaroxaban, aspirin, carbidopa-levodopa, dopamine agonists (e.g., pramipexole, ropinirole, rotigotine, apomorphine), MAO-B inhibitors (e.g., selegiline, rasagiline), COMT inhibitors (e.g., entacapone, tolcapone), anticholinergics (e.g., benztropine, trihexyphenidyl), amantadine, cholinesterase inhibitors (e.g., donepezil, galantamine, rivastigmine), antioxidants, curcumin, crocin, erythropoietin, omega-3 fatty acids, lithium, minocycline, nicotine, pyrroloquinoline quinone, resveratrol, vinpocetine, progesterone, statins, noopept, L-theanine, estrogen, caspase inhibitors, cannabinoids, bacopa monnieri, anti-protein aggregation agents (e.g., sodium 4-phenylbutyrate, trehalose, and polyQ-binding peptide), acetylcysteine, acetyl-L- carnitine, caffeine, memantine, or any combination thereof.
[0502] One embodiment of a combination therapy provides for a method of treating inflammation or inflammatory related disorder, angiogenesis associated disorder, atherosclerosis, aging, ischemic injury and neurodegenerative diseases, said method comprising administering a therapeutically effective amount of the extract of O. stamineus leaves or a formulation comprising the extract of O. stamineus leaves in combination with a therapeutically effective amount of an antioxidant. Non-limiting examples of antioxidants include retinol, ascorbic acid, tocopherol, tocotrienol, Coenzyme Q10, manganese, iodide, melatonin, carotenoid terpenoids, flavonoids, phenolic acids and their esters, curcumin, flavonolignans, xanthones, eugenol, capsaicin, bilirubin, citric acid, oxalic acid, phytic acid, N- Acetylcysteine, -alpha-lipoic acid, and uric acid. Non-limiting examples of carotenoid terpenoids include alpha-carotene, astaxanthin, beta-carotene, canthaxanthin, lutein, lycopene, and zeaxanthin. Non-limiting examples of flavonoids include, flavones, flavonols and their polymers, flavanones, isoflavones, stilbenoids, and anthocyanins. Non-limiting examples of phenolic acids and their esters include chicoric acid, chlorogenic acid, cinnamic acid, ellagic acid, ellagitannins, gallic acid, gallotannins, salicylic acid, and combinations thereof. In one embodiment, the other therapeutic agent for the treatment of a
neurodegenerative disorder can be a standard therapeutic agent for the treatment of the particular neurodegenerative disorder.
[0503] One embodiment of a combination therapy provides for a method of treating an angiogenesis associated disorder in a subject in need thereof, said method comprising administering to the subject a first, second and third therapeutic agent, wherein the first, second and third therapeutic agent are different from each other, and wherein the first therapeutic agent is a therapeutically effective amount of the extract of O. stamineus leaves or a formulation comprising a therapeutically effective amount of the extract of O.
stamineus leaves, the second therapeutic agent is a therapeutically effective amount of an anti-angiogenic agent, and the third therapeutic agent is a therapeutically effective amount of an anti-inflammatory agent or an agent for the treatment of an inflammatory related disorder. In certain embodiments, the therapeutic agents for the treatment of the angiogenesis associated disorder, inflammation or the inflammatory related disorder can be the standard therapeutic agent for the respective disorder.
[0504] Another embodiment provides for a method of treating an angiogenesis associated disorder in a subject, said method comprising administering a first, second, third,
and fourth therapeutic agent, wherein the first, second, third, and fourth therapeutic agents are different from each other, and wherein the first therapeutic agent is a therapeutically effective amount of the extract of O. stamineus leaves or a formulation comprising a therapeutically effective amount of the extract of O. stamineus leaves, the second therapeutic agent is a therapeutically effective amount of an anti-angiogenic agent, the third therapeutic agent is a therapeutically effective amount of an anti-inflammatory agent or an agent for the treatment of an inflammatory related disorder, and the fourth therapeutic agent is an antioxidant. In certain embodiments, the therapeutic agents for the treatment of the angiogenesis associated disorder, inflammation or the inflammatory related disorder can be the standard therapeutic agent for the respective disorder.
[0505] In certain embodiments, the extract of the O. stamineus leaves or formulations comprising the extract of the O. stamineus leaves can inhibit angiogenesis by at least 40% (e.g., 40, 45, 50, 55, 60, 65, 70, 75, 80, 85, 90, 95 or 100%). In certain embodiments, the extract of the O. stamineus leaves or formulations comprising the extract of the O.
stamineus leaves can inhibit endothelial cell migration by at least 40% (e.g., 40, 45, 50, 55, 60, 65, 70, 75, 80, 85, 90, 95 or 100%). In certain embodiments, the extract of the O.
stamineus leaves or formulations comprising the extract of the O. stamineus leaves can inhibit tumor growth by at least 40% (e.g., 40, 45, 50, 55, 60, 65, 70, 75, 80, 85, 90, 95 or 100%). The level of inhibition can be in vitro or in vivo.
[0506] Asthenia or Asthenia Fatigue Syndrome (AFS), is a common symptom which accompanies a large variety of endocrine, neurological and psychiatric disorders, metabolic disorders, drugs, various inflammatory diseases, and most frequently in advanced cancer. In cancer patients, asthenia is characterized by fatigue of a pathological degree, poor endurance, and impaired motor and cognitive function. Cachexia is characterized by weight loss, lipolysis, muscle wasting, anorexia, chronic nausea, and asthenia, with resulting changes in body image and psychological distress. Cachexia and asthenia commonly coexist, but can manifest independently of each other. Pathological fatigue is differentiated from physiological fatigue, which often follows strenuous exercise, work, lack of sleep or stress. Various chemotherapy drugs, pain and psychotropic medications, radiation therapy and surgery can be responsible for, or at least contribute to, asthenia and cachexia in cancer patients. It has been reported that at least 70% of cancer patients experience asthenia at some point during their illness or therapy (255), while cachexia occurs in more than 80% of patients with advanced cancer (256). Although the etiology cachexia and asthenia is still unknown, recent research suggests cytokines such as TNF-ot (257) IL-1, IL-6, and INFs (258) might play a role. The extract of O. stamineus inhibits or downregulates activity of these cytokines, and accordingly, can treat asthenia and cachexia. Thus, one embodiment provides for a method of treating or ameliorating asthenia in a subject in need thereof, said method comprising, administering to the subject a therapeutically effective amount of the extract of O. stamineus leaves or a formulation comprising a therapeutically effective amount of the extract of O. stamineus leaves for the treatment or amelioration of asthenia. Another embodiment, provides for a method of treating or ameliorating cachexia in a subject in need thereof, said method comprising, administering to the subject a therapeutically effective amount of the extract of O. stamineus leaves or a formulation comprising a therapeutically effective amount of the extract of O. stamineus leaves for the treatment or amelioration of cachexia. In certain embodiments, the method of treating asthenia and/or cachexia can be
treated with a therapeutically effective amount of the extract of O. stamineus leaves or a formulation comprising a therapeutically effective amount of the extract of O. stamineus leaves in combination with a therapeutically effective amount of any one or more of the following therapeutic agents: thalidomide, clenbuterol, melatonin, growth hormone, anabolic steroids/androgens, cannabinoids, Omega-3 fatty acids, NSAIDS or combinations thereof.
[0507] Certain other embodiments provide for the use of a therapeutically effective amount of the extract of O. stamineus leaves or a formulation comprising a therapeutically effective amount of the extract of O. stamineus leaves either alone or in combination with another therapeutic agent for the treatment of lithiasis, gout, microbial infections, stomach ulcers, fever, or liver disease. In certain embodiments, the lithiasis includes
cholecystolithiasis, nephrolithiasis, pancreatolithiasis, urolithiasis, or any combination thereof.
[0508] In certain embodiments, the subject being treated is a mammal, including but not limited to a dog, cat, horse, cow, pig, sheep, goat, chicken, rodent, primate or human. In certain embodiments, the human subject can be a pediatric, adult, or a geriatric subject, and can be of either gender. In other embodiments, the subjects include animals such as house pets (e.g., dogs, cats, and the like), agricultural stock subjects (e.g., cows, horses, pigs, chickens, etc.), laboratory subjects (e.g., mice, rats, rabbits, etc.), but are not so limited. Typically, the subject is a human.
[0509] The dose of the extract of O. stamineus leaves administered to the subject can depend on the type and severity of the disease and on the characteristics of the subject, such as subject type (i.e., human or animal), general health, age, sex, body weight and tolerance to drugs. A skilled person will be able to evaluate appropriate dosages depending on these and other factors. Typically, an effective amount of the extract of O. stamineus leaves can be sufficient for achieving a therapeutic or prophylactic effect. Subject test doses can be extrapolated from effective doses in cell studies, such as IC5o values, or from effective doses in vivo by extrapolating on a body weight or surface area basis. Such extrapolations are routine in the art (259) (260) (261). In certain embodiments calling for combination therapy, there can be a synergistic effect between the extract of O. stamineus and the additional therapeutic agent being administered. Accordingly, the dose of the extract of the O. stamineus leaves and the one or more additional therapeutic agent(s) being administered can be different from the dose when the extract of O. stamineus leaves and the one or more additional therapeutic agent(s) are administered individually. A skilled person will be able to evaluate the appropriate dose for each therapeutic agent in such cases.
[0510] Alternatively, the efficacy and dosage strength of the extract of O. stamineus leaves for the treatment of a physiological disorder can be personalized for a subject type and the type and severity of the physiological disorder. For example, one embodiment provides for a method of determining the dosage strength of the extract of O. stamineus leaves for the treatment of a tumorigenic disease in a subject in need thereof, said method comprising, harvesting the tumor (e.g., during a biopsy), culturing cells of the tumor and determining the effect of the extract of the O. stamineus leaves at serial concentrations as measured and described herein. Subject test doses can then be extrapolated from effective doses in cell studies, such as IC5o values, or from effective doses in vivo by extrapolating on a body weight or surface area basis. A similar evaluation can be done in the presence of
additional therapeutic agents when combination therapy can be the treatment of choice as decided by the skilled person. This analysis, together with the route of administration and the type of dosage form can provide an optimal dose of the extract of O. stamineus leaves either alone or in combination with one or more therapeutic agent(s) for the treatment of the tumorigenic disease or other physiological disorder.
[0511] Typically, the dose of the extract of O. stamineus leaves can comprise from 100 mg - 2000 mg of the extract of the O. stamineus leaves (e.g., 100, 125, 150, 175, 200, 225, 250, 275, 300, 325, 350, 375, 400, 425, 450, 475, 500, 525, 550, 575, 600, 625, 650, 675, 700, 725, 750, 775, 800, 825, 850, 875, 900, 925, 950, 975, 1000, 1025, 1050, 1075, 110, 1125, 1150, 1175, 1200, 1225, 1250, 1275, 1300, 1325, 1350, 1375, 1400, 1425, 1450, 1475, 1500, 1525, 1550, 1575, 1600, 1625, 1650, 1675, 1700, 1725, 1750, 1775, 1800, 1825, 1850, 1875, 1900, 1925, 1950, 1975, or 2000 mg). In certain embodiments, the formulations comprise 250mg - lOOOmg (e.g., 250, 260, 270, 280, 290, 300, 310, 320, 330, 340, 350, 360, 370, 380, 390, 400, 410, 420, 430, 440, 450, 460, 470, 480, 490, 500, 510, 520, 530, 540, 550, 560, 670, 580, 590, 600, 610, 620, 630, 640, 650, 660, 670, 680, 690, 700, 710, 720, 730, 740, 750, 760, 770, 780, 790, 800, 810, 820, 830, 840, 850, 860, 870, 880, 890, 900, 910, 920, 930, 940, 950, 960, 970, 980, 990, or 1000 mg) of the extract of O. stamineus leaves. In certain
embodiments, the dose comprises 250mg of the extract of O. stamineus leaves. In certain other embodiments, the dose comprises lOOOmg of the extract of O. stamineus leaves.
[0512] Depending on the subject type and the type, severity and location of the physiological disorder, the routes of administration may vary and can include enteral, parenteral, or a combination thereof. Examples of enteral routes of administration include oral or rectal.
[0513] Non-limiting examples of oral routes of administration include sublingual, sublabial, buccal, digestive tract, and respiratory tract. Non-limiting examples of dosage forms of formulations suitable for sublingual, sublabial, and buccal delivery include sublingual films, sublabial films, buccal films, ointments, gels, dendrimers, oral sprays, orally disintegrating tablets, lozenges, effervescent tablets, sublingual drops, lollipops, and chewing gums. Non-limiting examples of dosage forms or formulations suitable for delivery via the digestive tract include solid immediate release or modified release dosage forms (e.g. tablets, microspheres, granules, powders, etc.), capsules, gelcaps, pastilles, multiparticulates (e.g., microspheres, granules, powder), mini tablets, caplets, effervescent powder, effervescent tablets, hydrogels, syrups, and straws (see US Pat. No. 5,780,058; 5,718,681; and 8,334,003).
[0514] Non-limiting examples of dosage forms or formulations suitable for delivery via the respiratory tract include dry-powder inhalers, nebulizers, metered dose inhalers, and aerosol devices (e.g., e-cigarettes).
[0515] Non-limiting examples of dosage forms or formulations for rectal delivery include suppositories, gels, hydrogels, dendrimers, and specialized catheters (e.g., Macy Catheter).
[0516] Examples of parenteral routes of administration include extra-amniotic administration, intraarterial, intraarticular, intracardiac, intracavernous, intradermal, intralesional, intramuscular, intracerebral, intracerebroventricular, intraocular, intraosseous, intraperitoneal, intrathecal, intravaginal, intravenous, intravesical, ophthalmic, otologic, urogenital, dermal, epidural, and subcutaneous. One of example of a dosage form suitable
for extra-amniotic administration, intraarterial, intraarticular, intracardiac, intracavernous, intradermal, intralesional, intramuscular, intracerebral, intracerebroventricular, intraocular, intraosseous, intraperitoneal, intrathecal, intravenous, epidural, intravesical, intravitreal, and subcutaneous is an injectable.
[0517] Non-limiting examples of dosage forms or formulations for intravaginal administration include vaginal tablets, vaginal creams, vaginal suppositories, and vaginal rings.
[0518] Non-limiting examples of dosage forms or formulations suitable for dermal administration include dermal patches, transdermal patches, gels, hydrogels, ethosomes, niosomes, discosomes, phytosomes, liposomes, lotions, lip balms, ointments, creams, emulsions, topical sprays, and medicated shampoos.
[0519] Administration routes for the treatment of ophthalmic physiological disorders include topical, oral/systemic, intravitreal, intracameral, transscleral and combinations thereof (262). The transscleral delivery route can be further subdivided into subconjunctival, subtenon, retrobulbar, and peribulbar delivery routes (262). Non-limiting examples of dosage forms or formulations suitable for ophthalmic delivery include eye drops, hydrogels, ointments, injectables, topical emulsions, microparticles, biodegradable microparticles, biodegradable microspheres, biodegradable nano-microspheres, mini tablets, nanoparticles, polymeric microparticles/nanoparticles, steroidal nano- and microparticles, silicon microneedles, nanostructured lipid carriers, and dendrimers (262).
[0520] Administration routes for the treatment of otologic physiological disorders include oral/systemic, intratympanic, intracochlear, and combinations thereof (263). Non- limiting examples of suitable dosage forms for the delivery of therapeutic agents via the otologic route include, the oral formulations and dosage forms described herein, sustained release systems (e.g., hydrogels, nanoparticles) and commercially available cannula based delivery systems (e.g., Silverstein Microwick™ or Round Window Microcatheter) (263). Non- limiting examples of sustained release systems include hydrogels and nanoparticles (263).
[0521] Non-limiting examples of hydrogels include, biodegradable gelatin polymers (e.g., Gelfoam®, Pfizer, U.S.A.), hyaluronic acid based hydrogels (e.g., hyaluronic acid- carboxymethyl cellulose polymer, commercially available as Seprapack™, Genzyme
Corporation and thiol modified hyaluronic acid), glutaraldehyde cross linking of porcine type-collagen, gelatin, chitosan glycosylated derivative, temperature sensitive polymers (e.g., sol-gel polymers, such as for example, Poloxamer 407), and chitosan glycerophosphate hydrogel (263).
[0522] The following examples provide those of ordinary skill with a complete disclosure and description of how the extract of O. stamineus leaves, and formulations comprising said extract are made, used and evaluated, and are intended to be purely exemplary of the invention and are not intended to limit the scope of what the inventors regard as their invention.
EXAMPLES
Example 1. Method of Manufacturing a Countercurrent Exchange Extract (CCEe) of O.
stamineus Leaves
[0523] O. stamineus leaves were purchased from Herbagus Sdn. Bhd. (Kepala Batas, Penang, Malaysia). 90 kg of cleaned, dried and shredded (particle size not less than 3mm)
leaves of O. stamineus was loaded in the extraction vessel of a 500 DIG-MAZ® extractor (Samtech Extraktionstechnik GmbH, Jagerzeile 34, Mannersdorf, Austria 2452). The temperature of the extraction vessel jacket was set to 60°C and a vacuum of -550 mbar was created in the extraction vessel once the lid of the extraction vessel was closed and locked. 800 liters of 50% EtOH solvent (1:1 reverse osmosis water and EtOH) was placed in the solvent tank of the extractor. The solvent was preheated to 60°C using a heat-exchanger. Once the extraction vessel and solvent reached their desired vacuum pressure and temperature respectively, the extraction vessel was filled with the pre-heated solvent from the bottom of the vessel to displace all the traces of air and to avoid any possible air bubbles in the extraction vessel. The flow of the solvent was set to 800L/hr throughout the extraction process. The solvent circulation path was programmed to circulate the solvent back to the solvent tank through the top of the extraction vessel. After half an hour of extraction, the circulation direction of the solvent was changed from bottom of the extraction vessel to the top of the extractor vessel (counter current). The direction of solvent flow was programmed to alternate in opposite directions every half-hour (30min) for six hours (6hr) to create a countercurrent flow of the solvent. At the end of the six hours (6hr), the extract was passed through nine (9) layers of a Seitz® K700 filter from Pall Corporation (Port Washington, NY, USA) and collected in a concentration tank.
[0524] The solvent in the extract was evaporated in two-stages. In the first stage, the extract was evaporated using a plate evaporator (Samtech Extraktionstechnik GmbH, Jagerzeile 34, Mannersdorf, Austria 2452) for 2 hours to recover about 40% solvent (the parameters for plate evaporator were - vacuum: -800 mbar at 60°C). In the second stage, the extract was further concentrated with a thin film evaporator (Samtech
Extraktionstechnik GmbH, Jagerzeile 34, Mannersdorf, Austria 2452) to recover 80% of the solvent (the parameters for plate evaporator were - vacuum -800 mbar at 60°C). At the end of the concentration process, the initial 800 liters of solvent was reduced to 100 litres of solvent containing extract.
[0525] The remaining 100 liters of solvent is removed and the extract converted to a powder using a spray drier. The spray dryer used was a Labultima LU288 spray dryer (Labultima Process Technology Pvt. Ltd., Maharashtra, India) with the following operating parameters: an air pressure of 1.4 bar, inlet temperature: 150 °C, outlet temperature: 130 °C, inlet high temperature: 200 °C, outlet high temperature: 180 °C, cool temp temperature: 100 °C, ID blower: 400 units, FD blower: 200 units, Feed pump speed: 30 ml/min, D Block: 1, Nozzle Pressure: 60 bar, Cycle: 999, and Vacuum: -400 mbar. The powder thus formed has a consistent particle size distribution and can be further processed for chemical analysis or used in the manufacture of formulations for the treatment of a variety of physiological disorders.
Example 2. HPLC Analysis of an Extract of O. stamineus Leaves Manufactured as Described in
Example 1
[0526] Standardization and quantification of the dominant biomarker compounds in an extract of O. stamineus leaves manufactured as described in Example 1 was determined using HPLC.
[0527] Standard markers were included for A, SIN, EUP, and TMF. Stock solutions of standard marker compounds RA, SIN, EUP and TM F were prepared by dissolving 1 mg of
each marker in 1 mL of HPLC-grade methanol to water at a ratio of 1:1 (vol/vol) and filtered through a 0.45 μιη Whatman® filter paper. Working marker solutions were diluted with HPLC-grade methanol to water at a ratio of 1:1 (vol/vol) in serial concentrations range from 0.195-100μg/mL to prepare working standard solutions.
[0528] The extract was prepared for HPLC analysis by dissolving the dried powder at 10 mg/mL in a mixture of HPLC-grade methanol to water (1:1) for HPLC use. The stock solution was sonicated for 30 min and filtered using 0.45μιη syringe filters and transferred into an HPLC vial.
[0529] Reverse-phased HPLC was performed using a Dionex-Ultimate®3000 Rapid Separation LC system (Thermo Fisher Scientific Inc., USA), equipped with a degasser, an autosampler, a column heater, quaternary pump and a diode array detector (DAD) detector. Chromatographic separation was performed using a reverse phase Acclaim Polar Advantage II C18 column as described by Saidan et al. (264). The column (150 mm x 3 mm, 3μιη) was maintained at 40°C. The mobile phase consisted of 0.1% formic acid solution (A) and acetonitrile (B) with gradient elution system as shown in Table 1 at a flow rate of 1 mL/min, separation time 18 min and the injection volume was 5μί. The detection wavelength was performed at 320 nm. The peak identification was based on the retention time and the DAD spectrum against the standards presented in the chromatogram. Data collection and integration was performed by Chromeleon® software version 6.8 (Dionex, Thermo Fisher Scientific Inc.). Four standard reference compounds were used as bioactive markers namely EUP, RA, TMF, and SIN. Standard calibration curves were established by plotting the peak areas against different concentrations. The peak of reference standard was identified by comparison of their retention time values and spiked with the samples. The external standard method was used for quantification of the bioactive markers in the extract sample. The amount of RA in the extract was quantified and fixed throughout the work.
Table 1. HPLC mobile phase gradient elution program for the standards and an extract of O. stamineus leaves manufactured as described in Example 1
[0530] Linearity was evaluated by injecting 5 μί of the standard mixture in 10 serial concentrations ranges from 1.95-250 μg/mL. The calibration curve was obtained by plotting the concentration curves against peak area for each compound. The correlation coefficients (R
2) of each compound was determined by applying the linear regression equation of the calibration graphs in Excel
®.
[0531] Selectivity was determined by comparing the retention time of the compounds obtained in the sample extracts with those of the known reference compounds.
[0532] 5μί of the extract prepared for HPLC analysis was injected at 1 mg/mL and the peak area corresponding to target compounds EUP, SIN, A and TM F were recorded. The linear regression equations of the standard calibration curves were applied to calculate the concentration of the marker compounds in the samples. The content of the marker compounds was presented as average percentage (% w/w) of the dried extract by using the following equation:
Average percentage (wt/wt) = (used concentration /1000 μg/mL) x 100.
[0533] Results of the HPLC analysis are presented in Table 2 as mean ± SD, (n=3). The HPLC chemical fingerprint of the standards and of an extract of O. stamineus leaves manufactured as described in Example 1 is shown in Fig. 1A and IB respectively. Table 2 also shows the results of a different batch of O. stamineus leaves extracted as described in Example 1. For comparative purposes, the data for the prior art macerated extracts was reproduced from Shafaei et al. (123).
Table 2. Quantification of four marker compounds in an extract of O. stamineus leaves manufactured as described in Example 1 compared to that of macerated extracts reproduced from Shafaei et al. (123). Results are shown as % compound (wt/wt) of the extract. (ND: Not detected at 320 nm absorbance)
Example 3. Phytochemical Analysis of an Extract of O. stamineus Leaves Manufactured as
Described in Example 1
[0534] The extract of O. stamineus leaves manufactured as described in Example 1 was analyzed for phytochemical content by methods well known in the art. The class of phytochemicals analyzed included total polysaccharides, glycosaponins, phenolics, flavonoids, phospholipids, and protein content.
A. Determination of total soluble polysaccharide content.
[0535] Soluble polysaccharide content was determined as described by Siddiqui et al. (265). 0.2g of the extract was added to a centrifuge tube and the extract dissolved with 7 ml hot EtOH (80%) just to remove sugars. The sample tube was vortexed for 2 minutes and then centrifuged at 2700 rpm for 10 minutes. This process is repeated until washing of residue showed no color with anthrone reagent. The residue was then dried on a water bath and extracted with each 5 ml of water and 25% HCI at 0°C for 25minutes. Sample tube was centrifuged at 2700 rpm for 10 minutes and the supernatant was collected in a 100ml volumetric flask. The extraction is repeated with 10 ml 25% HCI and the supernatant collected into the same 100 ml volumetric flask. The total volume is made it up to 100 ml with distilled water. 100 μΙ of supernatant is pipetted into a test tube and the volume made
up to 1 ml with distilled water. To it was added 4ml of anthrone reagent and the test tube heated for 8 minutes in a boiling water bath. Sample tubes were cooled rapidly while keeping on ice and the intensity of green color was measured at 630 nm against a blank having all the reagents; except sample. Reference standard solutions of glucose were prepared from 20, 40, 60, 100 and 200 μg/ml and treated in the same way. All samples and standards were prepared in triplicates. Concentration of glucose was calculated from the linear regression equation obtained from the standard curve. Starch content was calculated by multiplying the glucose contents obtained from standard curve with a factor of 0.9.
B. Determination of total soluble glycosaponin content.
[0536] Total soluble glycosaponin content was determined as described by Siddiqui et al. (265). One gram of the extract was dissolved in 50 ml methanol, refluxed for 30 min and then filtered. This process was repeated twice. Filtrate was concentrated to 10 ml using rotary evaporator and the glycosaponins precipitated by adding extract dropwise to 50 ml acetone in a tarred beaker. Precipitate was dried in oven at 100°C to constant weight and glycosaponins calculated using the following formula:
Glycosaponins = (Weight of precipitate / Weight of sample) X 100.
C. Determination of total soluble phenolic content.
[0537] Total soluble phenolic content was determined using the Folin-Ciocalteu reagent as previously described with some modifications (266) (267). Gallic acid was used as standard and 4 mg/mL of the extract 1 was used. Different concentrations of gallic acid (0.313, 0.625, 0 1.25, 0 2.5, 5 and 10 mg/mL) in 80% methanol were prepared. 20 μΙ of sample solution and each concentration of gallic acid solutions were pipetted in separate test tubes followed by addition of 1.58 mL of distilled water and 100 μΙ of 2N Folin-Ciocalteu reagent. The test tubes were mixed thoroughly and incubated for 3 min. Subsequently, 300 μΙ of 20% Na2C03 solution was added and vortexed. The mixture was allowed to stand at room temperature for 2 h. Absorbance was measured at 765 nm using Hitachi U-2000 spectrophotometer (Hitachi, Japan). All determinations were carried out in triplicate. The concentration of total phenolic compounds in the extract was determined and expressed as microgram of gallic acid equivalent per g. The data is presented as the mean ± SD, (n=3).
D. Determination of total soluble flavonoid content.
[0538] Total flavonoid content was determined as previously described (268) (269) (270). Aluminum chloride colorimetric method (AICI3) was used to determine the total flavonoid contents of the extracts. Quercetin was used as positive control. A solution of 2 mg/mL of the extract of Example 1 in methanol and different concentrations of quercetin (0.625, 1.25, 2.5, 5, and 10 mg/mL) in 80% methanol HPLC grade were prepared. 0.5 mL of the extracts and quercetin followed by 0.1 mL of 10% (w/v) aluminum chloride, 100 μί of 1 M potassium acetate and 1.5 mL of methanol was pipetted into separate test tubes.
Subsequently, 2.8 mL of distilled water was added to all samples. Test tubes were mixed and incubated at room temperature for 30 min. All the samples and standards were prepared in triplicates and the absorbance of the reaction mixture was measured at 415 nm with a
Hitachi U-2000 spectrophotometer (Hitachi, Japan) against blank. The amount of 10% (w/v) aluminum chloride was substituted by the same amount of distilled water in a blank.
Quercetin (3.9-250 μg/mL) in methanol was used as standard. The concentration of total flavonoid contents in the extract was expressed and determined as micrograms of quercetin equivalent by using an equation that was obtained from the standard curve equation
(Υ=0.0062χ+0.0488). The data is represented as the mean ±SD, (n=3).
E. Determination of total soluble phospholipid content.
[0539] This assay is based on the formation of a complex between phospholipids and ammonium ferrothiocyanate (271). The reagent was prepared by dissolving 27 g of ferric chloride (FeCU 6H2O) and 30 g of ammonium thiocyanate (N H4SCN) in 1 liter of water.
Phosphatidylcholine in chloroform (1 mg/ml) was used as a reference standard. About 1 mg of the extract of Example 1 was dissolved in 2 ml of chloroform and 1 ml of thiocyanate reagent was added. The contents were vortexed for 1 min and centrifuged at low speed (1000 rpm) for 10 min. The red lower layer of chloroform was removed with a Pasteur pipette, after which, the remaining solution was read at an absorbance of 488 nm optical density (OD). The percentage of phospholipids in the extract was calculated using the regression equation obtained using the calibration curve of the standard phospholipid solution plotted with a different range of concentrations (10-100 μg).
F. Determination of total soluble protein (including free amino acid) content.
[0540] Total soluble protein was quantified as described by Lowry et. al. (272). Fifty milligrams of the extract of Example 1 was mixed with 10 ml distilled water in a centrifuge tube and vortexed for two minutes. The tube was further centrifuged for 10 min at 2700rpm. Supernatant was used for analysis. 0.05 ml of the supernatant was pipetted out into a test tube and made it up to 1 ml with distilled water. 3 ml of reagent C, prepared by mixing 50 ml of reagent A (2% sodium carbonate in 0.1N sodium hydroxide) and 1 ml of reagent B (0.5% copper sulphate in 1% potassium sodium tartrate) was then added to the tube. 0.2 ml of Folin-Ciocalteu reagent was further added to the tube and incubated for 30 min at room temperature. Bovine Serum Albumin (Fraction V) was used as a reference standard in a range of 10-250 ug/ml. All the samples and standards were prepared in triplicates and absorbance was measured at 600 nm against a blank having all the reagents except the sample. Total proteins were calculated from linear regression equation, obtained from the standard curve. The typical phytochemical content of an extract of O. stamineus leaves manufactured as described in Example 1 is presented in Table 3. Table 3: Phytochemical content in an extract of O. stamineus leaves manufactured as described in Example 1.
Example 4. Effect of an Extract of O. stamineus Leaves Manufactured as Described in
Example 1 on Sprouting of Microvessels from Rat Aortic Explants
[0541] The effectiveness of an extract of O. stamineus leaves manufactured as described in Example 1 on sprouting new blood microvessels at various concentrations was first compared to that of extracts prepared by maceration using water, 100% methanol, 50% methanol, 100% EtOH, 50% EtOH, RA and a suramin (positive control). The macerated
extracts were prepared as described in Shafaei et al. (123). This was then followed with the evaluation of the effectiveness of five different concentrations of an extract of O. stamineus leaves manufactured as described in Example 1. The rat aorta tissue explants were prepared as described by Brown et al. (273).
[0542] Eight to twelve-week old Sprague Dawley male rats were obtained from the animal house facility of the Universiti Sains Malaysia (USM) and were kept for one week in the transit animal unit at the School of Pharmaceutical Sciences of USM to acclimatize to the new environment. The rats were kept in ventilated cages on 12/12 h light/dark cycle at room temperature of 24 ± 2°C and a humidity of 60% with food and water provided all the time. Experimental work was done according to the guidelines of USM Animal Ethics Committee.
[0543] The animals were sacrificed via cervical dislocation under anesthesia with CO2. A midline inscision was made into the abdominal and thoracic cavities including splitting of the sternum. Thoracic aortas were excised, rinsed with serum free media, removed of fibro- adipose tissue and cross sectioned into thin rings approximately 1 mm in thickness.
[0544] Two layers of the M199 culture medium were prepared for the aortic ring assay. The lower layer (solidified layer) was prepared from serum free M199 supplemented with fibrinogen and aprotinin at 3 mg/mL and 5 μg/mL, respectively. 300 μί of this mixture was then applied in each well of a 48-well plate. Aortic ring sections were then placed in each well. 10 μΐ of thrombin, prepared at 50 NIH U/mL in 0.15 M NaCI in 1% bovine serum albumin was added to each well and allowed to solidify at 37°C in 5% CO2 for 90 min. The top liquid layer culture medium was prepared by adding the following to M199 basal medium: fetal bovine serum (FBS) at 20% v/v, L-glutamine at 1%, aminocaproic acid at 0.1%, amphotericin B at 1% and gentamicin at 0.6%. Initially, the extract O. stamineus leaves manufactured as described in Example 1, was screened at 100μg/mL, in comparison with the extracts obtained by maceration described by Shafaei et al. (123).
[0545] The IC50 value for the extract of O. stamineus leaves manufactured as described in Example 1 was determined for using serial concentrations (6.25 - 100 μg/mL) and incubated at 37°C, 5% CO2 in a humidified incubator. On day four, the top liquid layer culture medium was discarded and changed with fresh medium prepared as previously mentioned with the extract. Media was used as a negative control in all experiments. The work was done in a biosafety cabinet (Class II) (ESCO, Singapore).
[0546] The magnitude of blood vessel outgrowth from the rat aortic rings was quantified as described by Nicosia et. al. (274). Briefly, the distance of blood vessels outgrowing from the rat aorta tissue explant was measured on day five under the 20x magnification power of inverted light microscope supplied with Leica Quin computerized imaging system. The growth distance of at least twenty blood vessels per ring was measured. Blood vessels were selected at regular intervals around the rings to reduce bias. The experiment was performed in triplicate (each replicate containing six rings) and the results presented as a mean ± SD, (n=3). The inhibition of blood vessel formation was calculated using the formula:
% inhibition = (1- (A0/Ai)) x 100
[0547] where, Ao= distance of blood vessel growth in treated rings with the prior art macerated extracts or the extract of O. stamineus leaves as manufactured in Example 1 in μιη, and Ai=distance of blood vessel growth in the control in μιη.
[0548] Prior art macerated extracts were prepared as described by Shafaei et al. (123).
[0549] The effectiveness of the various solvent macerated extracts of O. stamineus leaves versus an extract of O. stamineus leaves manufactured as described in Example 1 on blood vessel outgrowth from rat aorta tissue explants is shown in Table 4.
Table 4. Effect of various solvent macerated extracts of O. stamineus leaves vs. an extract of O. stamineus leaves manufactured as described in Example 1 on inhibition of neovascularization. Values are expressed as % inhibition of blood vessel neovascularization compared to negative control ± SD. n=3, *p < 0.001 compared to negative control
[0550] Table 5 shows the effect of increasing concentrations of an extract of O.
stamineus leaves manufactured as described in Example 1, A, and Suramin in μg/ml on sprouting of new microvessels from preexisting blood vessels such as the rat aorta tissue explants used in this experiment.
Table 5. Effect of Various Concentrations of an Extract of O. stamineus Leaves Manufactured as Described in Example 1 (E) and RA on Inhibition of Neovascularization relative to negative control. Suramin (S) was used as a positive control. Values are presented as ± SD, n=5, *p < 0.05.
[0551] The data from Table 5 was used to generate the following regression curve for the % inhibition of neovascularization by the extract of O. stamineus leaves manufactured as described in Example 1:
Y = 25.39ln(x) - 23.61, r2 = 0.989
[0552] where y = % inhibition of neovascularization, and x = concentration of the extract according to Example 1.
[0553] Similarly, the data from Table 5 was used to generate the following regression curve for the % inhibition of neovascularization by RA:
Y = 19.13ln(x) + 6.363, r2 = 0.990
[0554] where y = % inhibition of neovascularization, and x = concentration of RA.
Example 5. Effect of an Extract of O. stamineus Leaves Manufactured as Described in
Example 1 on Proliferation of HUVECs.
[0555] Angiogenesis involves local proliferation of endothelial cells in response to an angiogenic stimulus. This example illustrates the effectiveness of an extract of O. stamineus leaves manufactured as described in Example 1 and pure RA in inhibiting endothelial cell and cancer cell proliferation.
[0556] The effect of the extract on HUVEC cell proliferation was investigated using the MTT assay as described previously (275). HUVECs (ScienCell Research Laboratories, USA. Catalog # 8000) were maintained in ECM supplemented with 5% FBS, 1% PS and 1% ECGS. The cells were seeded in 96-well plates at a density of 2xl04 cells/well in ΙΟΟμί growth media and kept overnight to facilitate attachment. The cells were exposed to the extract (E) and RA (3.625 tolOO μg/mL) for 48 h. After incubation, the viability of HUVECs was assessed by the MTT assay (276). 20 μΐ of MTT solution (5 mg/mL in PBS) was added to each well. After 4 h incubation, the mixed media and the MTT solution was carefully discarded and the crystallized dye solubilized with DMSO. Vincristine was used as the reference standard. The amount of blue dye formed was determined by measuring the absorbance at 570 nm.
[0557] The effect of various concentrations of an extract of O. stamineus leaves manufactured as described in Example 1 (E) and RA on the proliferation of HUVECs is shown in Table 6.
Table 6. Effect of an extract of O. stamineus leaves manufactured as described in Example 1 (E) and RA on the proliferation of HUVECS.
[0558] A dose response curve of the effect of the extract based on the data in Table 6 was used to generate the following equation:
y = 14.05ln(x) - 18.28, r2 = 0.982
[0559] where y = % inhibition of HUVEC proliferation, and x = concentration of the extract. The IC5o for the extract is 129 μg/ml.
[0560] A dose response curve of the effect of RA based on the data in Table 6 was used to generate the following equation:
y = 0.384x - 3.794, r2 = 0.975
[0561] where y = % inhibition of HUVEC proliferation, and x = concentration of RA. The ICso for RA is 141.6 μg/ml.
[0562] The standard reference (vincristine) exhibited a strong anti-proliferative effect, with an IC5o = 0.13 μg/mL.
Example 6. Effect of an Extract of O. stamineus Leaves Manufactured as Described in
Example 1 on Migration of HUVECs
[0563] Angiogenesis involves not just local proliferation of endothelial cells in response to an angiogenic stimulus, but also the migration of the endothelial cells to form the new capillary network. This example illustrates the effectiveness of an extract of O. stamineus leaves manufactured as described in Example 1 in inhibiting migration of endothelial and cancer cells.
[0564] The assay was carried out as described previously (277). HUVEC cells, were cultured as described in Example 3. For the migration assay, HUVECs were plated in 6-well plates till a 100% confluent monolayer was formed.
[0565] A wound was subsequently created in each well with a sterile 200μί micropipette tip. The detached cells were removed by gently washing twice with PBS and the plates were treated with the extract in a dose dependent manner. HUVECs were treated with vehicle and the extract of Example 1 at 12^g/ml (E-12.5) and 25μg/ml (E-25) and photographed at 0 and 12 h. Photographs were taken under an inverted light microscope supplied with Leica Quin computerized imaging system. About 8-10 fields per well were photographed and minimum of 20 readings per field were measured. The percentage of migration inhibition was calculated by the following equation:
% Migration inhibition = (1- (Ds / Dc)) χ 100 where, Ds = distance travelled by cells treated with the extract and Dc = Distance travelled by cells treated with vehicle. Percent inhibition of wound healing on HUVECs by the extract is shown in Table 7.
Table 7. Effect of an extract of O. stamineus leaves manufactured as described in Example 1 on wound healing on HUVECs 12 hours after creation of wound. Values are presented as % inhibition ± SD compared to negative control (vehicle), n = 5, * p < 0.001.
Example 7. Effect of an Extract of O. stamineus Leaves Manufactured as Described in
Example 1 on Invasiveness of Colorectal Cancer Cells
[0566] The effect of an extract of O. stamineus leaves manufactured as described in Example 1 on cancer cell invasion was determined on a human colorectal cancer (HCT-116) cell line.
[0567] The invasion assay was performed using Matrigel® matrix as previously described (278) with slight modification. Briefly, 50 μί of 10 mg/mL Matrigel® was diluted 1:1 in culture medium and coated onto each well of a 96-well plate and allowed to solidify for 45 min.
[0568] HCT-116 cells were used at passage number below 7 and maintained in PMI 1640 medium (GIBCO, Thermo Fisher Scientific Inc., USA) supplemented with 10% FBS and 1% P/S solution. 25 μg/mL (E-25) or 50 μg/mL (E-50) of the extract, 25 μg/ml of RA (RA-25) or vehicle was added to 5 X 103 cells in 150 μί RPMI medium were added prior to seeding each well to each well and incubated at 37°C, 5% CO2 in a humidified incubator for 48 h. Some of the cells were seeded in DMEM and vehicle only as the negative control. Plates were kept in a humidified incubator at 37°C and 5% CO2 for a further 24 h.
[0569] Subsequently, the upper media were aspirated carefully and the wells were washed twice with lx PBS to remove the non-invaded cells with extreme care to prevent disruption of the Matrigel layer. Finally, the wells were captured at 4x magnification using an inverted microscope connected to a digital imaging system. The cells that had migrated through the Matrigel® were photographed and counted after staining by calcein AM fluorescent dye.
[0570] Quantification of invasion data was performed by counting the number of the invaded cells in the treated wells with comparison to that of the untreated wells (negative control). The results were presented as percentage of inhibition of invasion in relation to the negative control and was calculated as follows:
% inhibition of invasion = (l-(no. of invaded cellsjs) /no. of invaded cellS(Nq)) x 100 where, S = treated wells with samples and NC = untreated wells (negative control).
[0571] All samples were run in triplicate and the results are presented as mean percentage of invasion inhibition relative to the negative control. Results are shown in Table 8.
Table 8. Effect of RA and an extract of O. stamineus leaves manufactured as described in Example 1 on cell Invasion of human colorectal cancer cells relative to untreated cells. Values are presented as % inhibition ± SD. n=3, *p < 0.001.
Example 8. Effect of an Extract of O. stamineus Leaves Manufactured as Described in
Example 1 on HUVEC Capillary-Like Tube Formation
[0572] This example illustrates the ability of the extract of O. stamineus leaves manufactured as described in Example 1 to inhibit formation of capillary-like tubes by endothelial cells. The formation of capillary-like tubes was performed on a Matrigel® matrix as previously described (49).
[0573] Confluent culture flasks with HUVECs were (a) left untreated, (b) treated with the extract of Example 1 at 2.5 μg/mL (E-2.5), (c) treated with the extract of Example 1 at 25 μg/mL (E-25), (d) treated with RA at 10 μg/mL (RA-10), and (e) treated with suramin at 10 μg/mL (S-10) for 24 h. The Matrigel® matrix stock (10 mg/mL) was diluted with cold serum- free endothelial cell medium (1:1) and a 150μί of the diluted Matrigel® mixture was coated onto 48-well plates and allowed to polymerize for 45 min at 37°C and 5% CO2. Subsequently, the endothelial cells were trypsinized and seeded (2 xlO5 cells per well) in 500μί of endothelial cell medium containing the various concentrations of the extract of Example 1 in triplicate. After 6 h, any capillary-like tubular structures formed were imaged under the inverted light microscope at 20X magnification. The quantitative assessment of capillary-like tube formation inhibition was performed by measuring the area occupied by capillary-like tubular structures as described by Bandyopadhyay using the Scion Image analysis program (Scion Corporation) (279). Results are presented as a mean percentage inhibition ± SD, (n=3). The percent inhibition was calculated using the following formula:
% Capillary-like Tube formation inhibition = (1- (AT/ AC)) χ 100 where, AT = Area of capillary-like tubes formed in treated wells with the extract and AC =
Area of capillary-like tubes formed in wells treated with the control.
[0574] The effect of increasing concentrations of the extract, RA, and suramin on capillary-like tube formation compared to negative control is shown in Table 9. Table 9. Effect of RA and an extract of O. stamineus leaves manufactured as described in Example 1 on capillary-like tube formation relative to untreated cells. Values are presented as % inhibition compared to negative control ± SD. n = 3, *p < 0.01, **p < 0.001.
Example 9. Effect of an Extract of O. stamineus Leaves Manufactured as Described in
Example 1 on Neovascularization in CAM
[0575] The ability of an extract of O. stamineus leaves manufactured as described in Example 1 to inhibit neovascularization was evaluated using the CAM assay as described by West et al. and Ribatti (280) (281). Five-day old fertilized pathogen free eggs were used in the study. The eggs were sterilized by antiseptic solution (70% alcohol) and incubated at 37°C/60-70% humidity. Albumin (5-7 mL) was aspirated using a sterilized 18 G-needle syringe, the hole was covered with sterilized surgical tape to avoid the further albumin flow out of the egg and prevent contamination. The eggs were incubated overnight at 37°C/60- 70% humidity horizontally to allow the CAM to detach from the egg shell.
[0576] The extract was prepared in 1.2% agarose discs at two concentrations:
50μg/disc (E-50) and 100μg/disc (E-200). RA at 50μg/disc (RA-50) was used as a positive control. Discs containing the vehicle were used as negative control. Then, a small opening with 2-2.5cm in diameter on the broad pole was made in the shell and the discs were directly applied onto the CAM at the high density of blood vessels as described by Ozcetin et al. (282). The square opening was sealed with sterilized surgical tape and the embryo was incubated for 24 h. The CAM was photographed under a dissecting microscope (n=6). The results are shown in Table 10.
Table 10. Effect of RA and an Extract of O. stamineus Leaves Manufactured as Described in Example 1 on Neovascularization In-Vivo in Chick Embryo Chorioallantoic Membrane (CAM). Values are presented as ± SD. n = 5, ***p < 0.001 compared to vehicle.
Example 10. Effect of an Extract of O. stamineus Leaves Manufactured as Described in Example 1 on Aggregation of Human Colorectal Cancer Cells to Form Solid Tumors
[0577] MCTS were generated from HCT-116 (ATCC, Rockville, USA) in hanging droplets as previously described (283) with minor modifications. HCT-116 cells were cultured and maintained as described in Example 7. To establish HCT-116 spheroids, 1 x 104 cells were suspended in 1 mL of RPMI medium supplemented with 1% glucose, 1% of P/S and 10% of FBS. 20 μί drops were transferred onto the inner surface of a 150mm petri dish cover. To
ensure the integrity and prevent merging of droplets, the droplets were placed sufficiently apart on the dish cover. The cover was then placed over the bottom dish containing 20 mL of PBS to prevent dehydration of the droplets. Spheroids, once formed, (usually after 48-72h of culture), were transferred to a 48-well plate coated with 1% agar (for preventing spheroid attachment to the plate). After 2 hrs, each well was filled with 300μΙ media and an extract of O. stamineus leaves manufactured as described in of Example 1 at 100 μg/ml or 200 μg/ml, and RA or betulinic acid at 100μg/ml (n=6 for each treatment). Betulinic acid has been shown to inhibit colon cancer cell and tumor growth (284) and served as a positive control. Spheroids were photographed after staining by calcein AM fluorescent dye (BD Biosciences, CA). Effect of the treatments on the integrity of HCT-116 spheroid formation is shown in Fig. 2.
Example 11. Effect of an Extract of O. stamineus Leaves Manufactured as Described in Example 1, RA, and Imatinib on Short-Term (28-days) Xenograft Ectopic Model Human
Colorectal Tumor Growth in Nude Mice.
[0578] Thirty-five athymic NCR nu/nu nude mice aged 4-6 weeks with a weight of 23 ± 2 g were obtained from Taconic Farms Inc., USA. Specific pathogen free cages, each with high efficiency particulate air filter, using animal transport unit (Allentown, USA) were used to house the mice. Sterile food, water and bedding were provided and mice were housed under a standardized 12/12 h light/dark cycle at a room temperature of 24 ± 2°C and a humidity of 60%. Sterile bedding was changed twice a week. All in-vivo studies were conducted according to ethical guidelines and were approved by the ethical committee of Universiti Sains Malaysia.
[0579] HCT-116 cells were selected as a model for colorectal cancer (285). The cells were used at passage number below 7 and were maintained in RPMI 1640 medium with 10% FBS and 1% P/S solution. Seventy percent confluent cultures in T75 flasks were trypsinized and resuspended in 5 mL of fresh medium, the cells were collected by centrifugation at 1000 rpm for 5 min and washed with a sterile PBS in order to remove the trypsin.
[0580] The cell pellet was re-suspended in 200 μί of complete RPMI culture medium supplemented with 10% FBS and 1% penicillin/streptomycin solution and kept on ice.
Animals were injected subcutaneously in the right flank with 5 xlO6 cells in 200 μί culture medium using a ImL syringe attached to a 25-Gauge needle. The injection site was inspected for 30sec with a sterile cotton swab to prevent leakage of cells before the animals were returned to their respective cages.
[0581] When the average tumor size reached approximately 100 mm3 (6 days post cell inoculation), animals with uniform tumor size were randomly divided into six groups (5- 6/group). Group 1 received 0.1 mL distilled water orally (negative control), Group 2 was treated with imatinib at 30 mg/kg (1-30), Group 3 was treated with RA at 30 mg/kg (RA-30), Group 4 was treated with lOOmg/kg of an extract of O. stamineus leaves manufactured as described in Example 1 (E-100), Group 5 was treated with 200 mg/kg of the extract (E-200) and finally, Group 6 was treated with 400 mg/kg of the extract (E-400). Treatments were administered once daily for a period of 28 days. Treatments were administered orally by oral gavage using 20-gauge needle. % inhibition of tumor growth was calculated as described by Deng et al. (286) as follows:
Percentage inhibition of tumour growth = (1 - (ΔΤ/AC)) x 100
where, ΔΤ = Τ28-Δ0 and AC = C28-Ao
Δο = the average of tumour volume at the beginning of the treatment (day 0).
T28 = the average tumour volume at the day 28 for the treated groups.
C28 = the average tumour volume at the day 28 for the negative control group.
[0582] Tumor volume (mm3) was determined with the aid of a digital calliper (287) by applying the following equation:
Tumor volume (mm3) = (LxWxD)/2
where, L is the length (mm), W is the width (mm) and D is the depth of the tumor (mm).
[0583] Tumor volume and body weight measurements were recorded at every seven- day interval until the end of the experiment. At the end of experiment, animals were euthanized by CO2 followed by cervical dislocation.
[0584] The xenograft tumors were harvested and the tumors were cut in two parts. One half was immediately placed on ice cold Procarta® lysis buffer (Affymetrix, Santa Clara, CA) and homogenized in a homogenizer until there were no clumps. The samples were centrifuged at 14,000 rpm for 10 min at 4°C, and the supernatant was transferred to a new tube and stored at -80°C for further use. The other half was preserved in 4%
paraformaldehyde for histopathology work and examined for vascularization, tissue morphology and necrosis/apoptosis. The results of the effect of the various treatments on tumor volume and inhibition of tumor growth are shown in Table 11. The change in weight of the animals over the treatment period is shown in Table 12.
Table 11. Effect of an Extract of O. stamineus Leaves Manufactured as Described in Example 1, RA, and Imatinib on Tumor Volume (mm3) and Percent Inhibition of Tumor Size (relative to vehicle at Day 28) in Response the Various Treatments in a Short-Term Study (28 days) on Tumor Size of Ectopic Xenografts of Human Colorectal Tumors in Nude Mice. Values are presented as ± SD. n = 6, ***p < 0.001 compared to vehicle.
Table 12. Effect of an Extract of O. stamineus Leaves Manufactured as Described in Example 1 and Imatinib on Weight Gain in Response to the Extract of O. stamineus Leaves, RA and Imatinib in a Short-Term Study (28 days) for Treatment of Ectopic Xenografts of Human Colorectal Tumors in Nude Mice. Values are presented as ± SD. n = 6, *p≥ 0.05.
Vehicle 25.7 ± 2.1 25.5 ± 2.3 25.2 ± 1.9 24.2 ± 1.6 24.3 ± 2
E-100 25.7 ± 2.1 25.4 ± 2.4 26 ± 2.4 25 ± 2.1 25 ± 2.4
E-200 29.7 ± 1.2 29.2 ± 1.4 28.8 ± 1.5 27.3 ± 1.4 27.0 ± 1.3
E-400 26.3 ± 0.7 26.2 ± 0.7 25.6 ± 1.3 24.3 ± 1.6 26.5 ± 1.3
RA-30 27.4 ± 2.4 27.3 ± 2.6 27.2 ± 2.7 26.1 ± 3.2 25.8 ± 3.6
1-30 28.4 ± 3.8 28.1 ± 4.1 27.0 ± 3.4 26.5 ± 3.2 27.1 ± 3.3
Example 12. Effect of an Extract of O. stamineus Leaves Manufactured as Described in Example 1, RA, and Imatinib on Survival of Long-Term (182-davs) Xenograft Ectopic Model
Human Colorectal Tumor Growth in Nude Mice
[0585] The purpose of this example was to investigate the survival rate of athymic nude mice bearing human HCT-116 colorectal xenograft ectopic tumors over a 26-week period (182 days) when treated at various doses of an extract of O. stamineus leaves manufactured as described in Example 1, RA and Imatinib.
[0586] The nude mice and HCT-116 cells were prepared and inoculated as described in Example 11. After day 6 post inoculation with 200 μί of 5 x 10s HCT-116 cells, animals were randomly divided into six groups of 10 animals each. The first group of mice was given 0.1 mL distilled water orally (negative control). Groups 2, 3, and 4 were treated with the extract. Group 2 was treated with 100 mg/kg/day of the extract (E-100), Group 3 was treated with 200 mg/kg/day of the extract (E-200), and Group 4 was treated with 400 mg/kg/day of the extract (E-400). Groups 5 and 6 were administrated with RA (RA-30) and imatinib (1-30) at a dose of 30 mg/kg respectively. Animal survival was observed daily up to 26 weeks. At the end of study, the animal survival rate was calculated by dividing the number of live animals by total number of animals. All negative control group animals were euthanized after four weeks when tumors reached more than 1000 mm3. At the end of experiment, the animals that survived were euthanized by CO2 followed by cervical dislocation. The results of the effect of the various treatments on long term survival are shown in Table 13.
Table 13. Effect of an extract of O. stamineus leaves manufactured as described in Example 1 (E), RA, and Imatinib (I) on long-term survival of xenograft ectopic model human colorectal tumor growth in nude mice.
Negative
Time control E-400 E-200 E-100 RA-30 1-30
1 10 10 10 10 10 10
1.999 10 10 10 10 10 10
2 10 10 10 10 10 10
2.999 10 10 10 10 10 10
3 10 10 10 10 10 10
3.999 10 10 10 10 10 10
4 10 10 10 10 10 10
4.999 10 10 10 10 10 10
5 0 10 10 10 10 10
5.999 0 10 10 10 10 10
6 0 10 10 10 10 10
6.999 0 10 10 10 10 10
7 0 10 10 10 10 10
7.999 0 10 10 10 10 10
8 0 10 10 10 10 8
8.999 0 10 10 10 10 8
9 0 9 9 6 5 5
9.999 0 9 9 6 5 5
10 0 8 9 5 5 5
10.999 0 8 9 5 5 5
11 0 8 9 4 5 4
11.999 0 8 9 4 5 4
12 0 8 9 4 5 4
12.999 0 8 9 4 5 4
13 0 7 8 2 5 3
13.999 0 7 8 2 5 3
14.998 0 7 8 2 5 3
15.997 0 7 8 2 5 3
15 0 7 7 2 4 2
15.999 0 7 7 2 4 2
16 0 6 7 2 4 2
16.999 0 6 7 2 4 2
17 0 6 7 2 4 2
17.999 0 6 7 2 4 2
18 0 6 7 2 4 2
18.999 0 6 7 2 4 2
19 0 6 7 2 4 2
19.999 0 6 7 2 4 2
20 0 5 7 1 4 2
20.999 0 5 7 1 4 2
21 0 5 6 1 4 2
21.999 0 5 6 1 4 2
22 0 5 6 1 2 2
22.999 0 5 6 1 2 2
23 0 5 6 1 2 2
23.999 0 5 6 1 2 2
24 0 5 6 1 2 2
24.999 0 5 6 1 2 2
25 0 5 6 1 2 2
25.999 0 5 6 1 2 2
26 0 5 6 1 2 2
26.999 0 5 6 1 2 2
Example 13. Effect of an Extract of O. stamineus Leaves Manufactured as Described in Example 1, A, and Imatinib on Orthotopic Xenograft Model Human Colorectal Tumor
Growth in Nude Mice for 35-davs.
[0587] The purpose of this example was to investigate the effect of an extract of O.
stamineus leaves manufactured as described in Example 1, on orthotopic xenografts of
colorectal tumor growth in athymic nude mice.
[0588] The mice and HCT-116 cells used in this example were prepared as described in Example 11. The HCT-116 colon cancer cell pellet was re-suspended in 150μΙ of complete PMI supplemented with 10% FBS, 1% P/S solution and L-Glutamine. Mice with an average weight of 23 ± 2g and aged 4 - 6 weeks were anesthetized using ketamine and xylazine with O.lmL/10 g body weight (1 mL from 100 mg/mL ketamine was mixed with 0.5 mL 20 mg/mL xylazine in 8.5 mL PBS and administered via intraperitoneal injection). After local sterilization by 70% alcohol and disinfection, a 1.5cm incision was made in the left lower quadrant abdominal cavity with sterilized surgical laboratory tools. The cecum was identified and carefully exteriorized. 5 χ 10s HCT-116 colon cancer cells were suspended in 150μί of culture medium and injected slowly into the cecal wall of each mouse using a lmL syringe attached to a 27-gauge needle. The needle was kept on the injection site for 30 sec prior to removal followed by gently pressure over the injection site for 30 sec with a sterile cotton swab to prevent leakage. The cecum was replaced into the abdominal cavity and the abdominal wall and skin was closed with 5-0 absorbable suture. Before the animals were returned to the cages, the animals were kept warm on a heating pad for 30 min. Postoperative status and wound healing were monitored and disinfection solution was applied every day for one week.
[0589] Forty animals were divided into six groups of six animals each then treated with the extract, RA or imatinib. Treatments were initiated six-days post cell inoculation once the incision wound was completely healed. Group A received 0.1 ml distilled water (negative control), Groups B, C and D received treatment with 100, 200 and 400 mg/kg body weight of the extract respectively (E-100, E-200 and E-400), and Group E and F received treatment with 30 mg/kg body weight of RA (RA-30) and imatinib (1-30), respectively. The treatments were administered by oral gavage once daily for a period of 35 days. Body weight was recorded every 7 days. Before the animals were sacrificed, the tumors were analyzed using three-dimensional FMT. Blood samples were taken from the tail vein for further analysis as described below. Tumors were harvested for histological analysis as described below.
[0590] Imaging of tumor-bearing mice was conducted using FMT 1500 Preclinical Imaging System (PerkinElmer, USA) with two fluorescent imaging agents, AngioSense® 750 as the vascular molecular agent and HypoxiSense® 680 as a marker of hypoxic tissue to assess both image quality and tumor fluorescence quantification (in pmol) under various imaging conditions, based on a near-infrared (NIR) fluorescence. AngioSense® 750
PerkinElmer, NEV10011, accumulates in tumor tissue, as a measurement of vascular permeability (288). HypoxiSense® 680 (PerkinElmer, USA), detects the tumor cell surface expression of CA9 protein, which expression is increased in a host of tumors. The intensity of HypoxiSense® 680 fluorescence is proportional to tumor size (289). Prior to imaging, mice were anesthetized via intraperitoneal administration of ketamine (100 mg/kg) and xylazine (20 mg/kg body weight). The mice were then injected intravenously into the tail vein of tumor bearing mice with 200 μί of a solution of 2 nmol each of HypoxiSense® and
AngioSense® 750. Imaging was conducted FMT on 24 h post-probe injection. Mice were kept warm on heating pads during recovery from anesthesia before they were returned to their respective cages.
[0591] FMT was performed as previously described (290). Briefly, FMT imaging was evaluated 24 h post-probe injection. Anesthetized mice were comfortably positioned in the
FMT animal imaging cassette. After the cassette was positioned in the FMT1500 imaging system, reflectance images and tomographic datasets were generated using near-infrared (NI R) laser light. Briefly, for optical tomographic imaging, a low power N IR laser diode trans- illuminated (i.e. the passing of light through the animal's body to be collected on the opposite side) the tumor region by scanning through numerous sites in and around the tumor. The signal was via a charge-coupled device (CCD) camera, which was placed on the opposite side of the imaged animal to collect the multiple trans-illumination images.
Appropriate optical filters allowed collection of both fluorescence and excitation datasets, and the multiple source detector fluorescence projections were normalized to the paired collection of laser excitation data.
[0592] Collected fluorescence data were automatically reconstructed by FMT system software (True Quant™ software) provided by the manufacturer (PerkinElmer,
excitation/emission; 745/785 nm) as three-dimensional (3D) fluorescence datasets showing signal within the flank tumors. To quantify this tumor fluorescence, a field enclosing the tumor was selected, and 3D regions of interest (ROI) were drawn around the tumors, and a threshold was applied identically to all animals that were equal to 20% of the mean tumor fluorescence for the vehicle-treated tumor group. The total amount of tumor fluorescence (in pmoles) was automatically calculated relative to internal standards generated with known concentrations of appropriate N IR dyes. The result of the FMT analysis is shown in Table 14.
Table 14. Shows the effect of an extract of O. stamineus leaves manufactured as described in Example 1, RA, and imatinib on tumor growth based on the intensity of fluorescence for detection of blood vessel density and CA9. Values are expressed as mean ± SD, n=3.
[0593] Histological analysis of tumors was carried out to evaluate necrosis, apoptosis and determine anti-angiogenic and anti-tumor effects of the treatments on all groups of mice. After fixation of the tissue by 4% paraformaldehyde, tumor cross sections were cut into 4 μιη sections on adhesive glass and stained by hematoxylin/eosin at Pantai Pathology Laboratories (Penang, Malaysia) and necrosis/apoptosis as well as vascularization and tissue morphology was assessed by a qualified pathologist. The hematoxylin/eosin staining of the cross sections of tumors treated with the various treatments is shown in Fig. 3.
[0594] Blood samples were collected and centrifuged immediately at 1500 rpm for ten min, and serum was collected. Biochemistry indexes were measured by automated Olympus 640 Biochemistry Analyzer (Olympus, Malaysia) performed at Gribbles Pathology (Penang, Malaysia). Total Protein, Albumin, Globulin, the Albumin/Globulin Ratio, total Bilirubin, GGT, ALP, ALT, AST, and CEA was measured and are shown in Table 15. Table 15. Biochemical parameters in blood of nude mice with orthotopic xenografts of colorectal tumors treated for 35-days with an extract of O. stamineus leaves manufactured as described in Example 1 (E), RA and imatinib (I). Data are represented as mean ± standard deviation, p value was calculated using independent t test by comparing between different groups (control group vs treated
group). *p≤ 0.05 is considered significant.
Example 14. In Vivo Assessment of the Preventive Effect of an Extract of O. stamineus Leaves Manufactured as Described in Example 1 against Ectopic Xenograft of Human Colorectal
Tumor Growth in Nude Mice.
[0595] The preventive effect of the extract of an extract of O. stamineus leaves manufactured as described in Example 1 on ectopic xenograft of human colorectal cancer cells (HCT-116) in NCR nu/nu nude mice was done following the same procedures as described in Example 11. This property of the extract was evaluated by pretreating the nude mice with different doses for two-weeks prior to implantation of human colon cancer cells. Eighteen animals were randomly distributed into three groups of 6 mice each. Group 1 received distilled water as negative control, Group 2 received 200 mg/kg body weight the extract of Example 1 (E-200), and Group 3 received 400 mg/kg body weight the extract (E- 400). Mice were treated once daily by gavage for 14 days prior to implantation of the colorectal cancer cells.
[0596] The HCT-116 colorectal cancer cells were prepared for implantation in the pre- treated mice as follows. Sub-confluent cultures of the HCT-116 (ATCC, Rockville, USA) colorectal carcinoma cell line at passage number five were maintained in RPM I medium with 10% FBS 1% P/S and harvested by trypsinization. 5 χ 10s cells in 200 μΐ RPMI medium were injected subcutaneously in the right flank of each nude mouse pre-treated with the extract. Tumor volume was measured weekly for 28-days as described in Example 11 and body weight was also recorded weekly. At the end of the 28-day observation period post- treatment, animals were photographed weighed and prior to being sacrificed and tumors subsequently harvested and preserved in 4% paraformaldehyde and prepared for histopathological study. The gross morphology of the tumors is shown in Fig. 4A - C. The effect of tumor growth in animals pre-treated with the extract and the weight of the animals over the 28-day period is shown in Tables 16 and 17 respectively. Cross-sections of the tumors stained with haematoxylin/eosin is shown in Fig. 5. Table 16. Effect of an extract of O. stamineus leaves manufactured as described in Example 1 (E) on the size of tumors excised from nude mice pre-treated for 14-days with the extract of Example 1 or vehicle and subsequently implanted with human colon cancer cells ectopically for 28 Days. Values are expressed as ± SD, n=6, *p < 0.01, **p < 0.001.
Tumor Volume (mm3)
Treatment
Day 7 Day 14 Day 21 Day 28
Negative Control (vehicle) 169 ± 36 363 ± 102 658 ± 136 974 ± 103
E-200 27 ± 0.0* 96 ± 46** 143 ± 74** 124 ± 97**
E-400 35 ± 0.0* 134 ± 74** 102 ± 83** 91 ± 63**
Table 17. Weight of animals pre-treated for 14-days with an Extract of O. stamineus leaves manufactured as described in Example 1 or vehicle and subsequently implanted with human colon cancer cells ectopically for 28-Days. Values are expressed as ± SD, n=6
stamineus Leaves Manufactured as Described in Example 1 on Human Lung Adenocarcinoma and Transformed Human Umbilical Vein Endothelial Cells.
[0597] The efficacy of an extract of O. stamineus leaves manufactured as described in Example 1 and liposomal formulations comprising the same were evaluated for their effect on human lung cancer cells in-vitro and in-vivo. In this experiment, the extract was formulated as a liposomal drug delivery system, and the effect of this liposomal drug delivery system compared to the effect of unformulated extract on human lung cancer cells.
[0598] Nano liposomes comprising the extract were prepared by thin lipid-film using soybean phospholipids as previously described by Aisha et al. (154) and Jiang et al. (291) with some modifications. Seven different nanoparticles formulations were prepared to develop the optimum ratio of (L-a-phosphatidylcholine : extract) (Sigma-Alderich, Germany), from soybean lecithin; where seven different ratios were used (0.25, 0.33, 0.5, 1, 2, 3 and 4 : 1) of phosphatidylcholine : extract as previously suggested by Jain et al. (292) and
EP0209037A1. The compositions of the seven formulations are shown in Table 18.
Table 18. Ratio of phosphatidylcholine to extract according to Example 1 (wt/wt) in seven different liposome formulations.
[0599] The seven formulations listed in Table 18 were tested to evaluate the entrapment efficiency of the extract.
[0600] Entrapment or encapsulation efficiency of the extract in NPC0.25, N PC0.33, N PC0.5, N PCi, NPC2, NPC3 and NPC4was evaluated using ultraviolet visible (UV-Vis)
spectrophotometry to estimate the entrapped concentration of the common biomarker RA as described by Aisha et al. (154). The nanoparticles were washed at the end of formulation twice with lx PBS (5-ml each time), then centrifuged at 15000 rpm for 20 min. Supernatant containing the free extract was collected and diluted with 10 ml PBS. Then, the free extract in the supernatant was measured. The extract solution was prepared in PBS for calculation of RA content. RA was prepared at six concentrations in PBS (1000, 500, 250, 125, 62.5 and 31.25 μg/ml). 100 μΙ of each concentration of the supernatants, extract and RA were pipetted into each well of a 96-well microplate (Nunclon TM, Denmark) in triplicate. 100 μΙ of lx PBS was used as a negative control (NC). Consequently, the absorbance was measured at a wavelength of 325 nm (as resulted from UV-Vis screening of RA in PBS (25 μg/ml) at 500-200 nm of UV region) using a microplate reader. The entrapment efficiency was calculated from the optical density (OD) as following:
ODsample = (Asample _ ANC)
[0601] Where: ODsampie = The optical density of supernatant, extract and rosmarinic acid, Asampie = The absorbance of supernatant, extract and rosmarinic acid, and ANc = The absorbance of wells containing PBS.
[0602] Then, the concentration of RA in the supernatant (free extract) is deducted from its content in the extract to find out the entrapped RA in the nanoparticles to calculate entrapment efficiency using the following equation:
% of entrapment efficiency = ((RAExtract - RASupernatant)/ RAExtract) x 100
[0603] Where: RAExtract = concentration of RA in the extract, and RAsupematant = concentration of RA in the supernatant. Results of the entrapment efficiency is shown in Table 19.
Table 19. Percentage entrapment efficiency of liposomes with varying phosphatidylcholine to extract according to Example 1 ratios shown in Table 18. Results are expressed as mean ± SD. n=3, *p<0.05.
[0604] The percentage entrapment efficiency proportionally increased with the increase of phosphatidylcholine to extract ratio until 1:1, where the percentage entrapment efficiency was 78.37±1.35 % for N PCi (P<0.05). N PC2, NPC3, and N PC4 showed a slight increase in the entrapment efficiency, but were not significantly higher than that of NPCi (p> 0.05).
[0605] Acordingly, NPCi was further developed into three types of liposomes, each comprising a different phospholipid content. N Pl comprised 500 mg of L-a- phosphatidylcholine, N P2 comprised 500 mg of L-a-phosphatidylcholine and 100 mg of cholesterol (Bio Basic, Canada), and N P3 500 mg of L-a-phosphatidylcholine, 100 mg of cholesterol and 50 mg of L-a-phosphatidyl-DL-glycerol sodium salt (Sigma-Alderich, USA), from egg yolk. The compositions of N Pl, N P2, and N P3 are summarized in Table 20.
Table 20. Phospholipid Composition of Three Liposomes NPl, NP2, and NP3. L-a-phosphatidylcholine (PC), cholesterol and L-a-phosphatidyl-DL-glycerol sodium salt (PG).
[0606] Each of the three liposome formulations NPl, N P2, and NP3 were
manufactured as follows. The lipid mixture for each formulation was transferred into a 250- ml round-bottomed flask containing a solvent mixture of 3.3 ml of chloroform and 1.7 ml of methanol ( iedel-de Haen, Germany). Subsequently, the flask was fixed to a rotary evaporator (Eyela, USA) at a temperature of 50°C and rotation speed of 60 rounds per minute (rpm) to allow the lipids to dissolve completely. The flask was then flushed with a low nitrogen flux through an inlet tap to allow nitrogen to go directly into the flask for 30 seconds. Next, the vacuum pump was turned on for 30 min at 340 hectopascal (hPa) until a dried thin lipid-film coated the internal walls of the flask. 500 mg of the extract was mixed with 5 ml of lx phosphate buffer saline (PBS) (Sigma-Aldrich, USA) at a pH of about 7.4 in a 50-ml beaker and purged with nitrogen gas using capillary tube. The extract was then poured into the 250-ml flask, mixed well, attached to a rotary evaporator and flushed with a low nitrogen flux for further 30 seconds. Then, a vacuum pump was turned on with a speed of 60 rpm for 30 min at room temperature to hydrate the thin film. The flask was then separated from the rotary evaporator, allowed to stand at room temperature for 2 hr to allow for complete swelling of the nanoparticles (liposomes). Finally, the un-entrapped extract i.e., the supernatant, was separated from the nanoparticles by cold centrifugation. The supernatant was collected into a 15-ml falcon tube and mixed with 5 ml of PBS, re- centrifuged at 15000 rpm for 20 min at 4°C.The supernatant was separated and collected in 50-ml falcon tube. Pellet was resuspended with 5 ml PBS and re-centrifuged at the same way. All supernatants were combined, diluted with 10 ml of PBS and kept at 4°C for further analysis. The pellet, comprising the liposomes, was dried using a freeze drier (Labconco, USA) for 48 h at a pressure of 0.1 mBar and stored at 4°C for further use.
[0607] Entrapment efficiency of the extract in N Pl, N P2, and N P3 was evaluated as described above. Table 21 shows the results of the entrapment efficiency of the extract in each of N Pl, NP2, and N P3.
Table 21. Percentage entrapment efficiency of an extract according to Example 1 by liposomes NPl, NP2, and NP3. Results are expressed as mean ± SD. n=3, *p<0.05.
No. Liposome % Entrapment Efficiency
1 NPl 78.8 ± 0.87
2 NP2 86.03 ± 2.45
3 NP3 90.99 ±2.31
[0608] Both NP2 and NP3 had significantly higher entrapment efficiencies compared to NPl (p<0.05). NP3 also had a higher entrapment efficiency compared to NP2, but was not statistically significant (p>0.05).
[0609] A, TMF, SIN and EUP were quantified in each of NPl, NP2, and NP3 using HPLC as described by Saidan et al. (264). The concentration of the marker compounds was calculated by applying the linear regression equations of the corresponding standard reference compounds, where the linear regression equations were Y=10.987X-101.6, Y=14.566X-123.87, Y=17.973X-151.24 and Y=7.592X-67.254 for the biomarkers RA, TMF, SIN and EUP, respectively as resulted from the corresponding calibration curves. Table 22 shows the results of the HPLC analysis of the four marker compounds comprising NPl, NP2, NP3, and the extract.
Table 22. Concentrations (%w/w) of the 4 marker compounds RA, TMF, SIN and EUP in the aqueous solutions of the unformulated extract (E) and the three liposomes NPl, NP2 and NP3. Results are expressed as mean ± SD, n = 3.
[0610] The in-vitro release and dissolution properties of the extract from the liposomes (NPl, NP2 and NP3) was performed using in vitro drug release assay using dialysis method as previously described by Avgoustakis et al. (293) with some modifications.
[0611] Dialysis tubes were purchased from SERVA Electrophoresis GmbH (Heidelberg, Germany), it is a cellulose membrane, which is treated chemically and physically to increase its resistance; it has molecular weight cut-off value of (12000-14000), with a pore diameter of 25A. Dialysis tubes were cut into bags 4.5 cm in length.
[0612] The dialysis bags were then immersed in 100 ml of (2 % sodium bicarbonate/1 mM EDTA) and boiled for 10 min, followed by further boiling in deionized distilled water for 10 min. Subsequently, the water was decanted, bags were submerged completely in 100 ml of 50% EtOH/lmM EDTA and stored at 4°C until use. The dialysis bags were then rinsed with deionized distilled water, filled with 4 ml of the release medium (PBS) containing 400 mg of the extract and suspensions of NPl, NP2, and NP3. Bags were hermetically sealed at both ends with dialysis clips (Pierce, Thermo Scientific, USA), followed by suspending them into a
dissolution compartment containing 100 ml of lx PBS at a pH of 7.4, and maintained at 37 ± 0.5°C with continuous stirring at 100 rpm using a magnetic stirrer. One ml aliquots of the samples were withdrawn from the incubation medium at pre-determined time intervals of (0, 5, 10, 15, 20 and 30 min, 1, 2, 3, 4, 6, 12, 18, 24, 30, 36, 42 and 48 h); which was immediately replaced with 1 mL of fresh PBS (pH 7.4) to maintain the dissolution conditions. Samples were analyzed spectrophotometrically (UV-Vis) at a wavelength of 325 nm to quantify the percentage of the cumulative concentration of RA in the dissolution
compartment of the samples at their individual time intervals in relation to the cumulative concentration of RA of the pure extract (E) at the end of the experiment (48 h). The concentration of RA in the samples was calculated using the regression equation of the standard calibration curve, by plotting the concentrations of the reference RA against the absorbance at 325 nm. The experiments were performed in triplicates, the results are expressed as a percentage of cumulative release (mean ± SD) (n = 3). % cumulative release was calculated as follows:
% cumulative release = (RASampie(t)/RAE(48 h))*100 where: RAsampie(t) = the concentration of RA at the dissolution compartment of the sample at the time interval (t), RAE(48 h) = the concentration of RA at the dissolution compartment of the extract at 48 h. The release kinetics of RA from NPl, NP2, NP3 and the extract is shown in Table 23. Table 23. Percentage cumulative release (%) of RA from the dialysis bags containing an unformulated extract of O. stamineus leaves manufatcured as Described in Example 1 (E) and the liposomes (NPl, NP2 and NP3) over 48hr at pH 7.4, 37°C. Concentration of RA was analyzed spectrophotometrically 325 nm. Results are presented as mean ± SD, n = 3. *p≤ 0.05 in comparison to the unformulated extract, E.
[0613] Anti-proliferation potential, using the MTT assay described in Example 5, of an unformulated extract of O. stamineus leaves, manufactured as described in Example 1 and the nano liposomes NPl, NP2 and NP3 towards A549, EA.hy926 and CCD-I8C0 cell lines was estimated using a single concentration of 200 μg/ml of the extract and the nanoparticles in
DM EM medium (100 μΙ/well). 100 μ§/ιηΙ of A was used as a positive control; while, as a negative control, cells received vehicle only (deionized distilled water (DDW)). Blank wells were pipetted with an equal amount of cell-free DM EM. The results of this experiment are shown in Table 24.
Table 24. Effect on Cell Viability of A549, EA.hy926 and CCD-I8C0 Cell Lines after 48 h treatment with 200 g/ml of an Extract of O. stamineus leaves, manufactured as described in Example 1 (E), 20u /ml nanoparticles NPl, NP2, NP3, and positive control (RA at lOu^g/ml). Results are presented as mean % Cell Viability ± SD (n = 3). *p≤ 0.05 compared to negative control (vehicle), a*p < 0.05 compared to the unformulated extract E.
[0614] Cytotoxicity of the unformulated extract, N Pl, NP2, and N P3, against A549 and EA.hy926 cells was tested at six concentrations ranging from 100-1000 μg/ml in 100 μΙ/well of DM EM medium. Half maximal inhibitory concentration (IC50) was calculated by plotting a regression curve of percentage cell viability versus sample concentrations using the data in Table 25 and 26 for A549 and EA.hy926 cells respectively. The IC50 values of the
unformulated extract (E), N Pl, N P2, and N P3 for A549 cells is 567.66 ± 35.39, 455.21 ± 61.63, 357.11 ± 66.13, and 296.05 ± 46.27 μ^ΓηΙ respectively. The IC50 values of the unformulated extract (E), N Pl, N P2 and NP3 for EA.hy926 cells is 443.51 ± 49.93, 349 ± 51.87, 220.35 ± 47.63, and 165.81 ± 59.65 μ^ΓηΙ respectively.
Table 25. Anti-Proliferative Activity of an Extract of O. stamineus leaves Manufactured as Described in Example 1 (E) and the Liposomes (NPl, NP2 and NP3) towards A549 cells. Percentage Cell Viability Obtained Using MTT assay. Values are mean ± SD of three independent experiments. *p≤ 0.05 in comparison to the negative control. a*p < 0.05 in comparison to the corresponding concentration of the unformulated extract (E).
Concentrations % Cell Viability of A549 Cells
(Mg/ml) E NPl NP2 NP3
100 91.25±5.57 82.74±4.68* 68.82±5.42* a* 63.52±0.27* a*
200 75.02±4.40* 67.28±7.02* 59.12±2.61*'a* 53.91±2.19*'a*
400 67.37±3.72* 53.56±2.29* 46.33±6.15*'a* 43.64±5.99*
600 52.29±2.92* 37.07±4.24* 36.30±3.84* a* 33.06±5.85* a*
800 29.21±1.90* 21.90±8.25* 17.50±5.32* 15.57±3.43*'a*
1000 11.40±0.83 7.92±3.13 6.63±3.12 5.57±2.11
Table 26. Anti-proliferative activity of an extract of O. stamineus leaves manufactured as described in Example 1 (E) and nano-liposomes NPl, NP2 and NP3 towards EA.hy926 cells. Percentage cell viability obtained using MTT assay. Values are mean ± SD of three independent experiments, p≤ 0.05 in comparison to the negative control. *p≤ 0.05 in comparison to the corresponding concentration of the unformulated extract (E).
[0615] The effect of N Pl, N P2, and N P3 on neovascularization was compared to an unformulated extract of O. stamineus leaves according to Example 1 and positive control A in rat aortic explants as described in Example 4. The IC5o for N Pl, N P2, and N P3 for inhibiting neovascularization compared the unformulated extract was calculated by plotting a regression curve of % inhibition of sprouting of new blood vessels from rat aortic rings versus sample concentrations using the data in Table 27. The IC5o values of the unformulated extract E, N Pl, NP2 and N P3, were 108.83 ± 9.21, 95.43 ± 12.24, 75.96 ± 11.94 and 64.37 ± 15.85 /vg/ml, respectively.
Table 27. Inhibitory effect of an extract of O. stamineus leaves manufactured as described in Example 1 (E) and nano-liposomes NPl, NP2, and NP3 on new blood vessels growth using rat aortic ring assay after 5 days of treatment. Percentage inhibition of neovascularization. Data are presented as mean ± SD of three independent experiments. *p≤ 0.05 in relation to the negative control. 3*p≤ 0.05 in relation to the unformulated extract E.
[0616] N P2 and NP3 showed the most potent anti-angiogenic effect compared to the unformulated extract E (p < 0.05), but the difference in anti-angiogenic activity between NP2 and N P3 was not statistically significantly different (p > 0.05). Accordingly, N P2 was deemed
the most optimum nano-liposome formulation and was used to further investigate the in- vitro and in-vivo antiangiogenic properties of NP2 as described below.
[0617] The aim of this experiment was to evaluate the potency of an unformulated extract of O. stamineus manufactured as described in Example 1 and said extract formulated as NP2 on cell division and colonization of A549 and EA.hy926 cells (294). Single-cell suspension of A549 lung cancer cells were cultured in DMEM culture medium at a density of 500 cells/ ml for seeding. 2 ml/well of the cell suspension was pipetted into a sterile 6-well plate (Coster Corning, USA), followed by incubating the plate in a humidified incubator at 37°C and 5% CO2 for 12 h. DMEM medium was carefully aspirated and replaced with fresh DMEM medium comprising either the extract or NP2 at concentrations of 50, 100 and 200 μg/ml. A at a concentration of 100 μg/ml was used as a positive control. As a negative control, cells were treated with vehicle only. Cells were treated for 48h, after which the medium was decanted and the wells washed with lx PBS. Subsequently, 2 ml/well of fresh DMEM medium was added and replenished every 3-4 days, with routine monitoring using an inverted microscope until sufficiently large colonies of at least 50 cells per colony were formed in the negative control (untreated) wells (i.e. after 10 days). The medium, at this point, was discarded and the wells rinsed with lx PBS. 4% para-formaldehyde was added to the wells to fix the colonies followed by staining with 0.2% of crystal violet (Sigma-Aldrich, USA). The wells were rinsed with water to remove excessive dye. Finally, colonies of more than 50 cells were counted under a dissecting microscope (Motic, Taiwan) and the wells were imaged using a digital camera. 500 cells/ml of EA.hy926 cell suspension (in DMEM culturing medium) was cultured in a 6-well plate (2 ml/well) followed by 12 h incubation. Subsequently, the old medium was replenished with fresh medium comprising the extract and NP2 at concentrations of 100 and 200 μg/ml. RA at 100 μg/ml was used as a positive control. Negative control cells were treated with vehicle. Cells were treated for 48hr after which the medium was decanted and the wells rinsed with lx PBS. Subsequently, 2 ml/well of fresh DMEM medium was added and replenished every 3-4 days, with routine monitoring using an inverted microscope until sufficiently large colonies of more than 20 cells were formed in the untreated cells (negative control), (i.e. 8 days) (295) (296) (297). Calculations were carried out using the following equations:
% Plating Efficiency (PE) = (no. of colonies in negative control / number of seeded cells) x
100
where, % PE is the ratio of the number of the grown colonies/well in the negative control to the number of the seeded cells/well. % PE for A549 cells was calculated as 42.05 ± 5.24%. % PE for EA.hy926 cells was calculated as 24.57%.
% SF = (number of colonies in treated wells / (number of seeded cells χ PE)) χ 100
[0618] The result of the effect of the unformulated extract and NP2 on colony formation by A549 and EA.hy926 cells is shown in Table 28. Table 28. Effect of various concentrations of an extract of O. stamineus leaves manufactured as described in Example 1, said extract formulated as NP2, and RA on lung cancer cells (A549) and transformed human umbilical vein endothelial cells (EA.hy926) on colony formation. Values are expressed as ± SD n = 3, *p < 0.05, **p<0.01 compared to negative control.
Negative Control 100 100
Extract according to Example 1
50ng/ml 75.86 ± 7.22* - lOC^g/ml 43.10 ± 3.49** 82.85 ± 4.13*
200μg/ml 21.74 ± 1.91** 57.58 ± 2.26**
NP2
50μg/ml 54.43 ± 5.76** - lOC^g/ml 30.52 ± 2.3** 74.65 ± 2.31*
200μg/ml 7.89 ± 2.31** 31.72 ± 4.20**
RA
100μg/ml 1.07 ± 0.96** 1.32 ± 1.23**
[0619] This example illustrates the effectiveness of an unformulated extract of O. stamineus leaves manufactured as described in Example 1 and said extract formulated as NP2 in inhibiting migration of endothelial and cancer cells. This experiment was carried out essentially as described in Example 6. 2ml/well of A549 cells cultured in DMEM was pipetted into each well of a 6-well plate at a cell density of 2xl05 cells/ ml. Cells were incubated for 48hr in a humidified incubator supplied with 5% CO2 at 37°C to achieve a confluent monolayer of cells. EA.hy926 cells were similarly seeded and cultured in DM EM culture medium. A wound was subsequently created in each well with a sterile 200μί micropipette tip. The detached cells were removed by gently washing twice with PBS and wells refilled with 2ml/well of fresh DMEM media comprising the unformulated extract and NP2 at concentrations of 100 and 200 μg/ml, and RA as a positive control at 100 μg/ml. Negative control cells were treated with the vehicle only. Subsequently, the wounds were imaged at zero time using an inverted light microscope at lOx magnification. Cells were photographed at 12 and 24hr to assess cell migration into the wound. Photographs were taken under an inverted light microscope supplied with Leica Quin computerized imaging system and percentage inhibition of migration calculated as described in Example 6. Results are shown in Table 29. Table 29. Percentage inhibition of A549 cell migration after 12 and 24 h and percentage inhibition of EA.hy926 cell migration after 12 and 18 h treatment with 100 and 200μg/ml of the unformulated extract (E-100 and E-200) manufactured as described in Example 1, and 100 and 200μg/ml of said extract formulated as NP2 (NP2-100 and NP-200), and 100 μg/ml of RA (RA-100) as a positive control. Results are expressed as mean ± SD compared to negative control, n = 3, *p≤ 0.05 compared to negative control.
[0620] The effect of an unformulated extract of O. stamineus leaves manufactured as described in Example 1 and said extract formulated as NP2 on aggregation of cancer cells was evaluated as follows. A549 cells were suspended in DMEM culture medium
supplemented with 10% HIFBS, 1% PS and 1% D-glucose, which is used to enhance viscosity of the medium (Sigma-Aldrich, USA) at a cell density of 2.5 x 105 cells/ml of single-cell suspension. 20μΙ drops of the cell suspension at a density of 5000 cells/drop were placed onto the inner surface of lids of a petri dish sufficiently apart to prevent them from touching each other. The lids were gently inverted over a petri dish containing 5 ml of DMEM medium to maintain the humidity of the dish, which is used as a hydration chamber. The petri dish was then incubated in a humidified incubator at 37°C and 5% CO2 to allow growth of the spheroids. The drops were routinely monitored under an inverted light microscope (EVOS fl) (AMG: Advanced Microscopy Group, USA) to allow sedimentation of cells as a single mass until sufficient formation of hanging drops after about 5 days. Spheroids were then transferred to 48-well plates coated with 2% (wt/vol) agarose. Each well was subsequently filled with 250 μΙ/well of DMEM medium supplemented with 10% HIFBS and 1% PS.
Spheroids were allowed to settle onto the bottom of the wells for lhr, after which spheroids were treated with 250 μΙ/well of DMEM medium comprising the extract of Example 1 or NP2 to obtain a final concentration of 100 and 200 μg/ml. DMEM medium containing 1% deionized distilled water served as the negative control and RA at 100 μg/ml was used as a positive control. The experiment was run in six replicates. Following the treatment, drops were imaged at 4x magnification using a digital inverted microscope (EVOS fl) (AMG:
Advanced Microscopy Group, USA) at time intervals of 0, 3 and 6 days. Results were analyzed by microscopic characterization of spheroid morphology and measuring the diameter of spheroids using ImageJ software (http://rsb.info.nih.gov/ij/); where the volume of each spheroid was calculated as follows:
Spheroid volume = 4/3 π r3, r = radius
[0621] The results are shown in Table 30. % inhibition of spheroid formation is expressed as follows:
% inhibition of spheroid formation = (l-(volT/volNc)) x 100 where, VolT = volume of treated spheroids and VolNc = volume of untreated spheroids.
Table 30. Effect of an extract of O. stamineus leaves manufactured as described in Example 1 at 100 and 200Mg/ml (E-100 and E-200), said extract formulated as NP2 at 100 and 200 μ /ιηΙ (NP2-100 and NP2-200), and RA at 100 Mg/ml on volume of spheroid formation by human lung adenocarcinoma cells. Values are presented as percentage inhibition of spheroid formation (mean ± SD), n = 3, *p≤ 0.05 relative to negative control.
[0622] The effect of an unformulated extract of O. stamineus leaves manufactured as described in Example 1 and said extract formulated as NP2 on cell invasion was determined on A549 cells as follows. Matrigel® (10 mg/ml) was liquefied, then mixed with DMEM culturing medium at a ratio of (1:1). The diluted Matrigel was pipetted into a 96-well plate (50 μΙ/well) using pre-chilled pipettes and plate, followed by incubation at 37°C incubator for 45 min to be solidified. A549 cells were seeded into the 96-wells plate (5000 cells/well) in DMEM medium (150 μΙ/well) comprising either the extract of NP2 at concentrations of 100 and 200 μg/ml. RA at 100 μg/ml was used as the positive control. Some cells were seeded in DMEM and vehicle only as the negative control. Cells were cultured in a humidified incubator at 37°C and 5% CO2 for a further 24 h after which the upper media was aspirated carefully and wells washed twice with lx PBS to remove any cells that hadn't invaded the Matrigel to prevent disruption of the Matrigel layer. Wells were photographed at 4x magnification using an inverted microscope connected to a digital imaging system.
Quantification of invasiveness of the treated A549 cells was performed by counting the number of the invaded cells in the treated wells with comparison to that of the untreated negative control wells. The results, calculated using the equation shown in Example 7, are presented in Table 31.
Table 31. Effect of an unformulated extract of O. stamineus leaves manufactured as described in Example 1 at 100 and 200
(E-100 and E-200), said extract formulated as NP2 at 100 and 200
(NP2-100 and NP-200) and RA at 100 (RA-100) on cell invasion of A549 cells relative to untreated Cells. Values are presented as % inhibition of cell Invasion compared to negative control ± SD. n = 3, *p < 0.05; **p < 0.01.
[0623] The effect of an unformulated extract of O. stamineus leaves manufactured as described in Example 1 and said extract formulated as NP2 on capillary-like tube formation by EA.hy926 endothelial cells was evaluated as follows. Low passage number EA.hy926 cells were seeded at a density of 2xl05 cells/ml of DMEM in cell culture flasks and incubated for 24 h until 70% confluency. Cells were treated in quadruplicate for an additional 24 h with DMEM medium comprising the extract and NP2 at concentrations of 50 and 100 μg/ml each. RA was used as a positive control at 50μg/ml, while negative control cells received vehicle. Matrigel" BD (10 mg/ml) (Bioscience, USA) at 4°C was mixed gently (1:1 v/v) with cold DMEM culture medium. A sterile 48-well plate was coated with the Matrigel mixture (150 μΙ/well), followed by 45 min incubation at 37°C and 5% CO2 to form a gelled basement membrane. The treated cells were trypsinized, harvested carefully, counted and diluted in DMEM medium to 2 χ 105 cells/ml. 500 μΙ/well of the diluted cell suspension was pipetted slowly onto the top of Matrigel matrix; and re-incubated for 16 h. Capillary-like tubular networks formed in the wells at the end of the 16 h incubation were imaged using an inverted light
microscope (EVOS fl) (AMG: Advanced M icroscopy Group, USA) with a digital camera at 4x magnification. The images were analysed by quantifying the area included by the capillarylike tubules, tube number, tube length or number of branching points. The capillary-like tube-structure area was measured as described in (297) and (279) using ImageJ software (http://rsb.info.nih.gov/ij/). % inhibition of capillary-like tube formation was calculated using the following formula:
% of inhibition of tube formation = (l-(Areas/AreaNc)) x 100 where, Areas = area of tubules in the treated wells, and AreaNc = the area of tubules in untreated wells (negative control). The results are shown in Table 32.
Table 32. Effect of an unformulated extract of O. stamineus leaves manufactured as described in Example 1 at 50 and 100 μg/ml (E-50 and E-100), said extract formulated as NP2 at 50 and 100 μg/ml (NP2-50 and NP2-100) and RA at 50 μg/ml (RA-50) on capillary-like tube formation of EA.hy926 cells relative to untreated cells. Values are presented as % inhibition compared to negative control ± SD. n = 2, **p < 0.01.
[0624] The effect of an unformulated extract of O. stamineus leaves manufactured as described in Example 1 and said extract formulated as NP2 on VEGF165 expression by A549 cells in-vitro was evaluated as follows. A549 cells were used as an in-vitro model for VEGF expression in human lung cancer (298). The assay was performed using an ELISA kit for human VEGF165 (DuoSet® ELISA Development System, USA). A549 cells were treated with an unformulated extract of O. stamineus leaves manufactured as described in Example 1 and N P2 at 200 and 400 μg/ml for 24 h. As a negative control, cells were treated with DDW using DM EM culture medium. Cells were subsequently trypsinized and lysed with lysis buffer (Wizard* SV, Promega, Madison, USA), centrifuged at 10000 rpm at 4°C. 100 μΙ of the supernatant was pipetted into each well of a 96-well plate of the kit in triplicate (the wells were previously coated with a specific capture antibody for human VEGF). The amount of VEGF165 in the lysates was quantified according to the kit manufacturer's instructions. The concentration of VEGF in the A549 cells was calculated from the regression equation as pg/ml of cell lysates. % inhibition of VEGF expression was calculated using the following equation:
% VEGF inhibition = (1- (VEGFS/ VEGFNC)) *100 where, VEGFS = VEGF concentration of the samples, VEGFNC = VEGF concentration of the negative control. Results of this experiment are presented in Table 33.
Table 33. Effect of an unformulated extract of O. stamineus leaves manufactured as described in Example 1 at 200 and 400 μg/ml (E-200 and E-400), and said extract formulated as NP2 at 200 and 400 μg/ml (NP2-200 and NP-400) on expression of VEGFi65 in A549 Cells. Values are presented as % inhibition of VEGFi6s expression compared to negative control ± SD. n = 3, **p < 0.01.
% Inhibition of VEGFi65
Expression in A549 Cells
E-200 28.36 ± 2.84**
E-400 47.91 ± 4.13**
NP2-200 40.11 ± 3.33 **
NP2-400 67.14 ± 2.09**
[0625] In vivo anti-tumour efficacy of an unformulated extract of O. stamineus leaves manufactured as described in Example 1 and said extract formulated as NP2 was evaluated using ectopic human lung adenocarcinoma xenograft tumour model (A549 cell line) in immunocompromised (N C-nu/nu) nude mice.
[0626] Athymic NCR nu/nu nude mice aged 4-6 weeks with a weight of 25-30 g were obtained from Taconic Farms Inc., USA. Specific pathogen free cages, each with high efficiency particulate air filter, using animal transport unit (Allentown, USA) were used to house the mice. Sterile food, water and bedding were provided and mice were housed under a standardized 12/12 h light/dark cycle at a room temperature of 24 ± 2°C and a humidity of 60%. Sterile bedding was changed twice a week. All in-vivo studies were conducted according to ethical guidelines and were approved by the ethical committee of Universiti Sains Malaysia.
[0627] The A549 cell line was selected as a model of lung cancer (299). Cells were maintained in DMEM cell culture medium supplemented with 10% HIFBS and 1% penicillin/streptomycin solution. Lower passage number cells (<10) were used. 90% confluence of A549 cells in T25 culture flasks were detached using trypsin and re-suspended in 5ml of fresh DMEM medium, then centrifuged at 1000 rpm for five minutes and washed with sterile PBS to remove the trypsin. Cells were then concentrated into 5x10s cells/200 μΙ in DMEM.
[0628] 5 x 10s A549 cells in 200μΙ DMEM medium were injected subcutaneously into the right flank of the thirty athymic nude mice using a 27-gauge needle connected to a 1ml syringe under aseptic conditions. The needle was removed, and injection site was gently compressed with a sterile cotton swab and inspected for 30 seconds to ensure no leakage of the cells after which mice were returned to their cages. Once the average tumor volume reached about 100 mm3, (i.e. in ten-days post cell inoculation), the mice were then randomly divided into 5 groups of 6-mice each.
[0629] Each group of mice was treated orally using oral gavage (20 G needle) with 200 μΙ of the appropriate treatment per mouse daily for 28 days. All treatment samples were prepared in distilled water. One group of mice received only distilled water (negative control); another three groups received the unformulated extract at 100, 200 and 400 mg/Kg body weight (E-100, E-200, and E-400). Three other groups were treated with the NP2 at doses of 100, 200 and 400 mg/Kg body weight (NP2-100, NP2-200, and NP2-400). One group was treated with the standard reference imatinib (Novartis, Switzerland) at 20 mg/Kg body weight as a positive control (1-20) (300).
[0630] Size of tumors with more than one lobe was calculated by summation of the size of individual lobes (301). The tumour size and body weight of the mice were recorded before starting the treatment and at 7-days intervals until the end of the experiment.
Depending on the tumour volume, the percentage inhibition of tumour growth was measured at the end of the experiment (i.e. day 28) (286) as follows:
Percentage inhibition of tumour growth = (1 - (ΔΤ/ΔΟ)) x 100
where, ΔΤ = Τ28-Δ0 and AC = C28-Ao
Δο = the average of tumour volume at the beginning of the treatment (day 0).
T28 = the average tumour volume at the day 28 for the treated groups.
C28 = the average tumour volume at the day 28 for the negative control group.
[0631] The results are shown in Table 34.
Table 34. Dose dependent effect of an unformulated extract of O. stamineus leaves manufactured as described in Example 1, said extract formulated as NP2, and imatinib on tumor volume (mm3) and percent inhibition of tumor size (relative to vehicle at Day 28) in response to various treatments in a short-term study (28 days) on tumor Size of ectopic xenografts of human lung adenocarcinoma in nude mice. Values are presented as ± SD. n = 6, *p < 0.05 compared to vehicle, **p < 0.05 in comparison to O. stamineus extract at 400mg/kg body weight.
[0632] At the end of the experiment, mice were sacrificed by euthanizing with CO2, followed by cervical dislocation. The effect of the various treatments on the gross morphology of the tumors is shown in Fig. 6. The subcutaneous tumors once removed, were weighed in grams and percentage inhibition of tumour weight was calculated as follows:
Percentage of tumor weight inhibition = (1- (TWS/ TWNC)) xl00 where: TWS = tumor weight (g) of the samples, TWNc = tumor weight (g) of the negative control. The results are shown in Table 35.
Table 35. Dose dependent effect of an extract of O. stamineus Leaves manufactured as described in Example 1, said extract formulated as NP2, and imatinib on tumor weight at Day 28 in response to the extract of Example 1, and imatinib in a short-term study (28 days) on tumor size of ectopic xenografts of human lung adenocarcinoma cells in nude mice. Values are presented as ± SD. n = 6, *p < 0.05 compared to negative control (vehicle).
E-400 69.23 ± 4.48*
NP2-100 49.60 ± 6.30*
NP2-200 68.50 ± 6.79*
NP2-400 86.02 ± 3.46*
1-20 88.52 ± 5.21*
[0633] Each tumor was then divided into two pieces, one piece was preserved in 4%
paraformaldehyde and sent to Gribbles pathology laboratories (Penang, Malaysia) for
preparation of cross sections which were stained with eosin/hematoxylin for histological
analysis. The other half of the tumor was processed for expression of VEGF165 as described below. Slides bearing the cross sections were imaged microscopically at lOx magnification to check for extent of vascularization; morphology, apoptosis and necrosis of the tissue using light microscope (Olympus BX41, Japan) connected to a digital camera and a specific imaging software (Olympus Cell A, Japan). Intra-tumor blood vessels were counted in 10 microscopic fields, then measure the average number of intra-tumor blood vessels per field, from which the percentage inhibition of the intra-tumor blood vessels per field was calculated from the following equation.
Percentage inhibition of intra-tumor blood vessels= (l-(N IBVT/NI BVNc)) x 100
where: N I BVT = Number of intra-tumour blood vessels of treated samples, and NI BVNC =
Number of intra-tumour blood vessels of negative control. The results are shown in Table
36. The change in weight gain over the treatment period is shown in Table 37.
Table 36. Dose dependent effect of an extract of O. stamineus leaves manufactured as described in
Example 1, said extract formulated as NP2, and imatinib compared to negative control on intra-tumor blood vessel number at day 28 in response to the extract of O. stamineus leaves, and imatinib in a
short-term study (28 days) on tumor size of ectopic xenografts of human lung adenocarcinoma in
nude mice. Values are presented as ± SD. n = 6, *p < 0.05 compared to negative control (vehicle).
Table 37. Dose dependent effect of an extract of O. stamineus leaves manufactured as described in
Example 1, said extract formulated as NP2, and imatinib on weight gain in response to the extract of
Example 1, and imatinib in a short-term study (28 days) for treatment of ectopic xenografts of human lung adenocarcinoma in nude mice. Values are presented as ± SD. n = 6, p > 0.5 compared to negative control.
Body Weight (g)
Treatment
Prior to Day 0 Day 7 Day 14 Day 21 Day 28 Injection
Vehicle 30.62 ± 2.39 28.83 ± 2.18 29.45 ± 2.62 29.20 ± 4.34 29.49 ± 3.98 29.42 ± 3.57
E-100 29.71 ± 2.21
27.60 ± 2.44 28.76 ± 1.46 29.77 ± 1.94 29.08 ± 2.77 29.55 ± 2.03
E-200 29.07 ± 3.33 30.78 ± 1.46 31.95 ± 3.70 30.57 ± 4.13 29.73 ± 3.89 30.74 ± 4.31
E-400 30.93 ± 2.28 31.57 ± 3.36 29.84 ± 3.18 28.41 ± 3.64 30.73 ± 2.60 30.46 ± 2.70
NP2-100 29.08 ± 2.64 30.31 ± 2.35 29.88 ± 2.74 30.01 ± 2.34 28.86 ± 3.11 28.19 ± 3.31
NP2-200 30.15 ± 2.43 29.55 ± 2.20 29.59 ± 2.79 28.72 ± 2.95 28.66 ± 4.56 28.29 ± 4.14
NP2-400 27.35 ± 2.26 28.79 ± 2.21 29.26 ± 1.56 29.20 ± 1.74 28.54 ± 3.23 28.97 ± 2.98
1-20 26.93 ± 1.39 27.47 ± 1.71 26.62 ±1.30 26.10 ± 2.11 26.51 ± 1.25 27.32 ± 1.58
[0634] The effect of various doses of an unformulated extract of O. stamineus leaves manufactured as described in Example 1, and such extract formulated as N P2 on expression of VEGFi65 was assessed as follows. 100 mg of tumor tissue from each animal treated with either 100, 200 or 400 mg/Kg body weight of the unformulated extract (E-100, E-200, and E- 400), N P2 at doses of either 100, 200 or 400 mg/Kg body weight (N P2-100, N P2-200, and
N P2-400), and imatinib at 20 mg/Kg body weight as a positive control (1-20) was
homogenized in 1 ml of lx cell lysis buffer (Wizard* SV, Promega, Madison, USA) using a
homogenizer until complete lysis of the tissue. Homogenates were centrifuged at 10000 rpm for 10 min at 4°C, and supernatants assessed for quantitative analysis of human VEGF165
expression in lung tumour tissue homogenates as described above. The concentration of
VEGF165 in the tumour tissue homogenates was calculated from the regression equation of the calibration curve of the VEGF-standard as pg/ml of tissue homogenate, from which
percentage inhibition of VEGF165 expression was calculated using the following equation:
Percentage of VEGFi65-expression inhibition = (1- (VEGFs/ VEGFNC)) xlOO
where, VEGFs = VEGF165 concentration of treated samples, and VEGFNC = VEGF165 concentration of tissue treated with negative control. Results are presented in Table 38.
Table 38. Effect of an unformulated extract of O. stamineus leaves manufactured as described in
Example 1 at 100, 200 and 400 mg/kg body weight (E-100, E-200, and E-400), and said extract
formulated as NP2 at 100, 200, and 400 mg/kg body weight (NP-100, NP-200 and NP-400), and
imatinib at 20mg/kg body weight on expression of VEG Fi6s in human lung adenocarcinoma tumors.
Values are presented as % inhibition of VEGFi6s expression compared to negative control ± SD. n = 3,
*p < 0.05 compared to negative control.
Example 16. Effect of an Extract of O. stamineus Leaves Manufactured as Described in
Example 1 on Vascular Normalization and Treatment of Occular Related Physiological
Disorders
[0635] The effectiveness of the extract on treatment of: 1) retinal ischemia, and 2) vascular normalization in the context of treatment of diabetic retinopathy was evaluated in this example.
[0636] In situ gel compositions comprising either an extract of O. stamineus leaves manufactured as described in Example 1 or control blank were prepared by the cold method. A weighed amount of poloxamer 407 and poloxamer 188 (15 - 20% w/v) was slowly added to 15 mL water in a beaker with continuous stirring using a magnetic stirrer at a speed of 500 rpm for 2 hrs. The solution was kept overnight in a refrigerator. HPMC K-100 (0.5% w/v) and carbopol 934 (0.5% w/v) was sprinkled slowly into the poloxamer solution with continuous stirring. The preservatives, methyl paraben (0.1% w/v) and propyl paraben
(0.01% w/v) were prepared separately by solubilizing in hot water. These preservatives were then added to the previous dispersion after cooling. A weighed amount of the extract (2% and 10% w/v for treatment of diabetic retinopathy and 5% for treatment of retinal ischemia) or blank was dissolved in a mixture of Tween 80 and glycerin at a ratio of 1:2. The extract mixture was added to the poloxamer dispersion containing preservatives. The final volume was made up and pH was adjusted to 7 by adding triethanolamine drop-by-drop.
[0637] For the treatment of diabetic retinopathy, 8-week-old male Sprague Dawley rats, weighing 200 ± 20g, were provided by the EMAN Biodiscovery (Pinang, Malaysia). Animals were acclimatized to the laboratory environment for 1 week (cyclic light (12 L:12 D) condition) with unlimited access to water and a commercial laboratory chow. All experiments were performed in compliance with the Animal Experimental Ethics Committee of Universiti Sains Malaysia. Following the 1-week acclimatization period, all rats were fasted overnight and equally divided into two groups. All animals in Group 1, the experimental group, received an intraperitoneal injection of STZ (dissolved in ice-cold saline) at a dose of 55 mg/kg to induce diabetes. Group 2, the control group, received physiological saline of same volume also by intraperitoneal injection. After 72 h, the blood was collected from the tail vein of all animals in both groups to measure FBG level. Rats with the FBG levels higher than 15.0 mmol/L in Group 1 were used as the diabetic subjects for further study. The survival rate of the animals in Group 1 and 2 was 100%. Prior to model establishment, there was no significant difference in body weight of animals in either group. After model establishment, rats in Group 1 demonstrated loss in body weight, polyuria, hair color dullness and tail skin ulcers, skeletonization of torso and head, and withered hair. From the first week onward, compared with animals in Group 2, animals in Group 1 demonstrated a significant decrease in body weight and increase in blood glucose (p < 0.05). Over time, the weight of the rats in Group 2 increased continuously, whereas the weight of the animals in Group 1 decreased continuously. Blood glucose was unchanged at each measurement in the animals in Group 2 (p < 0.05), whereas the blood glucose concentration in the animals in Group 1 was significantly increased and maintained at approximately 16 mmol/L throughout the experimental period. The rats in both normal control and STZ-induced diabetic groups received the blank in situ gel composition (30 μΙ/eye) on the left eye and the in-situ gel composition comprising the extract of Example 1 (30 μΙ/eye) on the right eye daily for 21 days. The FBG level was measured every week to insure the rats remained diabetic and photographs of the retina in both eyes of normal and STZ-induced diabetic rats were taken at adequate intervals to evaluate the fundoscopic changes using Panoptic™ ophthalmoscope (Welch Allyn, USA). On day 21, the FBG level was measured and the image of retina was
captured for further study. The effect of the 21-day treatment of the extract on vascular normalization on diabetic retinopathy in diabetic rats versus normal rats is shown in Fig. 7.
[0638] The effect of an extract of O. stamineus manufactured as described in Example 1 on ischemic cell death was evaluated in-vitro on 28 cells. R28 cells, purchased from Kerafast, USA, are known to exhibit several biochemical characteristics associated with retinal cells. R28 cells were maintained in Dulbecco's modified Eagle's medium (D-MEM; Sigma-Aldrich) supplemented with 10% fetal bovine serum (FBS; Invitrogen, Paisley, Scotland, UK) 25 mM glucose, 100 U/mL penicillin (Invitrogen), and 100 μg/ml streptomycin (Invitrogen) in a humidified atmosphere of 95% air and 5% CO2 at 37°C. Doubling time of the cells was approximately 20 hours. Confluent cultures of R28 cells from 75-cm2, filter capped cell culture flasks were passaged at a ratio of approximately 1:8 to give a cell density of approximately 4 to 5 χ 104cells/mL. One hundred microliters of these cells were plated onto 96-well plates (Corning, USA) or 500μί of cells were plated onto sterilized borosilicate glass coverslips in 24-well plates. R28 cells were seeded and incubated as described above for 24 h. All parts of the 96-well plate except for two columns were rinsed after the incubation for two to three times with serum-free medium. The cells then were treated with different concentrations of an extract of O. stamineus leaves manufactured as described in Example 1. Untreated wells that had not been rinsed with serum-free medium were used as positive controls in this assay. Following 48 h of incubation after treatment, MTT was added to each well. The plates were further incubated for 3-5 h at 37°C. The medium then was aspirated from each well and DMSO was added to dissolve the formazan crystals formed. The optical density of each well was measured using the microplate reader at a test wavelength of 570 nm, with 620 nm as the reference filter. The data for the effectiveness of the extract on inhibiting serum deprived cell death is shown in Table 39.
Table 39. Effect of increasing concentrations of an extract of O. stamineus manufactured as described in Example 1 (E) on serum-deprived cell death of R28 cells relative to control in-vitro.
[0639] The effectiveness of above the in-situ gel composition comprising the extract at 5% (w/v) in the treatment of retinal ischemia was evaluated on nu/nu Nude mice in-vivo. The animals were obtained from Jackson Laboratory, USA and maintained under sterile conditions with the aid of individually ventilated cages.
[0640] The retinal ischemia procedure was performed on the mice after anesthesia with ketamine (80 mg/kg body weight) and xylazine (20 mg/kg body weight) via
intraperitoneal injection. Retinal ischemia-reperfusion injury was achieved by transiently (30s) stopping blood flow at day 1 and 7 after pre-treatment with the gel composition comprising 5% of the extract. A 0-5 nylon suture was slit around the eyeball forming a loop around the optic nerve bundle immediately posterior to the eye ball for 30 seconds. The
loop around the optic nerve bundle was tightened until the clear translucent cornea appeared pale white due to a decrease in blood flow. The loop was removed after 30 seconds of ischemia to allow reperfusion. The animals were anesthetized throughout this procedure. The effect of the composition comprising 5% of the extract on the treatment of retinal ischemia was then evaluated by analyzing the intensity levels of ProSense® 750 EX (VisEn Medical, Bedford, MA, USA) - a protease activatable fluorescent in vivo imaging agent that is activated by key disease associated proteases such as Cathepsin B, L, S and plasmin. ProSense750 EX is optically silent in its unactivated state and becomes highly fluorescent following protease-mediated activation.
[0641] Changes in fluorescence were detected and measured using the FMT 2000
Fluorescence Tomography System. The preparation for FMT imaging was initiated 24 hr after retinal ischemia was induced. Animals were anesthetized as described above and then injected intravenously via a tail vein with 1 nmol ProSense 750 EX in 100 μΙ of PBS. 24 hours after ProSense injection, animals were anesthetized again and imaged by FMT, which detects fluorescence and resolves probe signal in the targeted region. For in vivo imaging of mice with the ProSense 750 EX, a fluorescent channel of 750/680 nm was chosen for this study. To measure the inflammatory response to retinal ischemia, analysis of FMT images were focused on two anatomical positions specific to the eye region. Two fluorescent intensity measurements were recorded for each position corresponding to the fluorescence emission and excitation. The FMT readings of changes in fluorescence intensity, which is directly related to the activity of proteases in response to the ischemia in the region of interest of the experimental groups, was collected using the FMT software and exported to Microsoft Excel for further analysis. The effectiveness of the extract of Example 1 in the treatment of retinal ischemia is shown in Table 40.
Table 40. The effect of an extract of O. stamineus leaves manufactured as described in Example 1 (E) on the treatment of retinal ischemia (Rl) in-vivo. Values are expressed as level of fluorescence intensity as measured by FMT imaging ± SD. n = 5, were *p<0.05 compared to untreated control.
Example 17. In-Vitro Effect of an Extract of O. stamineus Leaves Manufactured as Described in Example 1 on the Expression of Factors that Modulate Angiogenesis.
[0642] The effect of an extract of O. stamineus leaves manufactured as described in Example 1 on the expression of a select number of pro-angiogenic and anti-angiogenic factors in comparison to A, SIN, EUP, and TM F was evaluated using a human angiogenesis antibody array (RayBio® Human Angiogenesis Antibody Array 1 (G Series), Ray Biotech, Inc., Norcross, GA).
[0643] The effect of the treatments on the expression of both pro- and anti-angiogenic factors was tested on EAhy926 endothelial cells (ATCC, Rockville, USA). Cells were cultured in RPMI 1640 (GIBCO, Thermo Fisher Scientific Inc., USA) and DMEM supplemented with 5% of fetal bovine serum and penicillin (final concentration of 1 mg/mL) and streptomycin (final
concentration of 200
A confluence of 70-80% cells were used for seeding in 96-well plates (100 μΐ cells/well) and incubated (0.25-250 μg/mL) for 48 h at 37°C/5% C0
2. Cells were treated for 24hr at 37°C/ 5% C0
2 with either extract from Example 1 at 1000 μg/mL, RA and SIN at 400 μg/mL, and EUP and TMF at 100 μg/mL Preparation of the cell lysates and processing of the array was performed according to the manufacturer's instructions. The array was subsequently quantified by Genomax Technologies (Genomax Technologies Pte Ltd, Singapore). The data are shown in Table 41.
Table 41. Effect of an extract of O. stamineus leaves manufactured as described in Example 1 (E), RA, SIN, EUP, and TMF on expression of factors chosen from pro- and anti-angiogenic factors in endothelial cells (negative numbers represent decreased expression and positive numbers represent increased expression).
Example 18. Effect of an Extract of O. stamineus Leaves Manufactured as Described in
Example 1 on the Expression of CA9.
[0644] The effect of an extract of O. stamineus leaves manufactured as described in Example 1 on expression of CA9 was tested in a human colorectal carcinoma cell line HCT- 116 (ATCC, Rockville, USA), which was maintained in RPM I 1640 medium containing L- glutamine supplemented with 10% heat-inactivated FBS and 1% penicillin streptomycin (100 units/ml) in an atmosphere of 5% C02 at 37°C, and a human breast adenocarcinoma cell line MCF-7 (ATCC, Rockville, USA), which was maintained in Dulbecco's Modified Eagle medium (DMEM) containing 10% fetal bovine serum, supplemented with penicillin streptomycin (100 units/ml), and and L-glutamine (2 mM) in an atmosphere of 5% CO2 at 37°C.
[0645] The HCT-116 cells were treated with the extract at 50 μg/ml (E-50), 100 μg/ml
(E-100), and 200 μg/ml (E-200). MCF-7 cells were treated with the extract at 100 μg/ml (E- 100), 200 μg/m\ (E-200), and 400 μg/m\ (E-400). Untreated cells (with 1% DMSO as vehicle) served as a control for both cell lines. Cells were treated for 24hr at 37°C/5% CO2. The level of CA9 expression was quantified using a Quantikine® ELISA Human CA IX Immunoassay kit (Catalog No. DCA900, R&D Systems, Minneapolis, Minnesota, USA). Preparation of the cell lysates and processing of the ELISA was performed according to the manufacturer's instructions. The data are presented in Table 42.
Table 42. Dose dependent effect of an extract of O. stamineus leaves manufactured as described in Example 1 (E) on the expression of CA9 in human colorectal cancer cell line (HCT-116) and human breast cancer cell line (MCF7). Fold expression is relative to control. Values are expressed as ± SD, n = 2, *p < 0.05 compared to control.
Example 19. Effect of an Extract of O. stamineus Leaves Manufactured as Described in
Example 1 on Multidrug Resistance (MDR).
[0646] The effect of an extract of O. stamineus leaves manufactured as described in Example 1 on MDR was assessed by evaluating the expression of the MDR-1 and ABCC-4 (also known as MRP-4) genes in human pancreatic cancer cells.
[0647] Panc-1 (human pancreatic cell line) was obtained from ATCC (Rockville, USA). Panc-IGEM resistance cells were generated through subcutaneous injection of Panc-1 cells into SCID mice for 3 months and treated with gemcitabine (50 mg/kg). GEM resistant tumors were isolated and cells were isolated for resistance study in vitro.
[0648] All cells were grown in Dulbecco's Modified Eagle's Medium (DMEM) containing 10% fetal bovine serum, 2 mM L-glutamine and penicillin/streptomycin (0.5 U/ml and 150 g/ml) in 5% of CO2 at 37°C. Eighty to ninety percent confluent cultures in T75 flasks were trypsinized and resuspended in 5 mL fresh medium, the cells were collected by
centrifugation at 1000 rpm for 5 min and washed with a sterile PBS to remove the trypsin. The cells were subsequently re-suspended in DMEM and transferred to a six-well plate at a density of 3000 cells/well. Cells in each well were either left untreated, treated with PBS as a control or treated with the extract at a concentration of 60 μg/ml or 80 μg/ml or with EUP at a concentration of 25 μΜ or 50 μΜ for 72hr at 37°C/5% C02. Total RNA was isolated from the cells at the end of the treatment period using GENEzol™ Reagent (Geneaid Biotech Ltd, New Taipei City, Taiwan) according to the manufacturer's instructions. The isolated RNA was converted to cDNA using BIOLINE ISOLATE kit (BIOLINE Inc., Taunton, MA, USA) according to the manufacturer's instructions. The resulting cDNA was amplified on a 7500 Fast Real-Time PCR System (Applied Biosystems®, Foster City, CA, USA) using a KAPPA SYBR® Fast qPCR
Master Mix (2X) Kit (KAPABIOSYSTEMS, Boston, MA, USA).
[0649] Relative amount of target gene (M DR-1 and M RP-4) mRNA expression was calculated using the comparative threshold cycle Ct AACt method :
AACt method = (Ct(Target sample) - Ct(Target gene sample)) - (Ct(Target control) - Ct(Target gene control))
[0650] The RT-PCR data was normalized to the housekeeping genes β-actin and GAPDH, which were quantified using the same method. Each QRT-PCR analysis was performed in triplicate from triplicate biological samples. The results of this example are shown in Tables 43 and 44.
Table 43. Effect of an extract of O. stamineus leaves manufactured as described in Example 1 and Eupatorin on multidrug resistance in cancer cells relative to GAPDH mRNA expression. Values are expressed as ± SD, n = 3, *p < 0.05, * *p < 0.01, ** *p < 0.001, relative to untreated Panc-1 PBS, and ***p < 0.001 relative to untreated Panc-1 Gem.
Table 44. Effect of an extract of O. stmineus leaves manufactured as described in Example 1 and Eupatorin on multidrug resistance in cancer cells relative to β-Actin mRNA expression. Values are expressed as + SD, n= 3, *p < 0.05, * *p < 0.01, ** *p < 0.001 relative to untreated Panc-1 PBS, and < 0.01, *** p < 0.001 relative to untreated Panc-1 Gem.
Example 20. Effect of an Extract of O. stamineus Leaves Manufactured as Described in Example 1, RA and Imatinib on the Expression of Factors Affecting Cellular Pathways
[0651] This example illustrates: 1) the effect of the 28-day treatment of an extract according to Example 1, RA, and imatinib, as described in Example 11, on the expression of VEGF, EGF, b-FGF, I L-2, I L-7, β-NGF, TGF-ot, TN F-ot, TNF-β, GM-CSF, IFN-ot, IFN-β, and I FN-γ in human colorectal tumors, 2) the effect the expression of VEGF, EGF, b-FGF, I L-2, I L-7, β-NGF, TGF-ot, TN F-ot, TN F-β, GM-CSF, I FN-ot, I FN-β, and IFN-γ in H UVECs treated for 24hr with
either an extract according to Example 1, A and imatinib, 3) expression of multiple regulatory proteins implicated in apoptosis, and 4) the effect of an extract according to Example 1 and formulated as NP2 on expression of transcription factors.
[0652] Colorectal tumor lysates, prepared as described in Examples 12 were used for determining the effect of the extract of O. stamineus leaves, imatinib, and/or RA on the expression of the various factors listed above. HUVEC lysates were prepared by the same method used to prepare tumor lysates.
[0653] The concentration of VEGF, EGF, b-FGF, I L-2, I L-7, β-NGF, TGF-ot, TN F-ot, TNF-β, GM-CSF, IFN-ot, I FN-β, and I FN-γ in HUVEC lysates and lysates of human colorectal tumors from Example 11 were determined using the Luminex® Multiplexing Platform (xMAP® Technology, Luminex® Corporation, TX, USA). Standard calibration curves were used to calculate concentrations of VEGF, EGF, b-FGF, IL-2, IL-7, β-NGF, TGF-ot, TN F-ot, TN F-β, GM- CSF, I FN-ot, I FN-b, and IFN-γ in lysates of tumor tissue samples.
[0654] The Luminex® Multiplexing Platform assay was carried out according to the manufacturer's instructions. The incubations were performed in the dark at RT. Each well of a 96-well filter plate was pre-wetted with 150 μΙ/vjeU of reading buffer for 5 min at RT. The reading buffer was then removed from the plates by vacuum filtration. Next, 50 μΙ/vjeW antibody beads were added to each well. The antibody beads were washed with 150 μΙ/vjeW with IX washing buffer. After removing the washing buffer, the residual buffer was removed by blotting the bottom of the filter plates with paper towels. The standard, blank, and tumor tissue lysates were added (50 μΙ/vjeW) in duplicate. The filter plates were covered with a plate seal wrapped with aluminum foil and incubated for lhr on an orbital plate shaker (500-600 rpm). The liquid was removed from the plates using vacuum filtration. The plates were washed three times with 150 μΙ/vjeW of washing buffer. The biotinylated detector antibody was added (25 μί) to each well and incubated for 30 min at RT on an orbital shaker (500-600 rpm). The solution was then removed and the plates were washed three times with 150 μΙ/vjeU of IX washing buffer. Streptavidin PE was added (50 μΙ/vjeW) and incubated for 30 min on a plate shaker (500-600 rpm). The plates were then washed three times with 150 μΙ/vjeW of washing buffer. Finally, 120 μΙ/vjeW of reading buffer was added to each well. Samples were incubated for 5 min on a plate shaker and then analyzed on the Luminex® 200 (Luminex® Corporation, TX, USA). For each set of microspheres, 100 beads were analyzed and median values were reported.
[0655] The effect of the treatments on the expression of VEGF, EGF, b-FGF, IL-2, IL-7, β- NGF, TGF-ot, TNF-ot, TN F-β, GM-CSF, IFN-ot, IFN-β, and I FN-γ in human colorectal tumors is shown in Table 45.
Table 45. Effect of an extract of O. stamineus leaves manufactured as described in Example 1 (E), RA and Imatinib on the expression of pro- and anti-angiogenic factors in xenograft ectopic human colorectal tumors. All treatments are in mg of treatment/kg body weight of mice. Levels of all factors are expressed in pg/ml. Fold expression is relative to negative control. (-) represents no change. j = decrease, † = increase. Values are represented as mean ± SD, n=4, *p < 0.05, * *p < 0.01 and ** *p <0.001 compared to control group.
IFN-β 0.14 ±0.04 0.4 ±0.04** 0.68 ±0.00*** 0.05 ± 0.9 ±0.00*** 1.7 ±0.01*** 0.44 ±0.01*** 0.48 ±0.02*** 0.14 ±0.00 (-) (2.9 fold T) (4.9 fold T) 0.01*** (6.4 fold T) (12 fold T) (3.1 fold T) (3.4 fold T)
(3.6 fold T)
GM- 59.2 ±6.1 99.1 ±8.4* 144.4 ± 8.4** 136.8 ±9.5** 137.44 ±8.5** 141.8 ±4.1** 172 ±5.3** 130.5 ±8.9** 32.7 ±1.5 CSF (1.8 fold T) (3 fold T) (4.4 fold T) (4.2 fold T) (4.2 fold T) (4.3 fold T) (5.3 fold T) (4 fold T)
[0656] The effect of the treatments on the expression of VEG F, EGF, b-FGF, IL-2, I L-7, β-NGF, TGF-oc, TN F-a, TN F-β, GM-CSF, IFN-a, I FN-β, and IFN-γ in H UVECs is shown in Table 46.
Table 46. Effect of an Extract of O. stamineus Leaves Manufactured as Described in Example 1 (E), RA and Imatinib on the Expression of Pro- and Anti-angiogenic Factors in HUVECs. All treatments are in μg of treatment/ml culture medium. Levels of all factors are expressed in pg/ml. Fold expression is relative to Negative Control. (-) represents no change. j = decrease, † = increase. Values are represented as mean ± SD, n=4, *p < 0.05, compared to control group.
[0645] The effect of an extract of O. stamineus leaves manufactured as described in Example 1 on modulation and expression of transcription factors implicated in signalling pathways of cancer in A549 cells was evaluated using the Dual-luciferase® reporter assay system (Promega, USA). This kit includes various luciferase reporters including TCF/LEF, RBP-JK, p53, SMAD2/3/4, E2F/DP1, NF-κΒ, Myc/Max, H IF- lct, Elk-l/SRF and AP-1. The assay was performed according to the manufacturer's instructions. 50 μΙ of lx Opti-MEM* reduced serum cell culture medium (Gibco*, USA) was pipetted into each well of a 96-well plate of the array to reconstitute DNA constructs, followed by 5 min incubation of the plate at room
temperature under a cell culture laminar flow hood with gentle shaking. Next, a recommended concentration (6 μ\/μg DNA) of the transfection reagent (FuGENE*, Promega, USA) diluted in Opti-MEM medium was slowly dropped into the array plate (50 μΙ/well), followed by further incubation for 20 min at room temperature. A549 cells were re-suspended in Opti-MEM culture medium supplemented with 10% FBS and 1% MEM non-essential amino acids (MEM NEAA, Gibco, USA) without antibiotics at a cell concentration of 1 x 10s cells/ml. Subsequently, 50 μΙ of the cell suspension was pipetted into each well of the plate followed by incubation in a CO2 incubator at 37°C for 24 h to induce cellular transfection. The old Opti-MEM media in the wells was carefully aspirated and replaced with 75 μΙ/well of fresh DMEM culture media supplemented with 10% FBS, 1% penicillin/streptomycin antibiotics and 1% MEM non- essential amino acids in two groups - one was treated with the extract at a concentration of 400 μg/ml, and the other group was the negative control. The experiment was performed in triplicate. The plate was re-incubated for another 24 h in a C02 incubator at 379C. 25 μΙ of passive cell lysis buffer was next added into each well of the plate with gentle shaking in a laminar flow hood for 15 min. The effect of the extract on the expression of the transcription factors was detected using Dual-luciferase® reporter assay system as follows. 50 μΙ of Firefly luciferase assay reagent was pipetted into each well of the assay plate followed by 30 min incubation in the dark at room temperature. Firefly luciferase activity was detected by luminescence measurement using microplate reader (HIDEX, Finland). Immediately after the measurement, Renilla luciferase reagent was freshly reconstituted in a Stop & Glo® buffer of which 50 μΙ was added to each well of the plate and re-incubated for 15 min at room temperature in the dark. A second luminescence measurement was recorded to estimate the Renilla luciferase activity.
[0646] The Firefly /Renilla (FR) ratio was calculated using the luminescence values of Firefly and Renilla luciferase for each treatment. The relative fold change in the expression of each transcription factor was calculated by dividing FR ratio of the treated cells by that of negative control group (untreated cells). Results are presented as mean ± SD of relative fold change in th expression of each transcription factor in relation to the untreated cells, using the following equation.
Relative fold change in pathway activity = (FR ratioE)/(FR ratioNc) where, FR ratioE = Firefly /Renilla ratio of the treated group with the extract, and FR ratioNc =
Firefly /Renilla ratio of the negative control group. Results of this experiment are shown in Table 47. Table 47. Effect of an Extract of O. stamineus Leaves Manufactured as Described in Example 1 on the expression of transcription factors in A549 cells after 24 h treatment. Results are expressed as mean relative fold change in activity of expression factors ± SD, n = 3, *p≤ 0.05 relative to negative control.
Myc/Max 1.02 ± 0.11
HIF-lot 0.66 ± 0.06*
MAPK/E K 2.71 ± 0.01*
MAPK/JNK 0.96± 0.20
[0647] The effect of an extract of O. stamineus leaves manufactured as described in Example 1 on the expression level of various pro-apoptotic and anti-apoptotic proteins in lung cancer (A549) was evaluated using RayBio® human apoptosis antibody array-Gl kit (RayBiotech, Inc., USA). The assay was carried out using an 8-wells pre-coated glass slide of the antibody array system following the manufacturer's suggested protocol.
[0648] A549 cells were seeded at a cell concentration of 10 x 104 cells/ml in DMEM cell culture medium in each well of a 6-well plate and incubated in a C02 incubator at 379C for 24 h. The medium was aspirated and replaced with fresh DMEM medium comprising 400 μg/ml of the extract versus untreated cells, which received vehicle only. The plate was re-incubated for a further 24 h.
Subsequently, cells were washed with lx PBS and lysed with lx proteinase inhibitor diluted in lx cell lysis buffer.
[0649] Cell lysates were analyzed for expression of pro-apoptotic and anti-apoptotic proteins using the apoptosis antibody array system as follows. ΙΟΟμΙ of lx blocking buffer was added to each well of the 8-well plate of the kit followed by incubation for 1 h at room temperature with gentle shaking.
Subsequently, the blocking buffer was aspirated and replaced with 100 μΙ of the sample cell lysates diluted in lx blocking buffer at a ratio of 1:1 (vol/vol). The plate was incubated overnight at 4°C. The solution was aspirated from the plate and the array glass slide was gently washed with wash buffers (I and I I), individually. A biotin-conjugated antibody cocktail mix was freshly prepared in blocking buffer, then pipetted into the array slide (70 μΙ/well), followed by incubation for 2 h at room temperature with continuous gentle shaking. At the end of the incubation period, the cocktail mix of the antibodies was removed from the array plate, and wells washed with wash buffers (I and II), individually. Next, 70 μΙ of conjugated streptavidin was pipetted into each well, then the array slide was covered with a protective slide cover and incubated in the dark for 2 h, with gentle shaking at room temperature. At the end, the streptavidin solution was decanted from the wells and the slide was washed with wash buffers I and II extensively. The slide was completely dried for fluorescence scanning, which was performed at
Genomax® Technologies (Singapore) on an Agilent G2505C (Agilent, USA) microarray scanner. Image Studio Lite software (LI-COR, Biotechnology) was used to identify and label each spot in the array. The relative expression index was calculated to indicate up-regulation (+ve value) or down-regulation (-ve value) of each protein in relation to the untreated cells. Results of this assay are shown in Table 48.
Table 48. Effect of an extract of O. stamineus leaves manufactured as described in Example 1 on the expression pattern of multiple regulatory proteins of apoptosis.
Relative fold Relative expression Regulatory
Proteins
change index direction
Bax 2.84 2.84 Up
bcl-w 2.44 2.44 Up
BID 4.32 4.32 Up
Caspase3 36.04 36.04 Up
IGF-II 2.43 2.43 Up
IGFBP-1 4.07 4.07 Up
IGFBP-5 2.01 2.01 Up
TRAILR-1 1.62 1.62 Up
bcl-2 0.14 -7.37 Down
BIM 0.50 -2.01 Down
clAP-2 0.38 -2.65 Down
IGFBP-3 0.26 -3.91 Down
IGFBP-6 0.28 -3.59 Down
IGF-lsR 0.34 -2.98 Down
Livin 0.37 -2.74 Down
p21 0.06 -17.60 Down
p27 0.16 -6.07 Down
sTNF-Rl 0.03 -34.29 Down
Example 21. Effect of an Extract of O. stamineus leaves Manufactured as Described in Example 1, RA and
Imatinib on the Expression of HIF-la, WNT, KDR, and COX2 Genes in Human Colorectal Tumor
[0650] This example illustrates the effect of the 28-day treatment of an extract of O. stamineus leaves manufactured as described in Example 1, RA, and imatinib, as described in Example 11, on the expression level of HIF-la, WNT, KDR and COX2 gene in tumors harvested from the mice. The genes were quantified by Real Time Polymerase Chain Reaction (RT-qPCR). Table 49 shows the forward and reverse primers used to amplify each gene. All primers were designed and synthesized by Invitrogen (Carlsbad, CA, USA). RT-qPCR experiments were performed on 7500 Fast Real-Time PCR System (Applied Biosystems®, Foster City, CA, USA) using a Superscript® III Platinum® SYBR® Green One-Step qRT-PCR Kit (Thermo Fisher Scientific Inc., USA).
Table 49. Forward and reverse primers used for the Amplification of HIF-l , WNT, KDR and COX2 genes in tumors harvested from mice treated for 28-days with an extract of O. stamineus leaves manufactured as described in Example 1, RA, and Imatinib.
[0651] Total RNA was isolated from tumor tissues using TRIpure Reagent® (Sigma-Aldrich (M), Sdn. Bhd., Malaysia). The quality and quantity of extracted RNA from tumor tissues was measured using nanodrop microvolume spectrophotometer (Thermo Fischer Scientific, USA). All samples had high concentration of RNA with a 260/230 ratio of 1.94-2.26 and a 260/280 ratio of 1.98- 2.3. The RNA was diluted to 33 ng/μί by dissolving in DEPC treated water prior to amplification by RT-q PCR. RT-qPCR was carried out in triplicate using 100 ng RNA in 3μΙ DEPC H20, 10 μΙ 2X buffer Master Mix, 1 μί RT-q PCR Mix, 0.6 μΜ of forward and reverse primers for COX-2, WNT, KDR, and β-Actin, and topped up with RNase free water to a final volume of 20 μί. For HIF-l a, the concentration of the forward and reverse primers used was at 0.3 μΜ. All components were added into 1.5 mL tubes and then transferred to a q PCR 96 well plate (Applied Biosystem, Foster, CA, USA) on ice according to the manufacturer's protocol. RNA was reverse transcribed into cDNA at 50° C for 10 minutes followed by activation of DNA polymerase enzyme at 95°C for 5 minutes. The thermal profile was established according to the manufacturer's protocol. Briefly, the amplified conditions were 40 cycles of PCR reaction in which denaturation was 10 seconds at temperature 95°C. Annealing time was 30 seconds at 60°C and elongation at 60°C for 1 minute. PCR melting curve analysis was subsequently performed for 15 seconds at 95°C, 60 seconds at 70°C and 15 seconds at 95°C.
[0652] The products of the RT-qPCR reaction were analyzed using comparative threshold cycle Ct ΔΔΏ method:
Where the AACt method = (Ct (Target sample) - Ct (Target gene sample))- (Ct (Target control) - Ct (Target gene control))
[0653] The RT-qPCR data was normalized to β-actin. The amplified samples were electrophoresed in 1.2% agarose gel containing ethidium bromide stain (0.1 μg/mL) for 80 minutes at 70 volts. The gel was then photographed under UV illumination using a transilluminator. The data are shown in Table 50. Table 50. Effect of an extract of O. stamineus leaves manufactured as described in Example 1 (E), RA, and Imatinib (I) on expression of COX-2, WNT, KDR, and HIF- tissue lysates of xenograft ectopic human colorectal tumors treated for 28-Days with the extract. Values are represented as mean ± SD, n = 3 * *p < 0.01 and ** *p < 0.001.
HIF- 14.6 10.2** 8.54*** g 2***
Example 22. Effect of an Extract of O. stamineus Leaves Manufactured as Described in Example 1, RA, and Indomethacin on Expression of Inflammatory Factors IL-1, TN F-a, and Nitric Oxide.
[0654] This example utilized U937 cells (ATCC, Rockville, USA) to evaluate the effect of an extract of O. stamineus leaves manufactured as described in Example 1, RA on the expression of the inflammatory mediators TN F-a, IL-1 and NO and the effect of the extract and the NSAIDs indomethacin, aspirin and celecoxib on the enzyme activity of COX-1 and COX-2 compared to untreated U937 cells.
[0655] U937 cells were cultured in RPMI 1640 culture medium containing 10% FBS and PS (100 IL), 50μg/mL) at a density of 2 x 104 cells/well. U937 cells, which are monocytes, were induced to differentiate into macrophages in the presence of 50 nM phorbol myristate acetate (PMA) and then cultured for 3 days at 37°C /5% C02. Cells were then collected, washed, and suspended in the culture medium. Cell viability was determined by trypan blue exclusion, which was consistently over 90% viability. The macrophages were subsequently stimulated with Salmonella abortus lipopolysaccharide (LPS) as described below and used throughout the subsequent steps.
[0656] IL-1 and TN F-a levels were evaluated using individual ELISA kits for IL-1 (Cat. No. CSB- EL01162H, CUSABIO, China) and TN F-a (CSB-E04740H, CUSABIO, China). Approximately ΙΟΟμί of differentiated calls at a density of 1-2 x 10s cells were pipetted into 96 well flat -bottom plates in the presence or absence of LPS at ^g/mL for 24hr. Next, ΙΟΟμί of media alone or media comprising the positive control indomethacin at 200μg/mL (IN-200), media comprising the extract at 25, 50, 100 and 200μg/mL (E-25, E-50, E-100, and E-200) and RA at 25, 50, 100, and 200μg/mL were added to each well. The plates were incubated at 37°C incubator under 5% C02. After 48 h incubation, the plate was centrifuged and the cells were dispensed into 96-well plates and ΙΟΟμί of supernatant from each well subjected with the same volume of ELISA reagent to evaluate NO, IL-1 and TN F-a levels using the NO, I L- 1 and TN F-a ELISA kit according to the manufacturer's instructions (CUSABIO, China). IL-1, TN F-a and NO standards were used to generate a standard curve and the concentration of I L-1, TN F-a and NO in the supernatants were measured by optical density using microplate reader at a wavelength at 550 nm. Percent inhibition of IL-1, TNF-a and NO was calculated by using the following formula:
Percentage inhibition= (1- ((As - AB) / (Ac- AB)) x 100
where, As is the absorbance of sample, AB is the absorbance of blank and Ac is the absorbance of the control. The results of the effect of the extract in comparison to the effect of indomethacin on the expression of IL-1, TN F-a, and NO is shown in Table 51.
Table 51. Dose dependent effect of an extract of O. stamineus leaves manufactured as described in Example 1 (E), RA, and Indomethacin (IN) on the expression of IL-1, TNF-a, and NO in U937 Cells. Values are expressed as% inhibition ±%SD relative to untreated U937 Cells, n= 3.
RA-100 56 ± 3.1 80 ± 2 14 ± 3
RA-200 66 ± 2.8 90 ± 1 13 ± 0
IN-200 78.3 ± 3.9 65.1 ± 3 54 ± 3
[0657] The effect of the extract on enzyme activity of COX-1 and COX-2 was assessed using an enzyme-based kit (Cat. No. 560131, Cayman, USA)). Briefly, recombinant COX-1 (ovine) and COX-2 (human recombinant) were incubated separately with two concentrations of the extract at 50 (E-50) and 200 (E-200) μg/mL at room temperature for 15 min in separate test tubes. Aspirin and celecoxib were used as standard drugs for COX1 and COX2, respectively. The reaction was started by adding 10 μί arachidonic acid to all test tubes. The tubes were incubated at 37°C in a water bath for 2 min. The reaction was then stopped by the addition of dilute hydrochloric acid (50 μί of 1 M HCI) to each test tube followed by the addition of ΙΟΟμί of saturated stannous chloride solution at 50 mg/ml (to reduce unstable reaction products such as Prostaglandin H2 to a more stable prostaglandin PGF). After incubation for 18 h, the reaction mixture from every test tube was added into the wells of a mouse anti- rabbit IgG coated microplate. Prostaglandin antiserum and prostaglandin tracer (prostaglandin antibodies linked with AChE) were added to the wells of the microplate and allowed to incubate for 60- 90 min. Thereafter, the plate was washed extensively and Ellman's reagent was added. The absorbance was measured using a microplate reader (TECAN multimode microplate reader, Infinite® M200 Pro, Switzerland) at a wavelength range from 405 nm to 420 nm. The results of the effect of the extract, aspirin and celecoxib on the enzyme activity of COX-1 and COX-2 is shown in Table 52.
Table 52. Effect of an extract of O. stamineus leaves manufactured as described in Example 1 (E), Aspirin, and Celecoxib on the enzyme activity of COX-1 and COX-2. Values are expressed as% ±%SD relative to untreated U937 Cells, n=3, ***p < 0.001, **p < 0.01, *p < 0.05.
Example 23. Antioxidant Activity of an Extract of O. stamineus Leaves Manufactured as Described in
Example 1
[0658] The antioxidant capacity of an extract of O. stamineus leaves manufactured as described in Example 1 was determined using a modification of FRAP assay as described by Firuzi et al. (302). The FRAP reagent was prepared by mixing 2.5 mL of a 10 mmol/L TPTZ solution in 40 mmol/L HCI with 2.5 mL of 20 mmol/L FeCl3 e6H20 and 25 mL of 0.3mol/L acetate buffer, pH3.6. 150μί of the freshly prepared FRAP reagent warmed to 37°C was mixed with 20 μί of the extract of Example 1 or standard
(FeS04 e7H20) and the reaction mixture incubated at 37°C for 4 min. Absorbance at 593 nm was read against methanol (blank). The data are shown in Table 53.
Table 53. Antioxidant capacity of an extract of O. stamineus leaves manufactured as described in Example 1 as determined by the FRAP assay.
E (Mg/ml Average
31.2 0.51 ± 0.03
62.5 0.56 ± 0.00
125 0.64 ± 0.02
250 0.68 ± 0.10
500 0.91 ± 0.09
1000 1.09 ± 0.08
[0659] The following calibration curve was generated based on the data in Table 53:
Y= 0.5935X + 0.5379, r2 = 0.95773
where, Y = Absorbance and X = Concentration of the extract.
[0660] The measurement of the scavenging ability of DPPH radical helps to determine the intrinsic ability of an antioxidant to donate hydrogen atom or electrons to this reactive species. The principle of this method is based on the reduction of methanolic-DPPH solution due of the presence of antioxidants having hydrogen donating DPPH radical scavenging activity. The antioxidant activity of the extract was evaluated based on the scavenging activity of the stable DPPH as described previously by Benvenuti et al. with some modification (303). First, 100 μί of 0.2 mM DPPH solution in methanol was pipette into each well of a 96-well plate. Sequential dilutions of the extract at 6.25, 12.5, 25, 50 and 100 μg/mL were made with methanol. 100 μί of each dilution of the extract or positive control was added to each well. A negative control was also used by pipetting 100 μί of methanol alone into 100 μί of DPPH and used as a blank. Vitamin C was used as a positive control. The assay was run in triplicate for each serial dilution. Next, the plate was incubated at 37°C in the dark (wrapped with aluminum foil) for 30 min to allow the reaction between the extract and reagent to occur. The DPPH radical (deep violet colour) has a maximum absorbance between 515-528 nm and is reduced to diphenyl picryl hydrazine (colourless or pale yellow colour), which does not absorb at this wavelength. The reading of the colorimetric assay was taken using a microplate reader at a wavelength of 517 nm. Each sample was measured in triplicate and results were displayed as mean ± SD, (n=3). Percentage inhibition of oxidation was calculated using the formula:
Percentage inhibition= (1- ((As - AB) / (Ac- AB)) x 100
where, As is the absorbance of sample, AB is the absorbance of blank and Ac is the absorbance of the control. The scavenging activity of the extract based on the DPPH assay is shown in Table 54.
[0661] The IC5o of the DPPH scavenging activity was calculated by the following linear regression equation based on the data in Table 54:
Y = 27.94 ln(X) - 25.42; r2 = 0.939
where Y = the free radical scavenging activity of DPPH and X = concentration of the extract. The extract inhibited the scavenging activity of the DPPH radical with an IC5o = 14.87 μg/mL.
[0662] The ABTS radical scavenging capacity assay is based on a reaction between ABTS and potassium persulfate as described by Re et al. (304) and Kara elik et al. (305). Briefly, 7 μΜ of ABTS was first dissolved in deionized water, then 2.45 μΜ of potassium persulfate was added. The reaction mixture was left to stand at room temperature overnight (12 to 16 h) in the dark before use. The mixture formed was stable for more than two days when stored in the dark at room temperature. Prior to the experiment, EtOH or PBS pH 7.4 was used to dilute the solution of ABTS»+ radical cation until an absorbance value of 0.7 at 734 nm was produced. 100 μί of the extract was added to 900 μί of ABTS
solution. The solution was vortexed for 15sec and the absorbance was recorded at 734 nm after a 6 min incubation. The assay was performed in triplicate and the absorbance was measured by a microplate reader at 734 nm. PBS without ABTS»+ was used as a control and vitamin C at different concentrations (0.41-12.5 μg/mL) was used as a standard for plotting the calibration curve of the percentage of inhibition of oxidation. The results were expressed as mg VCEAC per gram of extract. The percentage inhibition was calculated using the following formula:
Percentage inhibition= (1- ((As- AB) / (Ac AB)) X 100 where, As is the absorbance of sample, AB is the absorbance of blank and Ac is the absorbance of the control. The data is shown in Table 54.
Table 54. Antioxidant capacity of an extract of O. stamineus leaves manufactured as described in Example 1 (E) as determined by the DPPH and ABTS assay. Values are expressed as ± SD, n = 3
[0663] The data in Table 54 was used to generate the following linear regression equation for the ABTS assay:
Y = 29.33 ln(X) - 31.29; r2 = 0.959
where Y= the free radical scavenging activity of ABTS and X= concentration of the extract. The extract inhibited the scavenging free radical of ABTS with an IC5o = 15.98 ± 1.3 μg/mL. The standard reference, vitamin C, had IC50 values of 4.69 ± 0.38 and 2.6 ± 0.4 μg/mL for the DPPH and ABTS assays, respectively.
Example 24. Effect of an Extract of O. stamineus Leaves Manufactured as Described in Example 1 in
Lowering Blood Glucose Levels
[0664] The aim of this study was to evaluate the effectiveness of an extract of O. stamineus leaves manufactured as described in Example 1 in lowering blood glucose levels in Type 2 Diabetic patients using two different dosage forms comprising said extract.
[0665] Nine patients (9) who had previously been diagnosed with Type 2 diabetes for more than 1 year, had no known allergy to O. stamineus, and on oral antihyperglycemic agents as a monotherapy or in combination with insulin volunteered for this study. Patients who were also on oral lipid lowering drugs and anti-hypertensive agents were also included in the study. All patients agreed to self- administer, under patient informed consent, two (2) different dosage forms of the extract and monitor their blood glucose levels under fasting (a.m.) and random (usually in the p.m.) conditions. "Fasting" means not having anything to eat or drink (except water) for at least 8 hours before the test. The FBG test is usually done first thing in the morning, before breakfast. The random (also called "casual") blood glucose test is measured at any time of the day when the patient experiences severe diabetes symptoms. The nine (9) individuals were divided randomly into two different groups. Group A comprised
four (4) individuals who each self-administered a standardized 250 mg dose of the extract q.i.d. (total dose = 1000 mg/day) with the low dose effervescent tablet ("LDeT") manufactured as described in Example 30. Group B comprised five (5) individuals who each self-administered a standardized 300 mg dose of the extract t.i.d. (total dose = 900mg/day) with a phytosome formulation manufactured as described in Example 27. All patients agreed to provide baseline blood glucose levels as well as daily blood glucose levels under fasting (a.m.) and random (p.m.) conditions over a 7-day period. The results of this 7-day study are provided in Table 55. The effectiveness of both formulations in lowering blood glucose relative to baseline blood glucose levels are shown graphically in Fig. 8 (Note: Baseline data from patient MLY* 004 was not included in the data used for generation of the graph shown in Figure 8). Percent blood glucose lowering was determined as follows for each group of patients:
% Blood Glucose Lowering (a.m or p.m.) = ((Average Baseline Blood Glucose (a.m. or p.m.) - Average Blood Glucose (a.m. or pm))/Average Baseline Blood Glucose (a.m. or p.m.)) x 100% Table 55: Blood glucose levels in Type 2 diabetic patients before and after administration of two different formulations comprising an extract of O. stamineus leaves manufactured as described in Example 1.
Note: All patients were on lOOOmg - 2000mg metformin.
** - Blood glucose levels not recorded.
* - Patient also on insulin glargine 10-18 units daily.
X - Patient dropped out. Baseline data from this patient was not included in the determination of percent blood glucose lowering shown in Fig. 8.
# - Patient also diagnosed with stage 4 adenocarcinoma of the lung.
Example 25. Effect of an Extract of O. stamineus Leaves Manufactured as Described in Example 1 on the activity of ACE-I
[0666] The inhibitory activity of an extract of O. stamineus leaves manufactured as described in Example 1 on ACE-I can be evaluated using the method described by Shafaei et al. (123).
[0667] Shafaei et al. describe a method for evaluating the inhibitory activity towards ACE-I of macerated extracts of O. stamineus leaves using as solvents, water, 100% EtOH, 100% methanol, 50% EtOH, and 50% methanol. Sections 4.4 and 4.5 in Shafaei et al. describe the HPLC set-up and methodology for the assessment of ACE-I inhibition activity of the macerated extracts. The macerated extracts of Shafaei can be substituted with the extract according to Example 1 in determining the inhibitory activity of the extract towards ACE-I.
Example 26. Effect of an Extract of O. stamineus Leaves Manufactured as Described in Example 1 on the
Activity of AChE
[0668] The effect of an extract of O. stamineus leaves manufactured as described in Example 1 on AChE enzyme activity was measured using a 96-well microplate assay based on Ellman's method (306). The enzyme hydrolyses the substrate acetylthiocholine (ACTI) resulting in the product thiocholine which reacts with Ellman's reagent (DTNB) to produce 2-nitrobenzoate-5-mercaptothiocholine and 5-thio-2- nitrobenzoate which can be detected at 412 nm. 0.1 M phosphate buffer (PBS) pH7.8 was used as a buffer throughout the experiment unless otherwise stated. AChE (Sigma Aldrich, Germany) used in the assay was from electric eels (type Vl-S lyophilized powder, 530 U/mg protein). The enzyme stock solution (5 U/ml) was kept at -80°C. Further enzyme dilutions were done in 0.1 M PBS to 0.26 U/mL. DTNB was dissolved in DTNB buffer containing 0.1 M NaCI and 0.02 M MgCI2 to a concentration of 3 mM. ATCI was dissolved in deionized water to a concentration of 15 mM. The positive control, donepezil hydrochloride (Sigma Aldrich, Germany) (1 mM stock solution) was diluted in 0.1 M PBS to a concentration of 0.015 mM. Distilled water was used as a negative control.
[0669] The assay was conducted as follows. 140 μί of 0.1M PBS buffer pH7.8, 20 μί of different concentrations of the extract (0.3125, 0.625, 1.25, 2.5, and 5mg/ml), positive control (donepezil at 0.015 mM), and negative control (distilled water), was added to each well of a 96-well plate. Samples were read at 412 nm. This first reading served as a blank. Following this, 20 μί of AChE at 0.26 U/mL was added to each well and incubated at room temperature for 15 min. This was followed by the addition of 10 μί of 3mM DTNB and 10 μί of 15 mM ATCI to each sample containing well. After mixing, the plate was read at 412 nm for 45 min at 5 min intervals. All the reactions were performed in triplicate. The percentage inhibition was calculated as follows:
% of inhibition = (l-(Treated-Blank l)/(Untreated-Blank2)) x 100 where; Blank 1 is the sample without DTNB, and Blank 2 is the negative control without DTNB. The results of the assay are shown in Table 56.
Table 56. Effect of various concentrations of an extract of O. stamineus leaves manufactured as described in Example 1 on AChE activity. Data is presented as mean percentage inhibition ± S.D. of n = 3. Values *p < 0.05 and **p < 0.01 were considered statistically significant.
20 ND 13.56502±1.04 17.79709±1.17* 30.5213±2.11* 79.76319±5.31**
25 ND 14.1312±2.00 20.71479±2.05* 35.57489±1.9* 82.02811±9.22**
30 ND 13.27654±1.16 22.27301±2.1* 38.62456±2.07* 90.23372±8.6**
[0670] A regression curve having the following equation was generated using the values obtained at 30min:
y = 16.321X - 1.0761, r2 = 0.99
where, y =% inhibition and x = concentration in mg/ml. Based on this regression curve, the IC5o value for the extract was calculated as 3.13 mg/ml.
Example 27. Methods of Manufacturing Nano Formulations Comprising an Extract of O. stamineus Leaves
Manufactured as Described in Example 1
[0671] A. Ethosomes
[0672] As described herein, ethosomes are "soft and flexible" nano-vesicles formed from phospholipids or sophorolipids in the presence of water and EtOH (alcohol) or glycols (polyols). The size of the ethosomes is dependent on the ratio of the water to alcohol/polyol and the phospholipid or sophorolipid concentration. In one embodiment, ethosomes comprising phospholipids typically have a ratio of the extract to phospholipid of 1:6 (wt/wt). In one embodiment, ethosomes comprising sophorolipids typically have a ratio of the extract to sophorolipid of 1:2 (wt/wt).
[0673] Ethosomes comprising the extract and a phospholipid can be manufactured based on the following steps:
[0674] IE. In one embodiment, a first solution comprising cholesterol and a phosphatidylcholine in a ratio of 1:12 (wt/wt cholesterol to phosphatidylcholine) is dissolved by suitable means in an appropriate amount of chloroform in a first suitable vessel. In this instance, 100 mg of cholesterol and 1200 mg of phosphatidylcholine was dissolved in 15 ml of chloroform and dissolved by sonication at 60°C for 15 min to obtain a clear solution in a beaker. The volume of the solvent and length of sonication time will depend on the amount of phospholipid and cholesterol to be dissolved and is within the purview of the skilled person.
[0675] 2E. Generally, in one embodiment, a second solution comprising, the extract is dissolved in a mixture of EtOH and methanol by suitable means in a second suitable vessel at 50°Cfor a suitable amount of time. In one embodiment, the ratio of the EtOH to methanol is 1:2.5 (v/v) and the ratio of the EtOH/methanol mixture to extract to is 1:28.5 (vol/wt). Thus, 200 mg of the extract was dissolved in 7 ml of a solution comprising 2 ml of 100% EtOH and 5 ml of 100% methanol. The extract was dissolved by sonication using a probe sonicator for at least 15 min at 50°C in a beaker. The volume of the solvent and length of sonication time will depend on the amount of the extract to be dissolved and is within the purview of the skilled person.
[0676] 3E. In one embodiment, the first and second solutions obtained in steps IE and 2E are combined and allowed to mix to homogeneity by suitable means at 50°C for a suitable amount of time in a third suitable vessel to obtain a third solution. In this instance, the solutions from steps IE and 2E were mixed to homogeneity by sonication at 50°C for 15 min.
[0677] 4E. In one embodiment, the solvents in the third solution are evaporated by suitable means known in the art. In this instance, the solvents in the third solution obtained in step 3E were evaporated completely in a shaker incubator at 50°C, 50-100 rpm overnight to obtain a thin film.
[0678] 5E. Depending on the dosage desired, the thin film comprising the extract is dissolved in an appropriate volume of 40% EtOH for a suitable amount of time at 50°C to obtain a completely dissolved and homogenous solution. In this instance, the thin film obtained in step 4E was dissolved in 40 ml of 40% EtOH and allowed to completely dissolve to homogeneity at 50°C for 5-6 hours. The solution was allowed to come to room temperature and sonicated 3x at 5 min intervals. The time to dissolve the thin film to homogeneity will depend on the volume of extract as well as the amount of
phospholipid/cholesterol/extract in the vessel and is well within the purview of the skilled person.
[0679] 6E. Generally, the pH of the resulting solution is acidic (pH 5-6) and is neutralized with either 0.1N NaOH or triethylamine followed by the addition of a suitable amount of a pharmaceutically acceptable viscosity enhancing or emulsion stabilizing polymer. In one embodiment, the viscosity enhancing or emulsion stabilizing polymer can be a polymer of acrylic acid and polyalkenyl polyether monomers (Carbomer). In this instance, the solution obtained in step 5E was neutralized and 400 mg of carbomer (Acrypol®; Corel Pharma, Ahmedabad, Gujarat, India) was slowly added to form a viscous gel like composition. Mixing was continued for a further 2 hours to ensure thorough incorporation of the carbomer. Any air bubbles incorporated into the gel can be removed by suitable means. In this instance, the bubbles incorporated into the gel were removed by placing the beaker containing the gel in an ultrasonic bath de-gasser overnight.
[0680] The ethosome mixture is stored in a refrigerated environment until the ethosomes can be incorporated into an appropriate formulation (e.g., topical, aerosol, inhalation, or oral). The particle size of the ethosomes were 40 nm and the EtOH content of the ethosomes formed was 40% (wt/wt).
[0681] Zeta potential is a physical parameter for predicting stability of the ethosomes. Methods for determining the zeta potential are well known in the art. The zeta potential for the ethosomes manufactured according to the method described herein was -42 mV.
[0682] Ethosomes comprising the extract and a sophorolipid was manufactured based on the following steps:
[0683] IS. In one embodiment, 200mg of sophorolipid was was dissolved in 15 ml chloroform and the pH adjusted to 8 with 0.1N NaCI. The solution was then heated 60°C for 15 minutes.
[0684] 2S. The extract is prepared essentially as described in step 2E except that the ratio of EtOH/methanol mixture to extract is 1:14.3 (v/wt). Thus, 100 mg of the extract was dissolved in 7 ml of a solution comprising 2 ml of 100% EtOH and 5 ml of 100% methanol. The extract was dissolved by sonication using a probe sonicator for at least 15 min at 50°C in a beaker. The volume of the solvent and length of sonication time will depend on the amount of the extract of O. stamineus leaves to be dissolved and is within the purview of the skilled person.
[0685] 3S. The solutions from step IS and 2S were combined and mixed to homogeneity.
[0686] 4S. The solution from step 3S was next circulated in a rotary evaporator at 50°C for 3 hours to allow encapsulation of the extract into sophorolipid micelles and allow formation of a thin film and evaporation of solvents.
[0687] 5S. The resulting thin film was dissolved in 20 ml of 40% EtOH by shaking at 50°C.
[0688] 6S. 1% (w/v) acrypol was slowly added to the hydroethanolic solution from step 5S while stirring to maintain a gel formulation of the sophorolipid comprising formulation.
[0689] 7S. The formulation from step 7S was stored at 4°C for later use.
[0690] B. Phytosomes
[0691] Generally, phospholipids for use in the manufacture of phytosomes can be purchased from sources known in the art or can be purified from any suitable source known to the skilled person. The phospholipids and extract of O. stamineus leaves are combined at a ratio of 1:1 to allow encapsulation of the phytochemicals in the extract into the phospholipid micelles. Thus, if a phytosome formulation comprising 100 mg of the extract of O. stamineus leaves is desired, 100 mg of the extract will be formulated with 100 mg of the desired phospholipid to form phytosomes as described below. Similarly, for the phytosome formulation used in Example 24, 300 mg of the extract of O. stamineus leaves was combined with 300 mg of the soy lecithin to the form phytosomes as described below. The mixture comprising the micelles is then spray dried by means well known in the art to obtain a powder which can then be used to formulate into the desired dosage form. For the 300 mg dose of the extract phytosome formulation used in Example 24, the formulation was manufactured as follows.
[0692] In this instance, phospholipids from soy lecithin were purified for use in the manufacture of the phytosomes comprising the extract, as follows:
[0693] IP. A suitable amount of soy lecithin was dissolved to homogeneity in a blender with 100% EtOH in a 1:1 ratio (wt/vol).
[0694] 2P. The solution from step IP was circulated in a thin film circulator at 60°C for 2 hours to allow the phospholipids from the soy lecithin to dissolve into the EtOH.
[0695] 3P. The mixture in step 2P was cooled to room temperature and then placed in a 5°C refrigerator overnight.
[0696] 4P. The resulting pale-yellow supernatant was collected and the EtOH evaporated by any suitable means known in the art.
[0697] 5P. The resulting purified phospholipids were obtained as a pale-yellow oily mixture.
[0698] The phospholipids purified from soy lecithin as described in the above steps were then used for the manufacture of phytosomes comprising the extract as follows:
[0699] 6P. The purified phospholipids from step 5P were dissolved in a suitable volume of 10% EtOH to obtain a solution of 30% total dissolved solids.
[0700] 7P. Similarly, the extract of was dissolved in a suitable volume of 10% EtOH to obtain a solution of 30% dissolved solids.
[0701] 8P. The solutions from step 6P and 7P were combined and mixed to form a homogenous mixture at 50°C for 3 hours to allow encapsulation of the extract into the phospholipid micelles.
[0702] 9P. The mixture from step 8P was then spray dried at 150°C at a rate of 10 - 14 ml/minute.
[0703] The resulting spray dried powder is stored in the cold for later use to be formulated into an appropriate dosage form.
[0704] The efficacy of the phytosomes, and ethosomes comprising the extract formulated at various concentrations together with either a phospholipid or SL, in inhibiting neovascularization by the method described in Example 4 was compared to that of the efficacy of the extract alone in inhibiting neovascularization. Ethosomes comprising phosphatidylcholine or palm based SL were manufactured with either 50 or 100 μg/ml of the extract. Phytosomes comprising lecithin were manufactured with either 25, 50, 100, 150, 200 or 250 μg/ml of the extract. The data are shown in Tables 57 and 58.
Table 57. Effect of an extract of O. stamineus leaves manufactured as described in Example 1 formulated as ethosomes comprising either a phosphatidylcholine or palm-based sophorolipid versus unformulated extract according to Example 1 on neovascularization. Values are expressed as % inhibition of neovascularization ± %SD
relative to negative control (ethosomes minus the extract according to Example 1). n = 5, *p < 0.05, **p<0.01.
Table 58. Effect of an extract of O. stamineus leaves manufactured as described in Example 1 formulated as phytosomes comprising lecithin versus unformulated extract of Example 1 on neovascularization. Values are expressed as % inhibition of neovascularization ± %SD relative to negative control (phytosomes minus the extract according to Example 1). n = 5, *p < 0.05
[0705] In one embodiment, the efficacy of ethosomes comprising the extract formulated with SL was tested for its ability to treat melanoma. A topical formulation comprising SL and the extract at a 1:1 ratio (SL:extract) was manufactured as follows.
[0706] 100 mg of sophorolipid was dissolved in 20 ml 100% ethanol and sonicated for 15 min at 60°C. 50 mg of the extract of O. stamineus leaves manufactured as described in Example 1 was dissolved in 20 ml 100% ethanol and sonicated for 10 min at 50°C. The solution comprising the dissolved sophorolipid and the solution comprising the dissolved extract were combined and sonicated for 15 min at 50°C. The combined solution was placed in an incubator shaker overnight at 100 rpm to allow the solvent to evaporate. 10 ml of 40% ethanol was added to dissolve the resulting residue in a covered beaker by shaking in an incubator shaker at 50°C for 6 hours. The pH of the resulting solution was measured and raised to pH 8 using 0.1N NaOH. 100 mg acrypol was added slowly to the solution while stirring. The resulting formulation was stirred for 2 hrs at room temperature prior to being stored in the refrigerator for further study.
[0707] Six-week-old male BALB/c mice were housed in a specific pathogen-free environment. B16- F10 cells were harvested, washed, and suspended in PBS. 5 x 10s cells were injected subcutaneously into the right flank regions of the mice. The topical formulation was applied once a day for the period of the experiment. The mice were then checked every day for the appearance of tumor, and the sizes of the tumors were determined by taking 2 measurements with a calliper. Tumor volume was measured as described in Example 11. Three mice were included in each of the three groups. The data are presented in Table 58A.
Table 58A. Effect of an extract of O. stamineus leaves manufactured as described in Example 1 formulated as ethosomes comprising palm-based sophorolipid versus unformulated extract according to Example 1 on melonama tumor volume. Values are expressed as ± SD. n = 6, p < 0.05.
[0708] In one embodiment, the efficacy of ethosomes comprising the extract formulated with SL was tested for its ability to treat wounds in-vivo.
[0709] A topical formulation comprising SL and the extract at a 2:1 ratio (SLextract) was manufactured as follows. 100 mg of sophorolipid was dissolved in 20 ml 100% ethanol and sonicated for 15 min at 60°C. 50 mg of the extract of O. stamineus leaves manufactured as described in Example 1 was dissolved in 20 ml 100% ethanol and sonicated for 10 min at 50°C. The solution comprising the dissolved sophorolipid and the solution comprising the dissolved extract were combined and sonicated for 15 min at 50°C. The combined solution was placed in an incubator shaker overnight at 100 rpm to allow the solvent to evaporate. 10 ml of 40% ethanol was added to dissolve the resulting residue in a covered beaker by shaking in an incubator shaker at 50°C for 6 hours. The pH of the resulting solution was measured and raised to pH 8 using 0.1N NaOH. 100 mg acrypol was added slowly to the solution while stirring. The resulting formulation was stirred for 2 hrs at room temperature prior to being stored in the refrigerator for further study.
[0710] The effect of the formulation on wound healing was tested as follows. The detailed procedure for the creation of the wound and its excision of has been described by Shukla et al. (307). The topical formulation was applied once a day throughout the experiment. The surface area of the wound was measured on days 5, 8 and 13 after creation of the wound. The surface area of the wound was measured by tracing the boundary of the still open wound on semi-transparent paper and calculating the are using a graph paper. The data are presented in Table 58B. Table 58B. Effect of an extract of O. stamineus leaves manufactured as described in Example 1 formulated as ethosomes comprising palm-based sophorolipid versus unformulated extract according to Example 1 on wound healing. Values are expressed as ± SD. n = 6, p < 0.05.
Example 28. The Anti-Angiogenic and Anti-Melanoma Properties of a Nano-Formulation (Ethosome) Comprising an Extract of O. stamineus Leaves Manufactured as Described in Example 1.
[0711] The effect of an extract of O. stamineus leaves manufactured as described in Example 1 formulated into a topical gel comprising ethosomes on anti-angiogenesis and melanoma was evaluated in this example.
[0712] In this example, two differing viscosities of gel formulations comprising an extract of O. stamineus leaves were manufactured generally as follows:
[0713] 300 mg of phosphatidylcholine (from lecithin) and 25mg cholesterol were dissolved in 20 ml of ethanol and sonicated for 30 minutes at 60°C.
[0714] 50 mg of the extract was dissolved in 20 ml ethanol and sonicated for 10 min at 50°C.
[0715] The solutions in 1 and 2 were combined into one beaker and again sonicated for 15 minutes at
50°C.
[0716] The beaker from step 3 was placed on an incubator shaker at 100 rpm overnight to solvent to evaporate.
[0717] 10 ml of 40% ethanol was added to the beaker in step 4 and placed, covered, on an incubator shaker for 6 hours at 50°C.
[0718] The pH was measured and adjusted to pH 8 with 0.1N NaOH.
[0719] 100 mg of a carbomer (Acrypol®, Corel Pharma, Ahmedabad, Gujarat, India) was added pinch by pinch while stirring. 1% (wt/vol) of Acrypol® was added to the dispersion to generate a 1% gel formulation or 2% (wt/vol) Acrypol® was added to generate a 2% gel formulation.
[0720] The formulations were stirred for 2 hours in room temperature before storage at 4°C for further study.
[0721] Several ethosome formulations comprising different ratios of phosphatidylcholine from soy lecithin or from frozen eggs to the extract were prepared to determine the optimum ratio of phospholipid to extract which would maximize entrapment of the extract. Entrapment efficiency was determined as described in Example 15. As shown in Table 59, highest entrapment efficiency was achieved with phosphatidylcholine from eggs at a ratio of 6:1 (wt/wt) phosphatidylcholine to extract. Average diameter and zeta potential of the ethosomes were determined as described above or by means well known in the art.
Table 59. Efficiency of entrapment of the extract of O. stamineus leaves manufactured as described in Example 1 in ethosomes manufactured with varying ratios of phospholipid to extract. (n= 3, ****p<0.0001 for Sample 1 in comparison to Samples 2-7).
2 Phosphatidylcholine 5:1 53.67 ± 2.83 204.7 nm -30.1 mV
(eggs)
3 Phosphatidylcholine 4:1 53.06 ± 2.54 145.0 nm -32.5 mV
(eggs)
4 Phosphatidylcholine 3:1 29.04 ± 1.54 195.7 nm -35.5 mV
(eggs)
5 Phosphatidylcholine 2:1 31.96 ± 2.86 204.7 nm -38.3 mV
(eggs)
6 Phosphatidylcholine 1:1 27.62 ± 282.7 nm -59.6 mV
(eggs) 2 83****
7 Phosphatidylcholine 6:1 30.38 ± 3.09 144.3 nm -44.2 mV
(lecithin from
soybean)
[0722] Fig. 9 shows the chemical fingerprint of Formulation 1 (A) and an unformulated extract (B) as determined by HPLC using UV at 320 nm.
[0723] A skin penetration study was conducted to determine the efficiency of penetration of the extract formulated as ethosomes versus unformulated extract labelled with red fluorescent dye.
Ethosomes comprising 500 mg of the extract and equivalent weight of unformulated extract (83 mg) was applied to skin samples 1 cm in diameter obtained from hairless mice. The efficiency of penetration of the extract, as determined by measuring the amount of A that had penetrated in skin samples, was assessed by confocal laser microscopy 24hrs after application of the formulated and unformulated extract and is shown in Table 60.
Table 60. Efficiency of permeation of the formulated and unformulated extract as determined by measuring the amount of RA permeated in skin samples over a 24hr Period. (n= 3,*p<0.05, **p<0.01,***p and **** p<0.001, when permeated RA in the formulation was compared to RA permeated from the extract).
[0724] The cytotoxic effect of Formulation 1, comprising 100 μg/ml or 200 μg/ml of the extract, and 100 μg/ml and 200 μg/ml of unformulated extract, was evaluated on a mouse melanoma cell line B16-F10 (ATCC® CRL-6475™) using the MTT assay as described in Example 5. The result of this experiment is shown in Table 61.
Table 61. Cytotoxic effect on B16-F10 mouse melanoma cells of an ethosome formulation prepared according to Formulation 1 comprising 100 (FlOO) and 200 (F200) μg/ml of an extract of O. stamineus leaves manufactured as described in Example 1 compared to 100 (E100) and 200 (E200) g/ml of an unformulated extract. Values are expressed as % cell viability (mean ± SD) (n= 3, ****and **= p < 0.0001, * = p < 0.035)
SAMPLE
F200 F100 E200 E100
Cell viability % 100.38±3.7 142.35±5.8**** 119.35±4.6** 105.33±5.4
[0725] The effect of Formulation 1, comprising 50 μg/ml and 100 μg/ml of the extract on aggregation of B16-F10 cells to form solid tumors was compared to the effect of 50 μg/ml and 100 μg/ml unformulated extract and 100 μg/ml of A. The experiment was performed as described in Example 11. The results of this experiment are shown in Table 62.
Table 62. Effect of an ethosome formulation prepared according to Formulation 1 Comprising 50 (F50) and 100 (F100) μg/ml of an extract of O. stamineus leaves manufactured as described in Example 1 compared to 50 (E50) and 100 (E100) g/ml of an unformulated extract, and RA at 100 g/ml (RA100) on volume of spheroid formation by B16-F10 mouse melanoma cells. Values are presented as percentage inhibition of spheroid formation (mean ± SD), n = 3, *p < 0.05, **p<0.009.
[0726] The effectiveness of Formulation 1, comprising 25, 50, 100, 150, 200 and 250 μg/ml of an extract of O. stamineus leaves manufactured as described in Example 1, was compared to 100 and 200 μg/ml of unformulated extract on neovascularization in a rat aortic assay as described in Example 4. The results of this experiment are shown in Table 63.
Table 63. Effect of an ethosome formulation prepared according to Formulation 1 comprising various
concentrations of an extract of O. stamineus leaves manufactured as described in Example 1 on inhibition of neovascularization. Values are expressed as % inhibition of blood vessel neovascularization compared to negative control ± SEM. n=5, *p < 0.001 compared to negative control.
[0727] The effect of various concentrations of an extract of O. stamineus leaves manufactured as described in Example 1, formulated according to Formulation 1, on inhibiting growth of B16-F10 induced tumors in albino mice was compared to the unformulated extract. Approximately 1 x 106 B26-F10 cells were injected into albino mice. After 5 days, the melanomas that had formed were treated by topically applying Formulation 1 comprising 1000 (Fl), 2000 (F2), and 3000 (F3) mg/kg body weight of an extract of O. stamineus leaves manufactured a described in Example 1 and 10000 (El), 2000 (E2), and 3000 (E3) mg/kg body weight unformulated extract. The gel formulation was applied 6 times daily at 3 hr intervals.
The effect of the various formulated and unformulated extracts was monitored over 21 days. Tumor volume was measured as described in Example 11. The results of the effect of the various formulated and unformulated extracts on tumor volume are shown in Table 64.
Table 64. Effect of various concentrations of unformulated extract of O. stamineus leaves manufactured as described in Example 1 or formulated as ethosomes according to Formulation 1 on Volume (mm3) of B16-F10 mouse melanoma tumors over 21 in albino mice. Values are presented as ± SD. n = 5, *p < 0.05, **p < 0.003, ** < 0.0001 compared to Fl with El, F2 with E2, F3 with E3 at each time interval using 2 way ANNOVA.
Example 29. Wound Healing Formulation Comprising an Extract of O. stamineus Leaves Manufactured as
Described in Example 1
[0728] This example illustrates the effect of a formulation comprising the components shown in Table 65 on wound healing in-vitro and in-vivo.
Table 65. Components comprising a wound healing formulation comprising an extract of O. stamineus leaves manufactured as described in Example 1.
[0729] A scratch wound assay was conducted to investigate the effects of the formulation on the migration of HUVEC cells in-vitro as described in Example 6. The results of this experiment are shown in Fig. 10. At 50 μg/ml, the formulation closed the wound by 48 ± 3, 67 ± 4 and 82 ± 3.5% at 6, 12 and 18hrs
respectively. At 100 μ§/ιτιΙ the formulation closed the wound by 56 ± 3.5, 71 ± 2, and 95 ± 3.5% after 6, 12, and 18 hrs respectively.
[0730] The formulation was also tested for its ability to close a wound in-vivo in a wound excision experiment over at least 12 days. The results of this experiment are shown in Fig. 11. Topical application of excision wound treated with the formulation demonstrated higher percentage of wound contraction (p<0.01) compared to the control group as shown in Fig. 11. Shorter closure time and complete epithelialisation (12 days) was observed for the wound treated with the formulation. In control animals, however, the duration of healing was extended up to 25 days (data not shown). The average wound diameter in control animals was 24.78 ± 1.59, 21.61 ± 183, 19.36 ± 1.72, and 14.87 ± 0.95mm on days 0, 4, 8, and 12 respectively. In animals treated with the formulation, the average wound diameter was 24.61 ± 2.03, 12.51 ± 0.33, 5.71 ± 0.55, 0.00 ± 0.00 mm on days 0, 4, 8, and 12 respectively.
[0731] The formulation was also tested for its ability to stimulate synthesis of VEGF. The effect of the formulation on the expression of VEGF was measured using a VEGF ELISA as described in the previous examples. The cultured HUVEC cells were treated with different concentrations of the formulation. After a 24 h incubation period, the cultured supernatant was collected and the VEGF concentration determined according to the kit manufacturer's instructions. The results of the effect of the formulation on synthesis of VEGF by HUVEC cells are shown in Fig. 12.
[0732] The ability of the formulation to promote neovascularization was assessed using the rat aorta ring assay as described in Example 4. After incubating the rings for 5 days in media supplemented with the formulation at different serial concentrations of 12, 25, 50 and 100μg/mL, vessel length and density were calculated as described in Example 4. The results of the effect of the formulation on neovascularization is shown in Fig. 13.
[0733] The anti-inflammatory activity of the formulation was evaluated in a carrageenan induced rat paw assay as described by Tabana et al. (308). The results are shown in Fig. 14.
[0734] The anti-microbial activity of the formulation was determined by the disk diffusion method as described in Ahamed et al. (309). The results of the anti-microbial activity of the formulation are shown in Fig. 15.
Example 30. Method of Manufacturing Effervescent Formulations Comprising an Extract of O. stamineus
Leaves Manufactured as Described in Example 1
[0735] One embodiment comprises an effervescent formulation comprising a high dose of an extract of O. stamineus leaves manufactured as described in Example 1 in the form of an effervescent powder.
[0736] Prior to manufacturing of the effervescent dosage form, a therapeutically effective amount of the extract is first encapsulated with β-cyclodextrin at a ratio of 1:2.5 (wt/wt extract of Example 1:β- cyclodextrin) in a 30% EtOH solution. Bulk β-cyclodextrin encapsulated extract was prepared by mixing 1.9 kg of the extract of Example 1 with 4.75 kg of β-cyclodextrin in 10 L of of 30% EtOH. The mixture was thoroughly mixed in a blender for 30 min at room temperature after which the mixture was run in a thin film circulator for 3 hours at 50°C. The mixture was subsequently spray dried at 150°C at 10 - 14 ml/min in a suitable spray drier.
[0737] An effervescent powder comprising a high dose of the extract ("HDeP") was then manufactured comprising the composition of ingredients shown in Table 66 as described in the steps
below.
Table 66. Composition of an effervescent powder comprising a high dose (1000 mg) of an extract of O. stamineus leaves manufactured as described in Example 1 ("HDeP").
1. The encapsulated extract and remaining ingredients shown in Table 66 are first individually passed through a respective sieve of the size shown in Table 66 to obtain uniform size particles.
2. Sieved Neusilin® was added to the encapsulated extract and mixed to homogeneity in a cone blender for 10 minutes. The mixture was then passed through a 120 μιτι sieve.
3. Sieved sodium bicarbonate was added to the mix from step 2 and mixed to homogeneity for
10 minutes in a cone blender before passing the powder through a 420 μιτι sieve.
4. Sieved citric acid was added to the mix from step 3 and mixed to homogeneity in a cone blender for 10 minutes. This mix was then passed through a 420 μιτι sieve twice.
5. Sieved sucralose, citron and any additional suitable flavourants, such as for example, pineapple flavor was added to the sieved mix from step 4 and mixed to homogeneity in a cone blender for 15 minutes before passing through a 420 μιτι sieve.
6. The blend from step 5 is ready for sachet filling or can be compressed into a tablet.
[0738] One embodiment comprises an effervescent formulation comprising a high dose of the extract in the form of an effervescent tablet ("HDeT"). The tablet comprises two separate blends, each of which are separately compressed and subsequently compressed together to form a single tablet. The composition of the two separate blends is shown in Table 67.
Table 67. Composition of an Effervescent Tablet comprising a High Dose (1000 mg) of an Extract of O. stamineus Leaves Manufactured as Described in Example 1 "HDeT")
β-cyclodextrin encapsulated extract according to 1750 mg 120
Example 1
Sodium bicarbonate 1000 mg 420
Sucralose 30 mg 120
Citron 150 mg 420
Neusilin® (Magnesium Aluminometasilicate) 30 mg 120
[0739] The β-cyclodextrin encapsulated extract in both blends was prepared as described above except that the amount of the extract in each blend was 500 mg and the amount of β-cyclodextrin was 1250 mg, thus maintaining the wt/wt ratio of extract to β-cyclodextrin of 1:2.5 in each blend. The remaining ingredients in each blend were sieved and mixed as described above for the H DeP.
[0740] The powder from blend 1 was then compressed into a tablet at 500 psi and the powder from blend 2 was compressed into a tablet at 1500 psi. Each of the two blend compressed tablets were then compressed together at 1500 psi to form the HDeT comprising the list of ingredients listed in Table 52. All steps in the manufacturing process was carried out under a controlled humidity environment of no more than 30% relative humidity.
[0741] One embodiment comprises an effervescent formulation comprising a low dose of the extract in the form of an effervescent powder ("LDeP") comprising the composition of ingredients shown in Table 68. Table 68. Composition of an Effervescent Powder comprising a Low Dose (250 mg) of an Extract of O. stamineus Leaves Manufactured as Described in Example 1 ("LDeP").
[0742] The LDeP comprising the ingredients listed in Table 68 was manufactured as as described in steps 2 - 6 above for the manufacture of the HDeP.
[0743] One embodiment comprises an effervescent formulation comprising the extract in the form of a low dose effervescent tablet ("LDeT"). The tablet comprises two separate blends, each of which are separately compressed and subsequently compressed together to form a single tablet. The composition of the two separate blends is shown in Table 69. Table 69. Composition of an Effervescent Tablet comprising a Low Dose (250 mg) of an Extract of O. stamineus Leaves Manufactured as Described in Example 1 ("LDeT").
I Blend 1 I
Ingredients Quantity/sachet Sieve size (μιτι)
Extract according to Example 1 125 mg 120
Citric acid 913 mg 420
Sucralose 23.5mg 120
Citron 15 mg 420
Pineapple Flavour 15mg 420
Neusilin® (Magnesium Aluminometasilicate) 15 mg 120
Blend 2
Extract according to Example 1 125 mg 120
Sodium bicarbonate 800 mg 420
Sucralose 23.5 mg 120
Citron 15 mg 420
Pineapple Flavour 15mg 420
Neusilin® (Magnesium Aluminometasilicate) 15 mg 120
[0744] The LDeT comprising the ingredients listed in Table 69 was manufactured as described above for the manufacture of the HDeT.
[0745] All steps in the manufacturing process for the HDeP, HDeT, LDeP, and LDeT were carried out under a controlled humidity environment of no more than 30% relative humidity.
Example 31. Method of Manufacturing Formulations Comprising an Extract of O. stamineus Leaves Manufactured as Described in Example 1 Comprising a Soluble Polymer and/or a Poloxamer
[0746] A. Formulations Comprising an extract of O. stamineus leaves manufactured as described in Example 1 and a Soluble Polymer.
[0747] In embodiments comprising the extract of O. stamineus leaves and a soluble polymer, the ratio of the extract to the soluble polymer is 1:1 (wt/wt). The soluble polymer can be any one or a combination of the soluble polymers described hereinabove. In one embodiment, the soluble polymer is PVP. A method for manufacturing a formulation comprising PVP and an extract of O. stamineus leaves manufactured as described in Example 1 is described below:
1A. 10 gm of the extract was dissolved in 20 ml of a 30% EtOH solution to obtain a slurry. 2A. 10 gm of PVP was added to the slurry obtained in step 1A and allowed to mix for at least 20 min at room temperature.
3A. The mix obtained from step 2A was stored at -20°C for at least 3 hours.
4A. The mix from step 3A was freeze dried by methods well known in the art to obtain a powder, which can be subsequently formulated with additional pharmaceutically acceptable excipients to form an appropriate dosage form.
[0748] B. Formulations comprising an extract of O. stamineus leaves manufactured as described in Example 1 and a Poloxamer.
[0749] In embodiments comprising an extract of O. stamineus leaves manufactured as described in Example 1 and a poloxamer, the ratio of the extract to the poloxamer is 1:1 (wt/wt). The poloxamer can be any one or a combination of the poloxamers described hereinabove. In one embodiment, the poloxamer is Poloxamer 188. In another embodiment, the poloxamer is Poloxamer 407. A method for
manufacturing a formulation comprising a poloxamer and an extract of O. stamineus leaves
manufactured as described in Example 1 is described below:
IB. 10 gm of the extract was dissolved in 20 ml of a 30% EtOH solution to obtain a slurry.
2B. 10 gm of poloxamer was added to the slurry obtained in step IB and allowed to mix for at least 20 min at room temperature.
3B. The mix obtained from step 2B was stored at -20°C for at least 3 hours.
4B. The mix from step 3B was freeze dried by methods well known in the art to obtain a powder, which can be subsequently formulated with additional pharmaceutically acceptable excipients to form an appropriate dosage form.
[0750] C. Formulations comprising an extract of O. stamineus leaves manufactured as described in Example 1, a Soluble Polymer and a Poloxamer.
[0751] In embodiments comprising an extract of O. stamineus leaves manufactured as described in Example 1, a soluble polymer and a poloxamer, the ratio of the extract to the soluble polymer to the poloxamer is 2:1:1 (wt/wt/wt). The soluble polymer and poloxamer can be any one or a combination of the soluble polymers and poloxamers described hereinabove. In one embodiment, the soluble polymer is PVP, the poloxamer is Poloxamer 188 or 407. In another embodiment, the poloxamer can be a combination of Poloxamer 188 and 407. A method for manufacturing a formulation comprising a soluble polymer and poloxamer and an extract of O. stamineus leaves manufactured as described in Example 1 is described below:
1C. 10 gm of the extract was dissolved in 20 ml of a 30% EtOH solution to obtain a slurry.
2C. 5 gm of PVP and 5 gm of Poloxamer (188, 407, or combination of 188 and 407, such that the total weight of the combination is 5gm) was added to the slurry obtained in step 1C and allowed to mix for at least 20 min at room temperature.
3C. The mix obtained from step 2B was stored at -20°C for at least 3 hours.
AC. The mix from step 3C was freeze dried by methods well known in the art to obtain a powder, which can be subsequently formulated with additional pharmaceutically acceptable excipients to form an appropriate dosage form.
[0752] In embodiments comprising an extract of O. stamineus leaves manufactured as described in Example 1, a soluble polymer and 2 poloxamers, which are different from each other, the steps involved in the method of manufacturing such a formulation is as described in steps 1C-4C, except that in step 2C, an additional 5 gm of a second poloxamer is added to the slurry, such that the ratio of the extract to the soluble polymer to poloxamer 1 to poloxamer 2 is 2:1:1:1 (wt/wt/wt/wt). Thus, in one embodiment, step 2C would involve adding 5 gm of PVP, 5 gm of Poloxamer 188 and 5 gm of Poloxamer 407 to the slurry obtained in step 1C.
Example 32. Pharmacokinetics of Formulations Comprising an Extract of O. stamineus Leaves
Manufactured as Described in Example 1
[0753] In one embodiment, the bioavailability of A was evaluated in an open label, randomized, balanced, two treatment, two period, two sequence, cross over, single oral dose study in 12 healthy, adult, male human subjects under fasting conditions after administration of an effervescent tablet comprising a high dose ("HDeT") of the extract or an effervescent powder comprising a high dose ("HDeP") of the extract. The HDeT and HDeP were manufactured as described in Example 30. The
duration of the study from the check-in of period one to the last blood sample collection after period two was 24 days with a wash out period of 20 days between two periods.
[0754] Out of 12 Indian healthy adult male subjects enrolled, 11 male subjects received either HDeT or HDeP in the first period. In the second period, 11 male subjects also received either the HDeT or HDeP product, however, subjects who received HDeT in the first period, received HDeP in the second period and vice versa as per the randomization schedule. The order of receiving the HDeT or HDeP during study was determined by a randomization schedule generated using the Proc Plan procedure of SAS Version 9.2 or higher.
[0755] After an overnight fast of at least 10-hours subjects were provided a single oral dose of either HDeT or HDeP as per the randomization schedule in a sitting posture with approximately 240 ± 2 mL (for administration of HDeP, the powder was dissolved in 200 ml of water and administered to the subject, the container was rinsed with the remaining 40 ml and given to the subject to swallow) of water at ambient temperature under the supervision of trained study personnel. To ensure the subject swallowed the drug, a "mouth check" was performed by trained personnel using disposable spatula with torch light after dosing was over.
[0756] All subjects were required to fast overnight for at least 10 hours and up to 4-hours post- dose. Standard meals were served to the subjects at appropriate times during their stay in the clinical facility. Water was restricted for one hour before and two hours after dosing (except 240 ± 2 mL given during dosing of HDeP). Water was permitted ad libitum at all other times during the study. Meals and beverages during confinement were identical for both the periods.
[0757] Blood sampling points were chosen such that T could be accurately characterized for A. In addition, sampling was done up to 24.00 hours such that the plasma concentration could be measured for adequately profiling the pharmacokinetics of the product.
[0758] In each of the study periods, 36 blood samples were collected from each subject. The pre- dose (0.000 hour) blood sample (5 mL) was collected within 2 hours prior to dosing. The post-dose blood samples (5 mL) were collected at 00.17, 00.33, 00.50, 00.75, 1.00, 1.25, 1.50, 1.75, 2.00, 2.50, 3.00, 4.00, 6.00, 8.00, 12.00, 16.00 and 24.00 hours after dosing. All post dose samples were collected within ± 2 minutes. No adverse events were reported during the study period.
[0759] Blood samples were centrifuged within 30 minutes of sample collection. The plasma was separated by centrifuging the samples at 3000 rpm at 4°C for 10 minutes. The separated plasma was transferred to pre-labelled polypropylene tubes in two aliquots and stored upright in a freezer at a temperature of -20 ± 10°C. Plasma samples were subsequently transferred into the deep freezer (-70 ± 10°C).
[0760] The concentration of RA was determined from all the plasma samples received from the clinical phase using a validated LC-MS/MS method. The mean PK parameters evaluated and the corresponding results are shown in Tables 70 and 71.
Table 70: PK Parameters for All Subjects Administered with the High Dose Effervescent Tablet (HDeT) Comprising an Extract of O. stamineus Leaves Manufactured as Described in Example 1.
PK Parameters
AUC o-t Kel
Cmax AUC, Tmax Thalf
(hr)* (Hr) 1 CI_F_obs Vz_F_obs
(ng/ml) (hr)*(ng/ml) (Hr) (Hr)
(ng/ml)
N 11 11 11 11 11 11 11 11
Mean 10.1013 13.8686 60.0275 0.51 0.7297 14.90 61.3251 167.5713
SD 3.44 7.74 120.44 0.20 0.72 38.41 43.52 135.22
Min 5.6640 5.6193 7.4054 0.33 0.0053 0.30 2.3883 43.3552
Median 9.5890 10.9490 20.6286 0.50 0.6807 1.02 48.4764 118.4788
Max 17.1930 32.0600 418.7158 0.75 2.2894 129.78 135.0360 447.1467
CV% 34.06 55.83 200.64 38.57 98.27 257.78 70.96 80.69
Geometric Mean 9.6151 12.2128 24.5467 0.48 0.3121 2.22 40.7387 130.5235
Table 71: PK Parameters for all Subjects Administered with the High Dose Effervescent Powder (HDeP) Comprising an Extract of O. Stamineus Leaves Manufactured as Described in Example 1.
Example 33. Effect of an Extract of O. stamineus Leaves Manufactured as Described in Example 1 on
Amyloid-3 Induced Neurotoxicity and Neuroprotection
[0761] A human neuroblastoma SH-SY5Y cell line (ATCC No: C L-2266) used in this study. SH-SY5Y cells were cultured in DMEM medium (Gibco, Life Technologies, Carlsbad, CA) supplemented with 10%
fetal calf serum, 100 U/ml penicillin and 100 μ§/ιτ)Ι streptomycin, and maintained at 37 °C in 5% C02 incubator. To determine the neurotoxic effects of the extract of O. stamineus leaves as well as the protective effects of the extract of O. stamineus leaves against Αβ cytotoxicity, the SH-SY5Y cells were either treated with the extract at increasing concentrations of the extract of O. stamineus leaves or first pretreated with the extract of O. stamineus leaves at concentrations ranging from 9.76x10-3 to 5ng/mL for 24 hours upon which the pretreated cells were then exposed to Ιμιτι Αβ to determine its neuroprotective effect. All experiments were done in triplicates.
[0762] Cell viability was determined by a mitochondria enzyme-dependent reaction of 3 -(3,4- dimethylthiazol-2-yl)-2,5-diphenyltetrazolium bromide (MTT). In this assay, metabolic active cells deactivate the yellow tetrazolium salt MTT to purple formazan crystals. MTT assay was carried out as described previously with minor modifications. The SH-SY5Y cells, in the exponential phase were employed whereby they were seeded onto the 96 well plates (10x104 cells/well). They were left to adhere for 24 hours, and were then treated with the range of the extract of O. stamineus leaf concentrations, vehicle and Αβ (Ιμιτι) and incubated for 24 hours. After the incubation time, the cells were washed with PBS and MTT was added to each well and were incubated for 4 hours after which the MTT solution was removed and ΙΟΟμί of DMSO was added. After 10 minutes, the absorbance was recorded at 540 nm. Results were expressed as percentage of control. The extract was found to be nontoxic up to the concentration of 0.1563μg/ml with an

(Table 72) and neuroprotective at 0.0391, 0.0781 and 0.1563μg/ml of the extract against Αβ (Table 73).
Table 72. Effect of various concentrations of the extract of O. stamineus leaves (OS) manufactured as described in Example 1 on viability of SH-SY5Y cells. Values are presented as ± SD. n = 3.
Table 73. Viability of SH-SY5Y cells pretreated with various concentrations of the extract of O. stamineus (OS) leaves manufactured as described in Example 1 on Αβ induced neurotoxicity. Values are presented as ± SD. n = 3. *p <0.05; **p<0.01
0.00975 μg/m\ OS + ΙμΜ Αβ 50.90 ± 4.18
0.0195
OS + ΙμΜ Αβ 59 .44 ± 6.64
0.0391 μ /ιτιΙ OS + ΙμΜ Αβ 68.22 ± 6.10
0.0781 μ /ιτιΙ OS + ΙμΜ Αβ 84.91 ± 9.45
0.1563 μ /ιτιΙ OS + ΙμΜ Αβ 100.83 ± 16.63
[0763] The patent and non-patent references cited in this patent specification are incorporated by reference in their entireties to the extent that their disclosures are not inconsistent with the explicit teachings of this application especially the definitions.
[0764] Embodiments of the invention include:
1. An extract of O. stamineus leaves, said extract comprising, a 1:1 (vol/vol) EtOH to water extract of O. stamineus leaves comprising <0.2% (wt/wt) of the extract 3'-hydroxy-5,6,7,4'- tetramethoxyflavone and 4% to 7% (wt/wt) rosmarinic acid.
2. The extract of embodiment 1, comprising, eupatorin and sinensetin.
3. The extract of embodiment 1, wherein 3'-hydroxy-5,6,7,4'- tetramethoxyflavone in said extract is not detectable by UV using HPLC at 310 - 340 nm.
4. The extract of embodiment 1, comprising, by weight based on the total weight of the extract, 0.05% to 0.5% sinensetin, and 0.05% to 0.5% eupatorin.
5. The extract of embodiment 1, comprising by weight based on the total weight of the extract, 2% to 4% polysaccharides, 25% to 40% glycosaponins, 32% to 39 % phenolics, 6% to 7% flavonoids, and
0.3% to 0.6% phospholipids, and <14 total protein.
6. The extract of embodiment 1, comprising, by weight based on the weight of the total extract, <0.1% 3'-hydroxy-5,6,7,4'- tetramethoxyflavone.
7. An extract of O. stamineus leaves, said extract comprising, a 1:1 (vol/vol) EtOH to water extract of O. stamineus leaves comprising by weight based on the weight of the total extract, 2% to 4% polysaccharides, 25% to 40% glycosaponins, 32% to 39% phenolics, 6% to 7% flavonoids, and 0.3% to 0.6% phospholipids, and <14% total protein.
8. The extract of embodiment 7, wherein the phenolics comprises rosmarinic acid, and the flavonoids comprises eupatorin, sinensetin, and 3'-hydroxy-5,6,7,4'-tetramethoxyflavone, and wherein said 3'-hydroxy-5,6,7,4'-tetramethoxyflavone is <0.2% wt/wt of the extract.
9. The extract of embodiment 7, wherein the phenolics comprises, by weight based on the weight of the total extract, 4% to 7% rosmarinic acid, 0.05% to 0.5% sinensetin, 0.05% to 0.5% eupatorin, and <0.2% 3'-hydroxy-5,6,7,4'- tetramethoxyflavone.
10. An extract of O. stamineus leaves, said extract comprising, a 1:1 (vol/vol) EtOH to water extract of O. stamineus leaves having a chemical fingerprint on high performance liquid chromatography at 320 nm absorbance substantially similar to that shown in FIG. 1(b).
11. The extract of embodiment 10, comprising, polysaccharides, glycosaponins, phenolics, flavonoids, and phospholipids.
12. The extract of embodiment 10 comprising, rosmarinic acid, eupatorin, and sinensetin.
13. An extract as recited in one of embodiments 1-12 having an anti-angiogenic activity.
14. A method of inhibiting or downregulating angiogenesis in a subject in need thereof, said method comprising, administering to the subject a therapeutically effective amount of the extract as
recited in one of embodiments 1-12 or a formulation comprising a therapeutically effective amount of the extract as recited in one of embodiments 1-12 for modulating the expression or activity of a factor or plurality of factors such that the factor or plurality of factors inhibits or downregulates angiogenesis.
15. The method of embodiment 14, wherein said factor or plurality of factors is chosen from a pro- angiogenic factor, a growth factor, a hormone, a chemokine, an interleukin, an interferon, a lymphokine, a tumor necrosis factor, and combinations thereof.
16. A method of treating an angiogenesis associated disorder in a subject in need thereof, said method comprising, administering to the subject a therapeutically effective amount of the extract as recited in one of embodiments 1-12 or a formulation comprising a therapeutically effective amount of the extract as recited in one of embodiments 1-12 for treating the angiogenesis associated disorder.
17. A method of treating an angiogenesis associated disorder in a subject in need thereof, said method comprising, administering to the subject a therapeutically effective amount of the extract as recited in one of embodiments 1-12 or a formulation comprising a therapeutically effective amount of the extract as recited in one of embodiment 1-12, such that the extract as recited in one of claims 1-18 inhibits or downregulates the expression or activity of a factor or a plurality of factors that promotes angiogenesis.
18. The method of embodiment 17, wherein said factor or plurality of factors is a growth factor, a hormone, a chemokine, an interleukin, an interferon, a lymphokine, a tumor necrosis factor, or any combination thereof.
19. The method of embodiment 17, wherein said factor or plurality of factors is VEGF, EGF, bFGF, TGF-oc, NGFfr TNFfr IL-2, IL-7, or any combination thereof.
20. A method of treating an angiogenesis associated disorder in a subject in need thereof, said method comprising, administering to the subject a therapeutically effective amount of the extract as recited in one of embodiments 1-12 or a formulation comprising a therapeutically effective amount of the extract as recited in one of embodiments 1-12 such that the extract inhibits or downregulates expression or activity of a receptor for a factor which promotes angiogenesis.
21. The method of embodiment 20, wherein the receptor that promotes angiogenesis is a receptor for a growth factor, a hormone, a chemokine, an interleukin, an interferon, a lymphokine, a tumor necrosis factor, or any combination thereof.
22. The method of embodiment 20, wherein the receptor is a receptor for VEGF, EGF, FGF, TGFoc, NGF, TN F , IL-2, IL-7, or any combination thereof.
23. A method of treating an angiogenesis associated disorder in a subject in need thereof, said method comprising, administering to the subject a therapeutically effective amount of the extract as recited in one of embodiments 1-12 or a formulation comprising a therapeutically effective amount of the extract as recited in one of embodiments 1-12 such that the extract up-regulates the expression or activity of a factor that inhibits angiogenesis.
24. The method of embodiment 23, wherein said factor is an anti-angiogenic factor, a growth factor, a hormone, a chemokine, an interleukin, an interferon, a lymphokine, a tumor necrosis factor, or any combination thereof.
25. The method of embodiment 23, wherein said factor is GM-CSF, IFN-oc, IFN-β, or any combination thereof.
26. A method of treating an angiogenesis associated disorder in a subject in need thereof, said method comprising, administering to the subject a therapeutically effective amount of the extract as recited in one of embodiments 1-12 or a formulation comprising a therapeutically effective amount of the extract as recited in one of embodiments 1-12 such that the extract inhibits or down regulates the expression or activity of a receptor which inhibits or downregulates angiogenesis.
27. The method of embodiment 26, wherein the receptor for the factor that inhibits or downregulates angiogenesis is a receptor for a growth factor, a hormone, a chemokine, an interleukin, an interferon, a lymphokine, a tumor necrosis factor, or any combination thereof.
28. The method of embodiment 26, wherein the receptor is a receptor for GM-CSF (CD116), IFN-oc, IFN-β, or any combination thereof.
29. The method of claim 26, wherein the angiogenesis associated disorder is a tumorigenic disease, a non-tumorigenic disease, or any combination thereof.
30. The method of embodiment 29, wherein the tumorigenic disease is a solid tumor, blood-borne cancer, or any combination thereof.
31. The method of embodiment 29, wherein the tumorigenic disease is a tumor beyond 2mm in diameter, melanoma, sarcoma, adenocarcinoma, lymphoma, blastoma, skin tumor, brain tumor, leukemia, or any combination thereof.
32. A method of treating a tumorigenic disease in a subject in need thereof, said method comprising, administering to the subject a therapeutically effective amount of the extract as recited in one of embodiments 1-12 or a formulation comprising a therapeutically effective amount of the extract of one of embodiments 1-12 such that the extract downregulates expression of a gene HIF-la, WNT, KDR, COX2, or any combination thereof.
33. A method of decreasing the size of an existing capillary network in a subject in need thereof, wherein the growth and maintenance of the network depends on angiogenesis, said method comprising, administering to the subject a therapeutically effective amount of the extract as recited in any one of embodiments 1-12 or a formulation comprising a therapeutically effective amount of the extract as recited in any one of embodiments 1-12 for decreasing the size of an existing capillary network the growth and maintenance of which is dependent on angiogenesis.
34. The method of embodiment 33, wherein the capillary network is associated with a tumorigenic disease.
35. The method of embodiment 33, wherein the capillary network is associated with a non- tumorigenic disease.
36. A method of inhibiting or slowing the growth of a preexisting tumor in a subject in need thereof, said method comprising, administering to the subject a therapeutically effective amount of the extract as recited in one of embodiments 1-12 or a formulation comprising a therapeutically effective amount of the extract as recited in one of embodiments 1-12 for inhibiting or slowing the growth of the preexisting tumor.
37. A method of treating a subject diagnosed with a disease chosen from diabetes, obesity, hyperglycemia, and combinations thereof, said method comprising, administering to the subject a therapeutically effective amount of the extract as recited in one of embodiments 1-12 or a formulation comprising a therapeutically effective amount of the extract as recited in one of embodiments 1-12 for the treatment of a disease chosen from diabetes, obesity, hyperglycemia, and combinations thereof.
38. A method of maintaining a healthy blood glucose level in a subject in need thereof, said method comprising, administering to the subject a therapeutically effective amount of the extract as recited in one of embodiments 1-12 or a formulation comprising a therapeutically effective amount of the extract as recited in one of embodiments 1-12 for maintaining healthy blood glucose levels.
39. A method for reducing multidrug resistance in a subject in need thereof, said method comprising, administering to the subject a therapeutically effective amount of the extract as recited in one of embodiments 1-12 or a formulation comprising a therapeutically effective amount of the extract as recited in one of embodiments 1-12 for reducing multidrug resistance.
40. A method of treating an an angiogenesis associated disorder by reducing multidrug resistance in a subject in need thereof, said method comprising, administering to the subject a therapeutically effective amount of the extract as recited in one of embodiments 1-12 or a formulation comprising a therapeutically effective amount of the extract as recited in one of embodiments 1-12 for reducing multidrug resistance.
41. A method of enhancing sensitivity of a tumor to a chemotherapeutic agent in a subject undergoing chemotherapy, said method comprising, administering to the subject a therapeutically effective amount of the extract as recited in one of embodiments 1-12 or a formulation comprising a therapeutically effective amount of the extract as recited in one of embodiments 1-12 prior to or during chemotherapy for enhancing the sensitivity of the tumor to the chemotherapeutic agent.
42. A method of treating a tumorigenic disease in a subject in need thereof, said method comprising, administering a therapeutically effective amount of the extract as recited in one of embodiments 1-12 or a formulation comprising a therapeutically effective amount of the extract as recited in one of embodiments 1-12 as a neoadjuvant for the treatment of the tumorigenic disease.
43. A method of treating a tumorigenic disease in a subject in need thereof, said method comprising, administering a therapeutically effective amount of the extract as recited in one of embodiments 1-12 or a formulation comprising a therapeutically effective amount of the extract as recited in one of embodiments 1-12 as an adjuvant for the treatment of the tumorigenic disease.
44. A method of treating an angiogenesis associated disorder in a subject in need thereof, said method comprising administering to the subject a therapeutically effective amount of the extract as recited in one of embodiments 1-12 or a formulation comprising a therapeutically effective amount of the extract as recited in one of embodiments 1-12 in combination with at least one other therapeutic agent for the treatment of the angiogenesis associated disorder.
45. A method of of providing progression free cancer survival of a subject diagnosed with the cancer, said method comprising, administering to the subject a therapeutically effective amount of the extract as recited in one of embodiments 1-12 or a formulation comprising a therapeutically effective amount of the extract of embodiments 1-12 for the progression free survival from cancer in the subject.
46. A method of treating or ameliorating asthenia in a subject in need thereof, said method comprising administering to the subject a therapeutically effective amount of the extract as recited in one of embodiments 1-12 or a formulation comprising a therapeutically effective amount of the extract as recited in one of embodiments 1-12 for the treatment or amelioration of asthenia.
47. A formulation comprising, a therapeutically effective amount of the extract as recited in embodiments 1-12 and at least one pharmaceutically acceptable excipient.
48. The formulation of embodiment 47, wherein the formulation is an immediate release formulation.
49. The formulation of embodiment 47, wherein the formulation is a modified release dosage form.
50. The formulation of embodiment 47, wherein said formulation is a sublingual film, a sublabial film, a buccal film, a gel, a dendrimer, an oral spray, an orally disintegrating tablet, a lozenge, an effervescent tablet, sublingual drops, a lollipop, a chewing gum, a solid immediate release dosage form, a modified release dosage form, a capsule, a gelcap, a pastille, a multiparticulate, a mini tablet, a caplet, an effervescent powder, a hydrogel, a syrup, a medicated straw, a dry-powder inhaler, a nebulizer, a metered dose inhaler, a suppository, dendrimers, a catheter, a vaginal tablet, a vaginal cream, a vaginal suppository, a vaginal ring, a dermal patch, a transdermal patch, ethosomes, niosomes, discosomes, phytosomes, liposomes, a lotion, a lip balm, an ointment, a cream, an emulsion, a topical spray, a nasal spray, a medicated shampoo, eye drops, injectables, a topical emulsion, biodegradable microparticles, biodegradable microspheres, biodegradable nano-microspheres, nanoparticles, polymeric
microparticles, polymeric nanoparticles, steroidal nanoparticles, steroidal microparticles, silicon microneedles, or nanostructured lipid carriers.
51. The formulation of embodiment 47, wherein the at least one pharmaceutically acceptable excipient comprises an effervescent couple, an anti-caking agent, and a taste masking agent.
52. The formulation of embodiment 47, wherein the formulation comprises from 100 mg to 200 mg of the extract.
53. The formulation of embodiment 47, wherein the formulation comprises 250 mg of the extract.
54. The formulation of embodiment 47, wherein the formulation comprises 1000 mg of the extract.
55. A method for manufacturing an extract of O. stamineus, said method comprising: (a) contacting pulverized leaves of O. stamineus with a solvent comprising 1:1 (vol/vol) EtOH to water solution preheated to 60°C, wherein the solvent is moving in a first direction for a period of time, (b) continuing the extraction by directing the solvent in a second direction opposite to the first direction for a period of time equal to the time in (a), (c) alternating direction of solvent flow for a period of time, (d) filtering the extract through a filter, and (e) concentrating the filtered extract by evaporation of the solvent.
56. A kit comprising a suitable dosage form comprising a therapeutically effective amount of the extract of one of embodiments 1-12 in package together with instructions for the treatment of an angiogenesis associated disorder in a subject in need thereof, wherein said instructions include instructions for the administration of said dosage form.
57. A functional food comprising the extract as recited in one of embodiments 1-12.
58. A dietary supplement comprising the extract as recited in one of embodiments 1-12.
59. A cosmeceutical comprising the extract as recited in one of embodiments 1-12.
60. The extract as recited in embodiments 1-12 for inhibiting or down regulating the expression and/or activity of AChE.
61. A method of inhibiting or downregulating the expression and/or activity of AChE in a subject in need thereof, said method comprising, administering to the subject a therapeutically effective amount of the extract as recited in one of embodiments 1-12 or a formulation comprising a therapeutically effective
amount of the extract as recited in one of embodiments 1-12 for inhibiting or downregulating the expression and/or activity of AChE.
62. A method of inhibiting or downregulating the expression and/or activity of AChE in a subject in need thereof, said method comprising, administering to the subject a therapeutically effective amount of the extract as recited in one of embodiments 1-12 or a formulation comprising a therapeutically effective amount of the extract as recited in one of embodiments 1-12 in combination with another active agent which inhibits or downregulates the expression and/or activity of AChE.
63. A method of treating a neurological disorder in a subject in need thereof by inhibiting or down regulating the expression and/or activity of AChE in a subject in need thereof, said method comprising, administering to the subject a therapeutically effective amount of the extract as recited in one of embodiments 1-12 or a formulation comprising a therapeutically effective amount of the extract as recited in one of embodiments 1-12 for inhibiting or downregulating the expression and/or activity of AChE.
64. The extract as recited in embodiments 1-12 for preventing or slowing the progression of Αβ dependent or Αβ induced cell death.
65. A method of of treating a neurological and/or ophthalmic disorder by preventing or slowing the progression of Αβ dependent or Αβ induced cell death in a subject in need thereof, said method comprising administering to the subject a therapeutically effective amount of the extract as recited in one of embodiments 1-12 or a formulation comprising a therapeutically effective amount of the extract as recited in one of embodiments 1-12 for preventing Αβ dependent or Αβ induced cell death.
REFERENCES
(1) B. B. Petrovska, "Historical review of medicinal plants' usage," Pharmacognosy Review, vol. 6, no.
11, pp. 1-5, Jan-Jun 2012.
(2) Z. Shen, "Recent research and developments in traditional Chinese medicine in China," in Report of the Third Meeting of Directors of WHO Collaborating Centres for Traditional Medicine, Geneva, World Health Organization, 1996, pp. 7-13.
(3) G. Mahady, "Global harmonization of herbal health claims," The Journal of Nutrition, vol. 131, no.
3S, pp. 1120S-1123S, 2001.
(4) T. Efferth and E. Koch, "Complex Interactions between Phytochemicals. The Multi-Target
Therapeutic Concept of Phytotherapy," Current Drug Targets, vol. 12, pp. 122-132, 2011.
(5) B. Schmidt, D. Ribnicky, P. Lipsky and I. Raskin, "Revisiting the ancient concept of botanical
therapeutics," Nature Chemical Biology, vol. 3, no. 7, pp. 360-366, 2007.
(6) L. Taylor, "Plant based drugs and medicines," Raintree, 22 February 2013. (Online). Available: http://www.rain-tree.eom/plantdrugs.htm#.WG70ELEZNE4. (Accessed 5 January 2017).
(7) A. L. Hopkins, "Network pharmacology: the next paradigm in drug discovery.," Nature Chemical Biology, vol. 4, no. 11, pp. 682-690, 2008.
(8) I. Kola and J. Landis, "Can the pharmaceutical industry reduce attrition rates?," Nature Reviews Drug Discovery, vol. 3, pp. 711-716, August 2004.
(9) J. M. Gostner, O. A. Wrulich, M. Jenny, D. Fuchs and F. Ueberall, "An update on the strategies in multicomponent activity monitoring within the phytopharmaceutical field," BMC Complementary and Alternative Medicine, vol. 12, no. 18, 2012.
(10) G. Zimmermann, J. Lehar and C. Keith, "Multi-target therapeutics: when the whole is greater than the sum of the parts," Drug Discovery Today, vol. 12, no. 1-2, pp. 34-42, January 2007.
(11) J. Hartman, B. Garvik and L. Hartwell, "Principles for the Buffering of Genetic Variation," Science, vol. 291, no. 5506, pp. 1001-1004, 9 February 2001.
(12) C. Costa, J. Incio and R. Soares, "Angiogenesis and chronic inflammation: cause or consequence?," Angiogenesis, vol. 10, no. 3, pp. 149-166, 2007.
(13) T. Masuda, K. Masuda and N. Nakatani, "Orthosiphol A, a highly oxygenated diterpene from the leaves of orthosiphon stamineus.," Tetrahedron Letters, vol. 33, no. 7, pp. 945-946, 1992.
(14) S. Awale, Y. Tezuka, A. H. Banskota and S. Kadota, "Siphonols A-E: novel nitric oxide inhibitors from Orthosiphon stamineus of Indonesia.," Bioorganic & Medicinal Chemistry Letters, vol. 13, no. 1, pp. 31-35, 2003.
(15) O. Z. Ameer, I. M. Salman, M. Z. Asmawi, Z. O. Ibraheem and M. F. Yam, "Orthosiphon stamineus: traditional uses, phytochemistry, pharmacology, and toxicology.," Journal of Medicinal Food, vol. 15, no. 8, pp. 678-690, 2012.
(16) I. K. Adnyana, F. Setiawan and M. Insanu, "From ethnopharmacology to clinical study of
orthosiphon stamineus benth," International Journal of Pharmacy and Pharmaceutical Sciences, vol. 5, no. 3, pp. 66-73, 2013.
(17) K. Ghedira and P. Goetz, "Orthosiphon stamineus Benth.: orthosiphon (Lamiaceae).,"
Phytotherapie, vol. 13, no. 1, pp. 39-44, 2015.
(18) A. Matkowski, "Antioxidant Activity of Extracts and Different Solvent Fractions of Glechoma hederacea L. and Orthosiphon stamineus (Benth.) Kudo," Advances in Clinical and Experimental Medicine, vol. 17, no. 6, pp. 615-624, 2008.
(19) M. F. Yam, L. F. Ang, . Basir, I. Salman, O. Z. Ameer and M. Z. Asmawi, "Evaluation of the antipyretic potential of Orthosiphon stamineus Benth standardized extract.," Inflammopharmacology, vol. 17, no. 1, pp. 50-54, 2009.
(20) L. Perry and J. Metzger, Medicinal Plants of East and Southeast Asia: attributed properties and uses, MIT Press, 1980, p. 620.
(21) G. Akowuah, Z. Ismail, I. Norhayati and A. Sadikun, "The effects of different extraction solvents of varying polarities on polyphenols of Orthosiphon stamineus and evaluation of the free radical- scavenging activity.," Food Chemistry, vol. 93, no. 2, pp. 311-317, 2005.
(22) Y. Tezuka, P. Stampoulis, A. H. Banskota, S. Awale, K. Q. Tran, I. Saiki and S. Kadota, "Constituents of the Vietnamese medicinal plant Orthosiphon stamineus," Chemical and Pharmaceutical Bulletin, vol. 48, no. 11, pp. 1711-1719, 2000.
(23) I. M. Lyckander and K. E. Malterud, "Lipophilic flavonoids from Orthosiphon spicatus prevent oxidative inactivation of 15-lipoxygenase.," Prostaglandins, Leukotrienes and Essential Fatty Acids, vol. 54, no. 4, pp. 239-246, 1996.
(24) N. K. R. Olah, M. C. L., D. Hanganu and S. Gocan, "Phytochemical and pharmacological studies on Orthosiphon stamineus Benth. (Lamiaceae) hydroalcoholic extracts," Journal of Pharmaceutical and Biomedical Analysis, vol. 33, pp. 117-123, 2003.
(25) M. F. Yam, C. P. Lim, L. Fung Ang, L. Y. Por, S. T. Wong, M. Z. Asmawi, R. Basir and M. Ahmad, "Antioxidant and Toxicity Studies of 50% Methanolic Extract of Orthosiphon stamineus Benth," BioMed Research International, vol. 10, p. 10, 2013.
(26) G. A. Akowuah, I. Zhari, I. Norhayati, A. Sadikun and S. M. Khamsah, "Sinensetin, eupatorin,' 3- hydroxy-5, 6, 7', 4-tetramethoxyflavone and rosmarinic acid contents and antioxidative effect of Orthosiphon stamineus from Malaysia.," Food Chemistry, vol. 87, no. 4, pp. 559-566, 2004.
(27) P. G. Pietta, P. L. Mauri, C. Gardana and A. Bruno, "High-performance liquid chromatography with diode-array ultraviolet detection of methoxylated flavones in Orthosiphon leaves," Journal of Chromatography A, vol. 547, pp. 439-442, 1991.
(28) Y. Takeda, T. Matsumoto, H. Terao, T. Shingu, Y. Futatsuishi, T. Nohara and T. Kajimoto,
"Orthosiphol D and E, minor diterpenes from Orthosiphon stamineus," Phytochemistry, vol. 33, no. 2, pp. 411-415, 1993.
(29) Y. H. Loon, J. W. Wong, S. P. Yap and K. H. Yuen, "Determination of flavonoids from Orthosiphon stamineus in plasma using a simple HPLC method with ultraviolet detection.," Journal of chromatography B, vol. 816, no. 1-2, pp. 161-166, 2005.
(30) M. A. Hossain, Z. Ismail, A. Rahman and S. C. Kang, "Chemical composition and anti-fungal
properties of the essential oils and crude extracts of Orthosiphon stamineus Benth.," Industrial Crops & Products, vol. 27, no. 3, pp. 328-334, 2008.
(31) M. Singh, B. Gidwani, A. Gupta, H. Dhongade, P. Kashyap and D. Tripathi, "A Review of the
Medicinal Plants of Genus Orthosiphon (Lamiaceae)," International Journal of Biological
Chemistry, vol. 9, no. 6, pp. 318-331, 2015.
(32) I. Doleckova, L. Rarova, J. Griiz, M. Vondrusova, M. Strnad and V. Krystof, "Antiproliferative and antiangiogenic effects of flavone eupatorin, an active constituent of chloroform extract of Orthosiphon stamineus leaves," Fitoterapia, vol. 83, no. 6, pp. 1000-1007, 2012.
(33) M. Ahamed, A. Aisha, Z. Nassar, J. Siddiqui, Z. Ismail, S. Omari, C. Parish and A. Majid, "Cat's Whiskers Tea (Orthosiphon Stamineus) Extract Inhibits Growth of Colon Tumor in Nude Mice and Angiogenesis in Endothelial Cells via Suppressing VEGFR Phosphorylation," Nutrition and Cancer, vol. 64, no. 1, pp. 89-99, 2012.
(34) M. Yam, V. Lim, I. Salman, O. Ameer, L. Ang, N. Rosidah, M. Abdulkarim, G. Abdullah, R. Basir, A.
Sadikun and M. Asmawi, "HPLC and Anti-Inflammatory Studies of the Flavonoid Rich Chloroform Extract Fraction of Orthosiphon Stamineus Leaves," Molecules, vol. 15, no. 6, pp. 4452-4466, 2010.
(35) M. Siddiqui and Z. Ismail, "Simultaneous Analysis of Bioactive Markers from Orthosiphon
Stamineus Benth Leaves Extracts by Reverse Phase High Performance Liquid Chromatography," Tropical Journal of Pharmaceutical Research, vol. 10, no. 1, pp. 97-103, 2011.
(36) M. Laavola, R. Nieminen, M. Yam, A. Sadikun, A. M. R. Basir, J. Welling, H. Vapaatalo, R. Korhonen and E. Moilanen, "Flavonoids Eupatorin and Sinensetin Present in Orthosiphon stamineus Leaves Inhibit Inflammatory Gene Expression and STAT1 Activation," Planta Med, vol. 78, no. 8, pp. 779- 786, 2012.
(37) R. Nijveldt, E. van Nood, D. E. van Hoorn, P. Boelens, K. van Norren and P. A. van Leeuwen,
"Flavonoids: a review of probable mechanisms of action and potential applications," Am J Clin Nutr, vol. 74, no. 4, pp. 418-425, 2001.
(38) N. Chandel and D. Tuveson, "The Promise and Perils of Antioxidants for Cancer Patients," N Engl J Med, vol. 371, no. 2, pp. 177-178, 2014.
(39) I. Majewska and E. Gendaszewska-Darmach, "Proangiogenic activity of plant extracts in
accelerating wound healing— a new face of old phytomedicines," Acta Biochim Pol., vol. 58, no. 4, pp. 449-460, 2011.
(40) T.-P. Fan, J.-C. Yeh, K. Leung, P. Yue and R. Wong, "Angiogenesis: from plants to blood vessels," TRENDS in Pharmacological Sciences, vol. 27, no. 6, pp. 297-309, 2006.
(41) K. Paavonen, P. Puolakkainen, L. Jussila, T. Jahkola and K. Alitalo, "Vascular endothelial growth factor receptor-3 in lymphan- giogenesis in wound healing," American Journal of Pathology, vol. 156, no. 5, pp. 1499-1504, 2000.
(42) D. Ruiter, R. Schlingemann, J. Westphal, M. Denijn, F. Rietveld and R. De Waal, "Angiogenesis in wound healing and tumor metastasis," Behring Inst. Mitt., vol. 92, pp. 258-272, 1993.
(43) K. Yano, L. Brown and M. Detmar, "Control of hair growth and follicle size by VEGF-mediated angiogenesis," Journal of Clinical Investigation, vol. 107, no. 4, pp. 409-417, 2001.
(44) N. Ferrara, H. Chen, T. Davis-Smyth, H. Gerber, T. Nguyen, D. Peers, V. Chisholm, K. Hillan and R.
Schwall, "Vascular endothelial growth factor is essential for corpus luteum angiogenesis," Nature Medicine, vol. 4, no. 3, pp. 336-340, 1998.
(45) E. Conway, D. Collen and P. Carmeliet, "Molecular mechanisms of blood vessel growth,"
Cardiovascular Research, vol. 49, no. 3, pp. 507-521, 2001.
(46) D. Hanahan and J. Folkman, "Patterns and emerging mechanisms of the angiogenic switch during tumorigenesis," Cell, vol. 86, no. 3, pp. 353-364, 1996.
(47) T. Tonini, F. Rossi and P. Claudio, "Molecular basis of angiogenesis and cancer," Oncogene, vol. 22, no. 42, pp. 6549-6556, 2003.
(48) I. Arnaoutova and H. Kleinman, "In vitro angiogenesis: endothelial cell tube formation on gelled basement membrane extract," Nature Protocols, vol. 5, no. 4, pp. 628-635, 2010.
K. L. DeCicco-Skinner, G. H. Henry, C. Cataisson, T. Tabib, J. C. Gwilliam, N. J. Watson, E. Bullwinkle, L. Falkenburg, . O'Neill, A. Morin and J. S. Wiest, "Endothelial cell tube formation assay for the in vitro study of angiogenesis," Journal of Visualized Experiments, vol. 91, p. e51312, 2014.
R. Sutherland, J. McCredie and W. Inch, "Growth of Multicell Spheroids in Tissue Culture as a Model of Nodular Carcinomas," J Natl Cancer Inst, vol. 46, no. 1, pp. 113-120, 1971.
G. Hamilton, "Multicellular spheroids as an in vitro tumor model," Cancer Lett., vol. 131, no. 1, pp. 29-34, 1998.
H. Ma, Q. Jiang, S. Han, Y. Wu, T. J. Cui, D. Wang, Y. Gan, G. Zou and X. Liang, "Multicellular tumor spheroids as an in vivo-like tumor model for three-dimensional imaging of chemotherapeutic and nano material cellular penetration.," Mol Imaging, vol. 11, no. 6, pp. 487-498, 2012.
C. Morton and H. P.J., "Establishment of human tumor xenografts in immunodeficient mice," Nature Protocols, vol. 2, no. 2, pp. 247-250, 2007.
S. Goel, D. Duda, L. Xu, L. Munn, Y. Boucher, D. Fukumura and R. Jain, "Normalization of the vasculature for treatment of cancer and other diseases," Physiol Rev., vol. 91, no. 3, pp. 1071- 1121, 2011.
W. Hart, M. Goldbaum, B. Cote, P. Kube and M. Nelson, "Measurement and classification of retinal vascular tortuosity," Int J Med Inform, vol. 53, no. 2-3, pp. 239-252, 1999.
H.-C. Han, "Twisted Blood Vessels: Symptoms, Etiology and Biomechanical Mechanisms," 7 Vadc Res, vol. 48, pp. 185-197, 2012.
C. Cheung, C. Y. L. Cheung, E. Y. Liu, P. Mitchell, J. Wang, H. Hamzah, A. Tin and T. Wong, "Retinal Vascular Tortuosity and Age-Related Macular Degeneration: The Singapore Malay Study," Investigative Ophthalmology & Visual Science, vol. 51, p. 4544, 2010.
X. Zhao, H. Si and P. Xu, "Protective Effects of 5,7,3',4'-Tetramethoxyflavone on Proliferation of Rat Chondrocytes Induced by IL-Ιβ," Advanced Materials Research, Vols. 998-999, pp. 287-290, 2014.
J. Ma, J. Wang, W. Fan, X. Pu, D. Zhang, C. Fan, L. Xiong, H. Zhu, N. Xu, R. Chen and S. Liu, "Upregulated TIMP-1 correlates with poor prognosis of laryngeal squamous cell carcinoma," Int. J. Clin. Exp. Patho., vol. 7, no. 1, pp. 246-254, 2014.
A. Tarhini, Y. Lin, O. Yeku, W. LaFramboise, M. Ashraf and C. S. L. a. J. M. K. Sander, "A four-marker signature of TNF-RII, TGF-ct, TIMP-1 and CRP is prognostic of worse survival in high-risk surgically resected melanoma," Journal of Translational Medicine, vol. 12, no. 19, 2014.
M. Benej, S. Pastorekova and J. Pastorek, "Carbonic Anhydrase IX: Regulation and Role in Cancer," in Carbonic Anhydrase: Mechanism, Regulation, Links to Disease, and Industrial Applications, Subcellular Biochemistry 75,, vol. 75, S. Frost and R. McKenna, Eds., Springer Science, 2014, pp. 199-219.
G. Wang, B. Jiang, E. Rue and G. Semenza, "Hypoxia-inducible factor 1 is a basic-helix-loop-helix- PAS heterodimer regulated by cellular 02 tension.," Proc Natl Acad Sci USA., vol. 92, no. 12, pp. 5510-5514, 1995.
P. Swietach, R. Vaughan-Jones and A. Harris, "Regulation of tumor pH and the role of carbonic anhydrase 9," Cancer Metastasis Rev, vol. 26, pp. 299-310, 2007.
V. Ling, "Multidrug resistance: molecular mechanisms and clincial relevance," Cnacer Chemother Pharmacol, vol. 40 (Suppl), pp. S3-S8, 1997.
R. Januchowski, K. Wojtowicz, P. Sujka-Kordowska, M. Andrzejewska and M. Zabel, "MDR Gene Expression Analysis of Six Drug-Resistant Ovarian Cancer Cell Lines," BioMed Research
International, p. 10, 2013.
(66) D. Keppler, "Multidrug resistance proteins (MRPs, ABCCs): importance for pathophysiology and drug therapy," in Drug Transporters, Handbook of Experimental Pharmacology , vol. 201, M. Fromm and R. Kim, Eds., 2011, pp. 299-323.
(67) E. Leslie, R. Deeley and S. Cole, "Multidrug resistance proteins: role of P-glycoprotein, MRP1, MRP2, and BCRP (ABCG2) in tissue defense," Toxicology and Applied Pharmacology, vol. 204, no. 3, pp. 216-237, 2005.
(68) F. Russel, J. Koenderink and R. Masereeuw, "Multidrug resistance protein 4 (MRP4/ABCC4): a versatile efflux transporter for drugs and signalling molecules," Trends in Pharmacological Sciences, vol. 29, no. 4, pp. 200-207, 2008.
(69) C. Marzolini, E. Paus, T. Buclin and R. Kim, "Polymorphisms in human MDR1 (P-glycoprotein):
Recent advances and clinical relevance," Clinical Pharmacology & Therapeutics, vol. 75, no. 1, pp. 13-33, 2004.
(70) C.-H. Heldin, B. Lu, R. Evans and J. Gutkind, "Cold Spring Harb Perspect Biol doi:
10.1101/cshperspect.a005900," in Signal Transduction. Principles, Pathways, and Processes, L. Cantley, T. Hunter, R. Sever and J. Thorner, Eds., Cold Spring Harbor, NY: Cold Spring Harbor Laboratory Press, 2014, pp. 1-29.
(71) N. Parmalee and J. Kitajewski, "Wnt Signaling in Angiogenesis," Curr Drug Targets, vol. 9, no. 7, pp.
558-564, 2008.
(72) K. Holmes, O. Roberts, A. Thomas and M. Cross, "Vascular endothelial growth factor receptor-2: structure, function, intracellular signalling and therapeutic inhibition," Cellular Signalling, vol. 19, no. 10, pp. 2003-2012, 2007.
(73) K. B. G. Plate, B. Millauer, A. Ullrich and W. Risau, "Up-regulation of vascular endothelial growth factor and its cognate receptors in a rat glioma model of tumor angiogenesis.," Cancer Research, vol. 53, no. 23, pp. 5822-5827, 1993.
(74) C. Holland, K. Day, A. Evans and S. Smith, "Expression of the VEGF and angiopoietin genes in
endometrial atypical hyperplasia and endometrial cancer," British Journal of Cancer, vol. 89, pp. 891-898, 2003.
(75) E. Fournier, D. Birnbaum and J. Borg, "Receptors for factors of the VEGF (Vascular Endothelial Growth Family)," Bull. Cancer, vol. 84, no. 4, pp. 397-405, 1997.
(76) C. Costa, R. Soares, J. Reis-Filho, D. Leitao, I. Amendoeira and F. Schmitt, "Cyclo-oxygenase 2
expression is associated with angiogenesis and lymph node metastasis in human breast cancer," Journal of Clinical Pathology, vol. 55, no. 6, pp. 429-434, 2002.
(77) A. Tatsuguchi, K. Matsui, Y. Shinji, K. Gudis, T. Tsukui, T. Kishida, Y. Fukuda, Y. Sugisaki, A.
Tokunaga, T. Tajiri and C. Sakamoto, "Cyclooxygenase-2 Expression Correlates With Angiogenesis and Apoptosis in Gastric Cancer Tissue," Human Pathology, vol. 35, no. 4, pp. 488-495, 2004.
(78) U. Fiedler and H. Augustin, "Angiopoietins: a link between angiogenesis and inflammation,"
TRENDS in Immunology, vol. 27, no. 12, pp. 552-558, 2006.
(79) J. Jackson, M. Seed, C. Kircher, D. Willoughby and J. Winkler, "The codependence of angiogenesis and chronic inflammation.," FASEB Journal, vol. 11, no. 6, pp. 457-465, 1997.
(80) L. Coussens and Z. Werb, "Inflammation and cancer," Nature, vol. 420, no. 6917, pp. 860-867, 2002.
(81) D. Hanahan and R. A. Weinberg, "Hallmarks of cancer: the next generation," Cell, vol. 144, no. 5, pp. 646-674, 2011.
(82) E. Flossmann, P. Rothwell, B. D. A. Trial and U.-T. A. Trial, "Effect of aspirin on long-term risk of colorectal cancer: consistent evidence from randomised and observational studies," Lancet, vol. 369, no. 9573, pp. 1603-1613, 2007.
(83) A. Chan, S. Ogino and C. Fuchs, "Aspirin and the Risk of Colorectal Cancer in Relation to the
Expression of COX-2," New England Journal of Medicine, vol. 356, no. 21, pp. 2131-2142, 2007.
(84) M. Bradley, C. Hughes, M. Cantwell, G. Napolitano and L. Murray, "Non-steroidal antiinflammatory drugs and pancreatic cancer risk: a nested case-control study," Br. J. Cancer, vol. 102, pp. 1415-1421, 2010.
(85) J. Brown and R. DuBois, "COX-2: A Molecular Target for Colorectal Cancer Prevention," J. Clin.
Oncol., vol. 23, no. 12, pp. 2840-2855, 2005.
(86) Y. Sun, X. Tang, E. Half, M. Kuo and F. Sinicrope, "Cyclooxygenase-2 Overexpression Reduces Apoptotic Susceptibility by Inhibiting the Cytochrome c-dependent Apoptotic Pathway in Human Colon Cancer Cellsl," Cancer Res., vol. 62, no. 21, pp. 6323-6328, 2002.
(87) H. Sies, "Oxidative stress: oxidants and anti-oxidants," Exp. Physiol., vol. 82, no. 2, pp. 291-296, 1997.
(88) N. Temple, "Anti-oxidants and disease: More questions than answers," Nutrition Research, vol. 20, no. 3, pp. 449-459, 2000.
(89) I. Urquiaga and F. Leighton, "Plant polyphenol anti-oxidants and oxidative stress," Biological Research, vol. 33, no. 2, pp. 55-64, 2000.
(90) B. Halliwell, "Anti-oxidants in human health and disease," Annu. Rev. Nutr., vol. 16, pp. 33-50, 1996.
(91) B. Poljsak and D. M. I. Suput, "Achieving the Balance between ROS and Anti-oxidants: When to Use the Synthetic Anti-oxidants," Oxidative Medicine and Cellular Longevity, vol. 11, p. 11, 2013.
(92) N. Rao, K. Bethala, S. Sisinthy and K. Rajeswari, " Antidiabetic activity of Orthosiphon stamineus bench roots in streptozotocin induced type 2 diabetic rats," Asian Journal of Pharmaceutical and Clinical research, vol. 7, no. 1, pp. 149-153, 2014.
(93) E. Mohamed, M. Yam, L. Ang and A. A. M. Mohamed, "Antidiabetic properties and mechanism of action of Orthosiphon stamineus Benth bioactive sub-fraction in streptozotocin-induced diabetic rats," Journal of Acupuncture and Meridian Studies, vol. 6, no. 1, pp. 31-40, 2013.
(94) E. Mohamed, A. Mohamed, M. Asmawi, A. Sadikun and O. Ebrika, "Antihyperglycemic Effect of Orthosiphon Stamineus Benth Leaves Extract and Its Bioassay-Guided Fractions," Molecules, vol. 16, no. 5, pp. 3787-3801, 2011.
(95) K. Sriplang, S. Adisakwattana, A. Rungsipipat and S. Yibchok-anun, "Effects of Orthosiphon
stamineus aqueous extract on plasma glucose concentration and lipid profile in normal and streptozotocin-induced diabetic rats," Journal of Ethnopharmacology, vol. 109, no. 3, pp. 510-514, 2007.
(96) P. Kearney, M. Whelton, K. Reynolds, P. Muntner, P. Whelton and J. He, "Global burden of
hypertension: Analysis of worldwide data," The Lancet, vol. 365, no. 9455, pp. 217-223, 2005.
(97) R. Hartmann and H. Meisel, "Food-derived peptides with biological activity: From research to food applications.," Curr. Opin. Biotechnol., vol. 18, no. 2, pp. 163-169, 2007.
(98) B. Mittal and A. Singh, "Hypertension in the developing world: Challenges and opportunities," Am.
J. Kidney Dis, vol. 55, no. 3, pp. 590-598, 2010.
(99) D. Coates, "The angiotensin converting enzyme (ACE)," The International Journal of Biochemistry & Cell Biology, vol. 35, no. 6, pp. 769-773, 2003.
(100) N. Al Shukor, J. Van Camp, G. Gonzales, D. Staljanssens, K. Struijs, M. Zotti, K. Raes and G.
Smagghe, "Angiotensin-converting enzyme inhibitory effects by plant phenolic compounds: A study of structure activity relationships," J. Agric. Food Chem., vol. 61, no. 48, pp. 11832-11839, 2013.
(101) M. Pfeffer and E. Frohlich, "Improvements in clinical outcomes with the use of angiotensin- converting enzyme inhibitors: Cross-fertilization between clinical and basic investigation," American Journal of Physiology-Heart and Circulatory Physiology, vol. 291, no. 5, pp. H2021- H2025, 2006.
(102) Z. Israili and W. Hall, "Cough and angioneurotic edema associated with angiotensin-converting enzyme inhibitor therapy: A review of the literature and pathophysiology," Ann. Intern. Med., vol. 117, no. 3, pp. 234-242, 1992.
(103) L. Opie, "Ace inhibitors in pregnancy: How to avoid the sting in the tail," South African Medical Journal, vol. 86, no. 4, pp. 326-327, 1996.
(104) U. Nyman, P. Joshi, L. Madsen, T. Pedersen, M. Pinstrup, S. Rajasekharan, V. George and P.
Pushpangadan, "Ethnomedical information and in vitro screening for angiotensin-converting enzyme inhibition of plants utilized as traditional medicines in gujarat, rajasthan and kerala (india)," 7. Ethnopharmacol., vol. 60, no. 3, pp. 247-263, 1998.
(105) P. -J. Park, J.-Y. Je and S.-K. Kim, "Angiotensin i converting enzyme (ace) inhibitory activity of
hetero-chitooligosaccharides prepared from partially different deacetylated chitosans," J. Agric. Food Chem., vol. 51, no. 17, pp. 4930-4934, 2003.
(106) B. Heran, M. Wong, I. Heran and J. .. T. C. L. 2. Wright, "Blood pressure lowering efficacy of
angiotensin converting enzyme (ace) inhibitors for primary hypertension," The Cochrane database of systematic reviews, vol. 4, p. CD003823, 2008.
(107) C. Cinq-Mars and E. Li-Chan, "Optimizing angiotensin i-converting enzyme inhibitory activity of pacific hake (merluccius productus) fillet hydrolysate using response surface methodology and ultrafiltration," / Agric. Food Chem., vol. 55, no. 23, pp. 9380-9388, 2007.
(108) L. Vercruysse, J. Van Camp and G. Smagghe, "Ace inhibitory peptides derived from enzymatic hydrolysates of animal muscle protein: A review.," J. Agric. Food Chem., vol. 53, no. 21, pp. 8106- 8115, 2005.
(109) L. Somova, A. Nadar, P. Rammanan and F. Shode, "Cardiovascular, antihyperlipidemic and
antioxidant effects of oleanolic and ursolic acids in experimental hypertension," Phytomedicine, vol. 10, no. 2, pp. 115-121, 2003.
(110) L. Guerrero, J. Castillo, M. Quifiones, S. Garcia-Vallve, L. Arola, G. Pujadas and B. Muguerza,
"Inhibition of angiotensin-converting enzyme activity by flavonoids: Structure-activity relationship studies.," PLoS One, vol. 7, no. 11, p. e49493, 2012.
(111) J. Dong, X. Xu, Y. Liang, R. Head and L. Bennett, "Inhibition of angiotensin converting enzyme (ace) activity by polyphenols from tea (camellia sinensis) and links to processing method," Food Fund., vol. 2, no. 6, pp. 310-319, 2011.
(112) D. Ojeda, E. Jimenez-Ferrer, A. Zamilpa, A. Herrera-Arellano, J. Tortoriello and L. Alvarez,
"Inhibition of angiotensin convertin enzyme (ace) activity by the anthocyanins delphinidin-and cyanidin-3-o-sambubiosides from hibiscus sabdariffa," J. Ethnopharmacol., vol. 127, no. 1, pp. 7- 10, 2010.
(113) M. Loizzo, A. Said, R. Tundis, K. Rashed, G. Statti, A. Hufner and F. Menichini, " Inhibition of
angiotensin converting enzyme (ace) by flavonoids isolated from ailanthus excelsa
(roxb)(simaroubaceae)," Phytother. Res, vol. 21, no. 1, pp. 32-36, 2007.
(114) L. Hackl, G. Cuttle, S. Sanches Dovichi, M. Lima-Landman and M. Nicolau, "Inhibition of angiotensin-converting enzyme by quercetin alters the vascular response to bradykinin and angiotensin I," Pharmacology, vol. 65, no. 4, pp. 182-186, 2002.
(115) M. Alam, C. Sernia and L. Brown, "Ferulic acid improves cardiovascular and kidney structure and function in hypertensive rats," . Cardiovasc. Pharmacol., vol. 61, no. 3, pp. 240-249, 2013.
(116) L. Actis-Goretta, J. Ottaviani, C. Keen and C. Fraga, "Inhibition of angiotensin converting enzyme (ACE) activity by flavan-3-ols and procyanidins," FEBS Lett, vol. 555, no. 3, pp. 597-600, 2003.
(117) E.-K. Kwon, D.-Y. Lee, H. Lee, D.-O. Kim, N.-l. Baek, Y.-E. Kim and H.-Y. Kim, "Flavonoids from the buds of rosa damascena inhibit the activity of 3-hydroxy-3-methylglutaryl-coenzyme a reductase and angiotensin l-converting enzyme," 7. Agric. Food Chem., vol. 58, no. 2, pp. 882-886, 2009.
(118) H. Bormann and M. Melzig, "Inhibition of metallopeptidases by flavonoids and related
compounds," Die Pharmazie, vol. 55, no. 2, pp. 129-132, 2000.
(119) A. Junior, F. Gasparotto, E. Louren o, S. Crestani, 3. M. 34, M. Salvador, J. da Silva-Santos, M.
Marques and C. Kassuya, "Antihypertensive effects of isoquercitrin and extracts from tropaeolum majus I.: Evidence for the inhibition of angiotensin converting enzyme," 7. Ethnopharmacol., vol. 134, no. 2, pp. 363-372, 2011.
(120) B. Balasuriya and H. Rupasinghe, "Plant flavonoids as angiotensin converting enzyme inhibitors in regulation of hypertension," Functional Foods in Health and Disease, vol. 1, no. 5, pp. 172-188, 2011.
(121) M. Quifiones, D. Sanchez, B. Muguerza, M. Miguel and A. Aleixandre, "Mechanisms for
antihypertensive effect of cocoanox, a polyphenol-rich cocoa powder, in spontaneously hypertensive rats," Food Res. Int., vol. 44, no. 5, pp. 1203-1208, 2011.
(122) N. Azizan, R. Ahmad, K. Mohamed, M. Ahmad and Z. Asmawi, "The in vivo antihypertensive
effects of standardized methanol extracts of Orthosiphon stamineus on spontaneous hypertensive rats: A preliminary study," African Journal of Pharmacy and Pharmacology, vol. 6, no. 6, pp. 376-379, 2012.
(123) A. Shafaei, M. Sultan Khan, A. F. A. Aisha, A. Abdul Majid, M. Hamdan, M. Mordi and Z. Ismail, "Flavonoids-Rich Orthosiphon stamineus Extract as New Candidate for Angiotensin l-Converting Enzyme Inhibition: A Molecular Docking Study," Molecules, vol. 21, no. 11, p. 1500, 2016.
(124) U. Holzgrabe, P. Kapkova, V. Alptuzun, J. Scheiber and K. E., "Targeting acetylcholinesterase to treat neurodegeneration," Expert Opin. Ther. Targets, vol. 11, no. 2, pp. 161-179, 2007.
(125) M. Mehta, A. Adem and M. Sabbagh, "New Acetylcholinesterase Inhibitors for Alzheimer's
Disease," International Journal of Alzheimer's Disease, vol. Article ID 728983, p. 8, 2012.
(126) P. Anand and B. Singh, "A review on cholinesterase inhibitors for Alzheimer's disease," Arch.
Pharm. Res., vol. 36, no. 4, pp. 375-399, 2013.
(127) P. Mukherjee, V. Kumar, M. Mai and P. Houghton, "Acetylcholinesterase inhibitors from plants," Phytomedicine, vol. 14, no. 4, pp. 289-300, 2007.
(128) A. Murray, M. Faraoni, M. Castro, N. Alza and V. Cavallaroa, "Natural AChE Inhibitors from Plants and their Contribution to Alzheimer's Disease Therapy," Curr Neuropharmacol., vol. 11, no. 4, pp. 388-413, 2013.
(129) N. Suganthy, S. Pandian and K. Devi, "Cholinesterase Inhibitors from Plants: Possible Treatment Strategy for Neurological Disorders - A Review," International Journal of Biomedical and
Pharmaceutical Sciences, vol. 3, no. Special Issue 1, pp. 87-103, 2009.
(130) S. Rius-Pereza, A. Tormosa, S. Pereza and R. Talens-Viscontib, "Vascular pathology: Cause or effect in Alzheimer disease?," Neurologia, vol. 33, no. 2, pp. 112-120, 2018.
(131) W. Jefferies, K. Price, K. Biron, F. Fenninger, C. Pfeifer and D. Dickstein, "Adjusting the compass: new insights into the role of angiogenesis in Alzheimer's disease," Alzheimer's Research & Therapy, vol. 5, p. 64, 2013.
(132) C. Singh, C. Pfeifer and W. Jefferies, Pathogenic Angiogenic Mechanisms in Alzheimer's, D.
Simionescu and A. Simionescu, Eds., London: Intech Open Limited, 2017, pp. 93-110.
(133) K. Biron, D. Dickstein, R. Gopaul and W. Jefferies, "Amyloid Triggers Extensive Cerebral
Angiogenesis Causing Blood Brain Barrier Permeability and Hypervascularity in Alzheimer's Disease," PLoS ONE, vol. 6, no. 8, p. e23789, 2011.
(134) W.-J. HUANG, X. ZHANG and W.-W. CHEN, "Role of oxidative stress in Alzheimer's disease,"
Biomed. Rep., vol. 4, no. 5, pp. 519-522, 2016.
(135) D. Butterfield, A. Swomley and R. Sultana, "Amyloid b-Peptide (l-42)-lnduced Oxidative Stress in Alzheimer Disease: Importance in Disease Pathogenesis and Progression," Antioxidants & Redox Signalling, vol. 19, no. 8, pp. 823-835, 2013.
(136) G. Perry, A. Cash and M. Smith, "Alzheimer Disease and Oxidative Stress," Journal of Biomedicine and Biotechnology, vol. 2, no. 3, pp. 120-123, 2002.
(137) C. Chen and C. Zhong, "Oxidative stress in Alzheimer's disease," Neurosci. Bull., vol. 30, no. 2, pp.
271-281, 2014.
(138) A. Gella and N. Durany, "Oxidative stress in Alzheimer disease," Cell Adhesion & Migration, vol. 3, no. 1, pp. 88-93, 2009.
(139) J. Ratnayaka, L. Serpell and A. Lotery, "Dementia of the eye: the role of amyloid beta in retinal degeneration," Eye, vol. 29, pp. 1013-1026, 2015.
(140) G. Taylor-Walker, S. Lynn, E. Keeling, R. Munday, D. Johnston, A. Page, J. Scott, S. Goverdhan, A.
Lotery and J. Ratnayaka, "The Alzheimer's-related amyloid beta peptide is internalised by R28 neuroretinal cells and disrupts the microtubule associated protein 2 (MAP-2)," Experimental Eye Research, vol. 153, pp. 110-121, 2016.
(141) N. Nagai, Y. Ito and T. Tanino, "Effect of High Glucose Levels on Amyloid β Production in Retinas of Spontaneous Diabetes Mellitus Otsuka Long-Evans Tokushima Fatty Rats," Biol. Pharm. Bull., vol. 38, no. 4, pp. 601-610, 2015.
(142) J. Ding, J. Lin, B. Mace, R. Herrmann, P. Sullivan and C. Bowes Rickman, "Targeting age-related macular degeneration with Alzheimer's disease based immunotherapies: Anti-amyloid-b antibody attenuates pathologies in an age-related macular degeneration mouse model," Vision Research, vol. 48, no. 3, pp. 339-345, 2008.
(143) J. Ding, L. Johnson, R. Herrmann, S. Farsiu, S. Smith, M. Groelle, B. Mace, P. Sullivan, J. Jamison, U.
Kelly, O. Harrabi, S. Bollini, J. Dilley, D. Kobayashi, B. Kuang, W. Li, J. Pons, J. Lin and C. Bowes Rickman, "Anti-amyloid therapy protects against retinal pigmented epithelium damage and vision loss in a model of age-related macular degeneration," Proc Natl Acad Sci U S A, vol. 108, no. 28, pp. E279-287, 2011.
(144) Remington and J. P., Remington: The Science and Practice of Pharmacy, L. Allen Jr., Ed.,
Philadelphia, PA: Pharmaceutical Press, 2012, p. 2724.
(145) R. Rowe, P. Sheskey, W. G. Cook and M. E. Fenton, Handbook of Pharmaceutical Excipients, 7th Edition ed., London: Pharmaceutical Press, 2012.
(146) P. Li and L. Zhao, "Developing early formulations: Practice and perspective," International Journal of Pharmaceutics, vol. 341, no. 1-2, pp. 1-19, 2007.
(147) T. Eteraf-Oskouei and M. Najafi, "Traditional and Modern Uses of Natural Honey in Human
Diseases: A Review," Iran J Basic Med Sci., vol. 16, no. 6, pp. 731-742, 2013.
(148) S. Ahmed and N. Othman, "Review of the Medicinal Effects of Tualang Honey and a Comparison with Manuka Honey," Malays. J. Med. Sci., vol. 20, no. 3, pp. 6-13, 2013.
(149) M. Aznan, O. Khan, A. Unar, S. Tuan Sharif, A. Khan, S. Abd. Aziz and A. Zakaria, "Effect of Tualang honey on the anastomotic wound healing in large bowel anastomosis in rats-A randomized controlled trial," BMC Complementary and Alternative Medicine, vol. 16, p. 28, 2015.
(150) G. Zorzi, E. Carvalhob, G. von Posera and H. Teixeiraa, "On the use of nanotechnology-based
strategies for association of complex matrices from plant extracts," Revista Brasileira de
Farmacognosia, vol. 25, no. 4, pp. 426-436, 2015.
(151) M. Sharma, "Applications of Nanotechnology Based Dosage Forms for Delivery of Herbal Drugs," Journal of Pharmaceutics and nanotechnology, vol. 2, no. 1, pp. 23-30, 2014.
(152) S. S. Ajazuddin, "Applications of novel drug delivery system for herbal formulations," Fitoterapia, vol. 81, pp. 680-689, 2010.
(153) F. Aqil, R. Munagala, J. Jeyabalan and M. Vadhanam, "Bioavailability of phytochemicals and its enhancement by drug delivery systems," Cancer Letters, vol. 334, no. 1, pp. 133-141, 2013.
(154) A. Aisha, A. Majid and Z. Ismail, "Preparation and characterization of nano liposomes of
Orthosiphon stamineus ethanolic extract in soybean phospholipids.," BMC Biotechnol. , vol. 14, p. 23, 2014.
(155) A. Jiang, J. Wang, M. Joshi and J. Christoforidis, "Systemic treatments for noninfectious vitreous inflammation," Mediators of Inflammation, vol. Annual, p. 11, 2013.
(156) E. Touitou, N. Dayan, L. Bergelson, B. Godin and M. Eliaz, "Ethosomes— novel vesicular carriers for enhanced delivery: characterization and skin penetration properties," 7. Control Release, vol. 65, no. 3, pp. 403-418, 2000.
(157) T. Parashar, Soniya, R. Sachan, V. Singh, G. Singh, S. Tyagi, C. Patel and A. Gupta, "Ethosomes: A recent vesicle of transdermal drug delivery system," Int. J. Res. Dev. Pharm. L. Sci., vol. 2, no. 2, pp. 285-292, 2013.
(158) R. Tiwari, N. Chauhan and H. Yogesh, "Ethosomes: A potential carries for transdermal drug
delivery," IntJ.Drug Dev. & Res., vol. 2, no. 2, pp. 448-452, 2010.
(159) R. Kesharwani, D. Patel, A. Sachan, V. Kumar and B. Mazumdar, "Ethosomes: A Novel Approach for Transdermal and Topical Drug Delivery," Research J. Topical and Cosmetic Sci., vol. 6, no. 1, pp. 15-20, 2015.
(160) L. Tyagi, S. Kumar, S. Maurya and M. Kori, "Ethosomes: Novel vesicular carrier for enhanced
transdermal drug delivery system," Bulletin of Pharmaceutical Research, vol. 3, no. 1, pp. 6-13, 2013.
(161) M. de Oliveira, A. Magri, C. Baldo, D. Camilios-Neto, T. Minucelli and M. Celligoi, "Review:
Sophorolipids A Promising Biosurfactant and it's Applications," International Journal of Advanced Biotechnology and Research, vol. 6, no. 2, pp. 161-174, 2015.
(162) R. Yatim and H. Zafarizal, "Process for the production of sophorolipid biosurfactant," Malaysian Palm Oil Board, 2012.
(163) R. Yatim, A. Norashikin and Z. Hassan, "Application of a palm-based sophorolipid as a liquid
deodorant," Malayisan Palm Oil Board, 2010.
(164) S. Mohamed, A. Majid, A. Yatim, M. Vishkaei and M. Asif, "Antiangiogenic Effects of Sophorolipids Extracted from Malaysian Palm Oil," 7. ofBiomed. & Clin. Sci., vol. 1, no. 1, p. 68, 2016.
(165) S. Bhattacharya and A. Ghosh, "Phytosomes: the Emerging Technology for Enhancement of Bioavailability of Botanicals and Nutraceuticals," The Internet Journal of Aesthetic and Antiaging Medicine, vol. 2, no. 1, p. 8, 2008.
(166) A. Patel, Y. Tanwar, S. Rakesh and P. Poojan, "Phytosome: Phytolipid Drug Dilivery System for Improving Bioavailability of Herbal Drug," Journal of Pharmaceutical Science and Bioscientific Research, vol. 3, no. 2, pp. 51-57, 2013.
(167) T. Amin and S. Bhat, "A Review on Phytosome Technology as a Novel Approach to Improve The Bioavailability of Nutraceuticals," International Journal of Advancements in Research &
Technology, vol. 1, no. 3, p. 15, 2012.
(168) S. Svenson and A. Chauhan, "Solubility Enhancement of Poorly Water Soluble Molecules Using Dendrimers;," Nanomedicine, vol. 3, no. 5, pp. 679-702, 2008.
(169) A. Mustafa, M. Widodo and Y. Kristianto, "Albumin And Zinc Content Of Snakehead Fish (Channa striata) Extract And Its Role In Health," IEESE International Journal of Science and Technology , vol. 1, no. 2, pp. 1-8, 2012.
(170) P. Rahayu, F. Marcelline, E. Sulistyaningrum, M. Suhartono and R. Tjandrawinata, "Potential effect of striatin (DLBS0333), a bioactive protein fraction isolated from Channa striata for wound treatment," Asian Pac. J. Trop. Biomed., vol. 6, no. 12, pp. 1001-1007, 2016.
(171) T. Crawford, D. Alfaro, J. Kerrison and E. Jablon, "Diabetic retinopathy and angiogenesis," Current Diabetes Reviews, vol. 5, no. 1, pp. 8-13, 2009.
(172) M. Saeed, E. Gkaragkani and K. AN, "Emerging roles for antiangiogenesis factors in management of ocular disease," Clinical Opthalmology, vol. 6, pp. 533-543, 2013.
(173) A. Witmer, G. Vrensen, C. Van Noorden and R. Schlingemann, "Vascular endothelial growth
factors and angiogenesis in eye disease," Progress in Retinal and Eye Research, vol. 22, no. 1, pp. 1-29, 2003.
(174) P. Wiedemann, "Growth Factors in Retinal Diseases: Proliferative Vitreoretinopathy, Proliferative Diabetic Retinopathy, and Retinal Degeneration.," Survey of Opthalmology, vol. 36, no. 5, pp. 373- 384, 1992.
(175) M. Hartnett, Penn and J.S., "Mechanisms and Management of Retinopathy of Prematurity," N Engl J Med, vol. 367, no. 26, pp. 2515-2526, 2012.
(176) J. Cao, M. Mathews, D. McLeod, C. Merges, L. Hjelmeland and G. Lutty, "Angiogenic factors in human proliferative sickle cell retinopathy," British Journal of Opthalmology, vol. 83, no. 7, pp. 838-846, 1999.
(177) C. Cursiefen, M. Kuchle and G. Naumann, "Angiogenesis in Corneal Diseases: Histopathologic Evaluation of 254 Human Corneal Buttons with Neovascularization," Cornea, vol. 17, no. 6, pp. 611-613, 1998.
(178) R. Tripathi, J. Li, B. Tripathi, K. Chalam and A. Adamis, "Increased level of vascular endothelial growth factor in aqueous humor of patients with neovascular glaucoma," Ophthalmology, vol. 105, no. 2, pp. 232-237, 1998.
(179) A. Chintakuntlawa and J. Chodosh, "Cellular and Tissue Architecture of Conjunctival Membranes in Epidemic Keratoconjunctivitis," Ocular Immunology and Inflammation, vol. 18, no. 5, pp. 341-345, 2010.
(180) C. Cursiefen, J. Colin, R. Dana, M. Diaz-Llopis, L. Faraj, S. Garcia-Delpech, G. Geerling, F. Price, L.
Remeijer, B. Rouse, B. Seitz, P. Udaondo, D. Meller and H. Dua, "Consensus statement on indications for anti-angiogenic therapy in the management of corneal diseases associated with
neovascularisation: outcome of an expert roundtable," British Journal of Opthalmology, vol. 96, no. 1, pp. 3-9, 2012.
(181) C. Livezeanu, M. Craitoiu, . Manescu, C. Mocanu and S. Craitoiu, "Angiogenesis in the
pathogenesis of pterygium," Rom. J. Morphol. Embryol., vol. 52, no. 3, pp. 837-844, 2011.
(182) T. Carmachael, "Corneal angiogenesis in Ocular Angiogenesis: Diseases, Mechanisms, and
Therapeutics," in Ocular angiogenesis: diseases, mechanisms, and therapeutics, J. Tombran-Tink and C. J. Barnstable, Eds., Totowa, NJ: Humana Press, 2006, pp. 45-72.
(183) S. Lisi, M. Sisto, M. D'Amore, D. Lofrumento and D. Ribatti, "Emerging avenues linking
inflammation, angiogenesis and Sjogren's syndrome," Cytokine, vol. 61, no. 3, pp. 693-703, 2013.
(184) A. Gomaa, M. Yaar, M. Eyada and J. Bhawan, "Lymphangiogenesis and angiogenesis in non- phymatous rosacea ," Journal of Cutaneous Pathology. , vol. 34, no. 10, pp. 748-753, 2007.
(185) K. Aroni, E. Tsagroni, K. N., E. Patsouris and E. loannidis, "A study of the pathogenesis of rosacea: how angiogenesis and mast cells may participate in a complex multifactorial process.," Archives of Dermatological Research, vol. 300, no. 3, pp. 125-131, 2008.
(186) N. Macaron, C. Cohen, S. Chen and J. Arbiser, "Cutaneous lesions of secondary syphilis are highly angiogenic," Journal of the American Academy of Dermatology, vol. 48, no. 6, pp. 878-881, 2002.
(187) S. Oehlers, M. Cronan, N. Scott, M. Thomas, K. Okuda, E. Walton, R. Beerman, P. Crosier and D.
Tobin, "Interception of host angiogenic signalling limits mycobacterial growth," Nature, vol. 517, no. 7536, pp. 612-615, 2015.
(188) M. Meyer, M. Clauss, A. Lepple-Wienhues, J. Waltenberger, H. Augustin, M. Ziche, C. Lanz, M.
Buttner, H. Rziha and C. Dehio, "A novel vascular endothelial growth factor encoded by Orf virus, VEGF- E, mediates angiogenesis via signalling through VEGFR-2 (KDR) but not VEGFR-1 (Fit- 1) receptor tyrosine kinases," EMBOJ., vol. 18, no. 2, pp. 363-374, 1999.
(189) K. Harada, S. Lu, D. Chisholm, S. Syrjanen and A. Schor, "Angiogenesis and vasodilation in skin warts. Association with HPV infection," Anticancer Research, vol. 20, no. 6B, pp. 4519-4523, 2000.
(190) G. Barillari and B. Ensoli, "Angiogenic effects of extracellular human immunodeficiency virus type 1 Tat protein and its role in the pathogenesis of AIDS-associated Kaposi's sarcoma," Clin.
Microbiol. Rev., vol. 15, no. 2, pp. 310-326, 2002.
(191) J. Joyal, Y. Sun, M. Gantner, Z. Shao, L. Evans, N. Saba, F. T. S. Burnim, J. Kim, G. Patel, A. Juan, C.
Hurst, C. Hatton, Z. Cui, K. Pierce, P. Bherer, E. Aguilar, M. Powner, K. Vevis, M. Boisvert, Z. Fu, E. Levy, M. Fruttiger, A. Packard, F. Rezende, B. Maranda, P. Sapieha, J. Chen, M. Friedlander, C. Clish and L. Smith, "Retinal lipid and glucose metabolism dictates angiogenesis through lipid sensor Ffarl," Nature Medicine, vol. 22, no. 4, pp. 439-445, 2016.
(192) S. Szabo, X. Deng, G. Tolstanova, T. Khomenko, B. Paunovic, L. Chen, M. Jadus and Z. Sandor, "Angiogenic and anti-angiogenic therapy for gastrointestinal ulcers: new challenges for rational therapeutic predictions and drug design," Curr. Pharm Des., vol. 17, no. 16, pp. 1633-1642, 2011.
(193) M. Aghi, S. Rabkin and R. Martuza, "Angiogenic response caused by oncolytic herpes simplex virus-induced reduced thrombospondin expression can be prevented by specific viral mutations or by administering a thrombospondin-derived peptide.," Cancer Research, vol. 67, no. 2, pp. 440- 444, 2007.
(194) N. Osherov and R. Ben-Ami, "Modulation of Host Angiogenesis as a Microbial Survival Strategy and Therapeutic Target," PLoS Pathogens, vol. 12, no. 4, p. el005479, 2016.
(195) D. Hos, F. Bock, B. Bachmann and Cursiefen, "Corneal Neovascular Diseases," in Anti-Angiogenic Therapy in Opthalmology, A. Stahl, Ed., Springer International Publishing, 2016, pp. 159-172.
(196) D. Walsh, "Angiogenesis and arthritis.," Rheumatology, vol. 38, no. 2, pp. 103-112, 1999.
(197) C. Bonnet and D. Wales, "Osteoarthritis, angiogenesis and inflammation," Rheumatology, vol. 44, no. 1, pp. 7-16, 2005.
(198) C. M.-H. M. Lambert, J. Dubuc, E. Montell, J. Verges, C. Munaut, A. Noel and Y. Henrotin,
"Characterization of synovial angiogenesis in osteoarthritis patients and its modulation by chondroitin sulfate," Arthritis Research & Therapy, vol. 14, p. R58, 2012.
(199) Y. Henrotin, L. Pesesse and C. Lambert, "Targeting the synovial angiogenesis as a novel treatment approach to osteoarthritis," Therapeutic Advances in Musculoskeletal Diseases, vol. 6, no. 1, pp. 20-34, 2014.
(200) E. Robak, A. Wozniacka, A. Sysa-Jedrzejowska, H. Stepien and T. Robak, "Circulating angiogenesis inhibitor endostatin and positive endothelial growth regulators in patients with systemic lupus erythematosus," Lupus, vol. 11, no. 6, pp. 348-355, 2002.
(201) J. Liu, X. Wang, X. Yang, Q. Yan, S. Wang and W. Han, "Investigating the role of angiogenesis in systemic lupus erythematosus," Lupus, vol. 24, no. 6, pp. 621-627, 2015.
(202) K. Kikuchi, T. Hoashi, S. Kanazawa and K. Tamaki, "Angiogenic cytokines in serum and cutaneous lesions of patients with polyarteritis nodosa," J Am Acad Dermatol, vol. 53, no. 1, pp. 57-61, 2005.
(203) T. Zielonka, U. Demkow, E. Radzikowska, B. Bialas, M. Filewska, K. Zycinska, M. Obrowski, J.
Kowalski, K. Wardyn and E. Skopinska-Rozewska, "Angiogenic activity of sera from interstitial lung disease patients in relation to pulmonary function," European Journal of Medical Research, vol. 15, no. Suppl 2, pp. 229-234, 2010.
(204) A. Marneros, "Increased VEGF-A promotes multiple distinct aging diseases of the eye through shared pathomechanisms," EMBO Molecular Medicine, vol. 8, no. 3, pp. 208-231, 2016.
(205) A. Rattner and J. Nathans, "Macular degeneration: recent advances and therapeutic
opportunities," Nature Reviews Neuroscience, vol. 7, no. 11, pp. 860-872, 2006.
(206) F. Lopes, F. Traina, C. Almeida, F. Leonardo, C. Franco-Penteado, V. Garrido, M. Colella, R. Soares,
5. Olalla-Saad, F. Costa and C. Nicola, "Key endothelial cell angiogenic mechanisms are stimulated by the circulating milieu in sickle cell disease and attenuated by hydroxyurea," Haematologica, vol. 100, no. 6, pp. 730-739, 2015.
(207) A. Tzouvelekis, S. Anevlavis and D. Bouros, "Angiogenesis in Interstitial Lung Diseases: a
pathogenetic hallmark or a bystander?," Respiratory Research, vol. 7, no. 1, p. 82, 2006.
(208) A. Abu El-Asrar, S. Al-Kharashi, L. Missotten and K. Geboes, "Expression of growth factors in the conjunctiva from patients with active trachoma," Eye, vol. 20, pp. 362-369, 2006.
(209) F. Verbraak, "Antivascular endothelial growth factor treatment in pseudoxanthoma elasticum patients," Developmental Opthalmology, vol. 46, pp. 96-106, 2010.
(210) P. Ellis, A. MacLean, L. Wong Te Fong, J. Crow and C. Perrett, "Angiogenesis in Paget's Disease of the Vulva and the Breast: Correlation with Microvessel Density," Journal of Oncology, vol. 2012, p.
6, 2012.
(211) R. Tarquini, F. Perfetto and B. Tarquini, "Endothelin-l and Paget's Bone Disease: Is There a Link?," Calcified Tissue International, vol. 63, no. 2, pp. 118-120, 1998.
(212) R. Pirzer, N. Tilly, U. Sommer, U. Liegibel, I. Grafe, P. Nawroth and C. Kasperk, "Endothelin-l levels in patients with Paget's disease of bone," Exp Clin Endocrinol Diabetes, vol. 113, no. 10, pp. 598- 601, 2005.
(213) S. Boyd, I. Zachary, U. Chakravarthy, G. Allen, G. Wisdom, I. Cree, J. Martin and P. Hykin,
"Correlation of increased vascular endothelial growth factor with neovascularization and permeability in ischemic central vein occlusion.," Arch Ophthalmol, vol. 120, no. 12, pp. 1644- 1650, 2002.
(214) I. Kuo and J. E. T. Cunningham, "Ocular neovascularization in patients with uveitis," International ophthalmology clinics, vol. 40, no. 2, pp. 111-126, 2000.
(215) J. Biswas, . Ravi, A. Naryanasamy, L. Kulandai and H. Madhavan, "Eales' disease - current
concepts in diagnosis and management," J Ophthalmic Inflamm Infect, vol. 3, no. 1, pp. 1-5, 2013.
(216) D. Keskin, G. Keskin, A. Inal and Ozsik, "Serum angiostatin levels in patients with Behcet's disease: does angiogenesis play a role in the pathogenesis of Behcet's disease?," Acta Clinica Belgica, vol. 69, no. 4, pp. 246-250, 2014.
(217) M. Munk, R. Ruckert, M. Zinkernagel, A. Ebneter and S. Wolf, "The role of anti-VEGF agents in myopic choroidal neovascularization: Current standards and future outlook," Expert Opinion on Biological Therapy, vol. 16, no. 4, pp. 477-487, 2016.
(218) F. Scaldaferri, S. Vetrano, M. Sans, V. Arena, G. Straface, E. Stigliano, A. Repici, A. Sturm, A.
Malesci, J. Panes, S. Yla-Herttuala, C. Fiocchi and S. Danese, "VEGF-A links angiogenesis and inflammation in inflammatory bowel disease pathogenesis.," Gastroenterology, vol. 136, no. 2, pp. 585-595, 2009.
(219) C. Alkim, H. Alkim, A. Koksal, S. Boga and I. Sen, "Angiogenesis in Inflammatory Bowel Disease," International Journal of Inflammation , vol. 2015, p. 10, 2015.
(220) I. Pousa, J. Mate and J. Gisbert, "Angiogenesis in inflammatory bowel disease," Eur J Clin Invest, vol. 38, no. 2, pp. 73-81, 2008.
(221) I. Koutroubakis, G. Tsiolakidou, K. Karmiris and E. Kouroumalis, "Role of angiogenesis in
inflammatory bowel disease," Inflammatory Bowel Diseases, vol. 12, no. 6, pp. 515-523, 2006.
(222) N. Meyer and C. Akdis, "Vascular Endothelial Growth Factor as a Key Inducer of Angiogenesis in the Asthmatic Airways," Current Allergy and Asthma Reports, vol. 13, no. 1, pp. 1-9, 2013.
(223) M. Vikkula, L. Boon, K. Carraway 3rd, J. Calvert, A. Diamonti, B. Goumnerov, K. Pasyk, D. Marchuk, M. Warman, L. Cantley, J. Mulliken and B. Olsen, "Vascular Dysmorphogenesis Caused by an Activating Mutation in the Receptor Tyrosine Kinase TIE2," Cell, vol. 87, no. 7, pp. 1181-1190, 1996.
(224) I. Stalmans, D. Lambrechts, F. De Smet, S. Jansen, J. Wang, S. Maity, P. Kneer, M. von der Ohe, A.
Swillen, C. Maes, M. Gewillig, D. Molin, P. Hellings, T. Boetel, M. Haardt, V. Compernolle, M. Dewerchin, S. Plaisance, R. Vlietinck, B. Emanuel, A. Gittenberger-de Groot, P. Scambler, B.
Morrow, D. Driscol, L. Moons, C. Esguerra, G. Carmeliet, A. Behn-Krappa, K. Devriendt, D. Collen, S. Conway and P. Carmeliet, "VEGF: a modifier of the del22qll (DiGeorge) syndrome?," Nat. Med., vol. 9, no. 2, pp. 173-182, 2003.
(225) S. van den Driesche, C. Mummery and C. Westermann, "Hereditary hemorrhagic telangiectasia: an update on transforming growth factor β signaling in vasculogenesis and angiogenesis Authors," Cardiovascular Research, vol. 58, no. 1, pp. 20-31, 2003.
(226) P. Mabeta and M. Pepper, "Hemangiomas - current therapeutic strategies," Int. J. Dev. Biol., vol.
55, no. 4-5, pp. 431-437, 2011.
(227) M. Rupnick, D. Panigrahy, C.-Y. Zhang, S. Dallabrida, B. Lowell, R. Langer and M. Folkman,
"Adipose tissue mass can be regulated through the vasculature," Proc. Natl. Acad. Sci. USA, vol. 99, no. 16, p. 10730-10735, 2002.
(228) M. Detmar, "The role of VEGF and thrombospondins in skin angiogenesis," Journal of
Dermatological Science, vol. 24, no. Supplement 1, pp. S78-S84, 2000.
(229) M. Vladau, A. Cimpean, R. Balica, A. Jitariu, R. Popovici and M. Raica, "VEGF/VEGFR2 Axis in
Periodontal Disease Progression and Angiogenesis: Basic Approach for a New Therapeutic Strategy.," In Vivo, vol. 30, no. 1, pp. 53-60, 2016.
(230) V. Booth, S. Young, A. Cruchley, N. Taichman and E. Paleolog, "Vascular endothelial growth factor in human periodontal disease," 7. Periodontal Res., vol. 33, no. 8, pp. 491-499, 1998.
(231) C. Molinas, M. Binda and P. Koninckx, "Angiogenic factors in peritoneal adhesion formation," Gynecological Surgery, vol. 3, no. 3, pp. 157-167, 2006.
(232) M. Kralickova and V. Vetvicka, "Role of angiogenesis in endometriosis," Pathology Discovery, vol.
4, p. 5, 2016.
(233) A. Rocha, R. F. and R. Taylor, "Angiogenesis and endometriosis," Obstet. Gynecol. Int., vol. 2013, no. Annual, p. 8, 2013.
(234) R. Taylor, J. Yu, P. Torres, A. Schickedanz, J. Park, M. Michael and N. Sidell, "Mechanistic and Therapeutic Implications of Angiogenesis in Endometriosis," Reproductive Sciences, vol. 16, no. 2, pp. 140-146, 2009.
(235) L. Reynolds, A. Grazul-Bilska and D. Redmer, "Angiogenesis in the female reproductive organs: pathological implications.," International Journal of Experimental Pathology, vol. 83, no. 4, pp. 151-163, 2002.
(236) K. Neely and T. Gardner, "Ocular Neovascularization: Clarifying Complex Interactions," American Journal of Pathology, vol. 153, no. 3, pp. 665-670, 1998.
(237) P. Campochiaro, "Ocular neovascularization," Journal of Molecular Medicine, vol. 91, no. 3, pp.
311-321, 2013.
(238) M. Tolentino, "Systemic and Ocular Safety of Intravitreal Anti-VEGF Therapies for Ocular
Neovascular Disease," Survey of Ophthalmology, vol. 56, no. 2, pp. 95-113, 2011.
(239) J. LeCouter, J. Kowalski, J. Foster, P. Hass, Z. Zhang, L. Dillard-Telm, G. Frantz, L. Rangell, L.
DeGuzman, G. Keller, F. Peale, A. Gurney, K. H ilia n and F. N., "Identification of an angiogenic mitogen selective for endocrine gland endothelium," Nature, vol. 412, no. 6850, pp. 877-884, 2001.
(240) A. Martin, M. Komada and D. Sane, "Abnormal Angiogenesis in Diabetes Mellitus," Medicinal Research Reviews, vol. 23, no. 2, pp. 117-145, 2003.
(241) G. Kolluru, S. Bir and C. Kevil, "Endothelial Dysfunction and Diabetes: Effects on Angiogenesis, Vascular Remodeling, and Wound Healing," International Journal of Vascular Medicine, vol. 5, no. 918267, p. 30, 2012.
(242) R. Soares, "Angiogenesis in Diabetes. Unraveling the Angiogenic Paradox.," The Open Circulation and Vascular Journal, vol. 3, no. 1, pp. 3-9, 2010.
(243) B. Himani, B. Seema, N. Bhole and S. Mamta, "Misai kuching: A glimpse of maestro," International Journal of Pharmaceutical Sciences Review and Research, vol. 22, no. 2, pp. 55-59, 2013.
(244) M. Almatar, H. Ekal and Z. Rahmat, "A Glance on Medical Applications of Orthosiphon stamineus and Some of its Oxidative Comp," International Journal of Pharmaceutical Sciences Review and Research, vol. 24, no. 2, pp. 83-88, 2014.
(245) P. Holm, R. Slart, Z. Clark, J. Hillebrands and R. Tio, "Does the Role of Angiogenesis play a Role in Atherosclerosis and Plaque Instability?," Annals of Medicine, vol. 41, no. 4, pp. 257-264, 2009.
(246) F. Cerimele, L. Brown, F. Bravo, G. Ihler, P. Kouadio and J. Arbiser, "Infectious Angiogenesis :
Bartonella bacilliformis Infection Results in Endothelial Production of Angiopoetin-2 and
Epidermal Production of Vascular Endothelial Growth Factor," The American Journal of Pathology, vol. 163, no. 4, pp. 1321-1327, 2003.
(247) R. Katoh, "Angiogenesis in Endocrine Glands: Special Reference to the Expression of Vascular Endothelial Growth Factor," Microscopy Research and Technique, vol. 60, no. 2, pp. 181-185, 2003.
(248) O. Segiet, M. Michalski, M. Brzozowa-Zasada, A. Piecuch, M. Zaba, K. Helewski, A. Gabriel and R.
Wojnicz, "Angiogenesis in primary hyperparathyroidism," Annals of Diagnostic Pathology, vol. 19, no. 2, pp. 91-98, 2015.
(249) P. Martins, F. Schmitt, H. Almeida and J. Frazao, "Evaluation of parathyroid gland angiogenesis in chronic kidney disease associated with secondary hyperparathyroidism," Nephrology Dialysis Transplantation, vol. 23, no. 9, pp. 2889-2894, 2008.
(250) C. Vulpio, M. Bossola, E. Di Stasio, L. Tazza, P. Silvestri and G. Fadda, "Histology and
immunohistochemistry of the parathyroid glands in renal secondary hyperparathyroidism refractory to vitamin D or cinacalcet therapy.," European Journal of Endocrinology, vol. 168, no. 6, pp. 811-819, 2013.
(251) J. Folkman, "Tumor Angiogenesis," Advances in Cancer Research, vol. 43, pp. 175-203, 1985.
(252) M. M0ller, K. Werther, A. Nalla, S. Stangerup, J. Thomsen, T. B0g-Hansen, H. Nielsen and P. Caye- Thomasen, "Angiogenesis in vestibular schwannomas: expression of extracellular matrix factors MMP-2, MMP-9, and TIMP-1," Laryngoscope, vol. 120, no. 4, pp. 657-662, 2010.
(253) N. Voelkel, C. Cool, L. Taraceviene-Stewart, M. Geraci, M. Yeager, T. Bull, M. Kasper and R. Tuder, "Janus face of vascular endothelial growth factor: the obligatory survival factor for lung vascular endothelium controls precapillary artery remodeling in severe pulmonary hypertension," Critical Care Medicine, vol. 30, no. 5 Suppl, pp. S251-S256, 2002.
(254) M. Yeager, G. Halley, H. Golpon, N. Voelkel and R. Tuder, "Microsatellite instability of endothelial cell growth and apoptosis genes within plexiform lesions in primary pulmonary hypertension.," Ore. Res., vol. 88, no. 1, pp. E2-E11, 2001.
(255) S. Scialla, R. Cole and L. Bednarz, "Redefining Cancer-Related Asthenia-Fatigue Syndrome," Journal of Palliative Medicine, vol. 9, no. 4, pp. 866-872, 2006.
(256) E. Bruera and C. Sweeney, "Cachexia and asthenia in cancer patients," Lancet Oncology, vol. 1, pp.
138-147, 2000.
(257) Monk, J. P., G. Phillips, R. Waite, J. Kuhn, L. Schaaf, G. Otterson, D. Guttridge, C. Rhoades, M. Shah, T. Criswell, M. Caligiuri and M. Villalona-Calero, "Assessment of Tumor Necrosis Factor Alpha Blockade As an Intervention to Improve Tolerability of Dose-Intensive Chemotherapy in Cancer Patients," J Clin Oncol, vol. 24, no. 12, pp. 1852-1859, 2006.
(258) H. Neuenschwander and E. Bruera, "Pathophysiology of Cancer Asthenia," in Topics in Palliative Care, vol. 2, New York, New York: Oxford University Press, 1998, pp. 171-181.
(259) C. U.S. Department of Health and Human Services (FDA, "Guidance For Industry. Estimating the Maximum Safe Starting Dose in Initial Clinical Trials For Therapeutics in Adult Healthy Volunteers," Pharmacology and Toxicology, July 2005.
(260) A. Nair and S. Jacob, "A simple practice guide for dose conversion between animals and human," J. Basic. Clin. Pharma., vol. 7, pp. 27-31, 2016.
(261) J.-W. Shin, l.-C. Seol and C.-G. Son, "Interpretation of animal dose and human equivalent dose for drug development," 7. Korean Oriental Medicine, vol. 31, no. 3, pp. 1-7, 2010.
(262) J. Shah, H. Shah, A. Groshev, A. Hirani, Y. Pathak and V. B. Sutariya, "Nanoparticulate Transscleral Ocular Drug Delivery," J Biomol Res Ther, vol. 3, no. 3, p. 14, 2014.
(263) H. Liu, J. Hao and K. Li, "Current strategies for drug delivery to the inner ear," Acta Pharmaceutica Sinica B, vol. 3, no. 2, pp. 86-96, 2013.
(264) N. H. Saidan, A. F. A. Aisha, M. S. R. Hamil, A. M. S. A. Majid and Z. Ismail, "A novel reverse phase high-performance liquid chromatography method for standardization of Orthosiphon stamineus leaf extracts," Pharmacognosy Research, vol. 7, no. 1, pp. 23-31, 2015.
(265) M. Siddiqui, S. Hafizoh, S. Ismail, M. Helal and A. Majid, "Analysis of Total Proteins,
polysaccharides and glycosaponions contents of Orthosiphon stamineus Benth. in spray and freeze dried methanol :Water (1:1) extractract and its contribution to cytotoxic and antiangiogenic activities," Phcog Mag, vol. 1, no. 5, pp. 320-326, Sep-Oct 2009.
(266) V. Kraujalyte, P. R. Venskutonis, A. Pukalskas, L. Cesoniene and R. Daubaras, "Anti-oxidant
properties and polyphenolic compositions of fruits from different European cranberrybush (Viburnum opulus L.) genotypes," Food Chemistry, vol. 141, no. 4, pp. 3695-3702, 2013.
(267) F. P. Flores, R. K. Singh, W. L. Kerr, R. B. Pegg and F. Kong, "Total phenolics content and antioxidant capacities of microencapsulated blueberry anthocyanins during in vitro digestion," Food Chemistry, vol. 153, pp. 272-278, 2014.
(268) C. C. Chang, M. H. Yang, H. M. Wen and J. C. Chern, "Estimation of total flavonoid content in propolis by two complementary colorimetric methods," Journal of Food and Drug Analysis, vol. 10, no. 3, pp. 178-182, 2002.
(269) E. Suhartono, E. Viani, M. A. Rahmadhan, I. S. Gultom, M. F. Rakhman and D. Indrawardhana, "Total flavonoid and Anti-oxidant Activity of Some Selected Medicinal Plants in South Kalimantan of Indonesian," APCBEE Procedia, vol. 4, pp. 235-239, 2012.
(270) R. Chirinos, R. Pedreschi, H. Rogez, Y. Larondelle and D. Campos, "Phenolic compound contents and anti-oxidant activity in plants with nutritional and/or medicinal properties from the Peruvian Andean region," Industrial Crops and Products, vol. 47, pp. 145-152, 2013.
(271) J. Stewart, "Colorimetric determination of phospholipids with ammonium ferrothiocyanate.," Analytical Biochemistry, vol. 104, no. 1, pp. 10-14, 1980.
(272) O. Lowry, N. Rosebrough, A. Farr and R. Randall, "Protein measurement with the folin phenol reagent," 7. Biol. Chem., vol. 193, no. 1, pp. 265-275, 1951.
(273) K. J. Brown, S. F. Maynes, A. Bezos, D. J. Maguire, M. D. Ford and C. R. Parish, "A novel in vitro assay for human angiogenesis," Laboratory Investigation, vol. 75, no. 4, pp. 539-555, 1996.
(274) R. Nicosia, E. Bonanno and S. Villaschi, "Large-vessel endothelium switches to a microvascular phenotype during angiogenesis in collagen gel culture of rat aorta," Arthewrosclerosis, vol. 95, no. 2-3, pp. 191-199, 1992.
(275) O. S. A. Al-Salahi, C. Kit Lam, A. M. S. A. Majid, F. S. R. Al-Suede, S. A. Mohammed Saghir, W. Z.
Abdullah and M. B. K. Y. N. M. Ahamed, "Anti-angiogenic quassinoid-rich fraction from Eurycoma longifolia modulates endothelial cell function," Microvascular Research, vol. 90, pp. 30-39, 2013.
(276) T. Mosmann, "Rapid colorimetric assay for cellular growth and survival: application to
proliferation and cytotoxicity assays," Journal of Immunological Methods, vol. 65, no. 1-2, p. 55- 63, 1983.
(277) C. C. Liang, A. Y. Park and J. L. Guan, "In vitro scratch assay: a convenient and inexpensive method for analysis of cell migration in vitro," Nature Protocols, vol. 2, no. 2, pp. 329-333, 2007.
(278) A. Valster, N. L. Tran, M. Nakada, M. E. Berens, A. Y. Chan and M. Symons, "Cell migration and invasion assays," Methods, vol. 37, no. 2, pp. 208-215, 2005.
(279) A. Bandyopadhyay, Y. Zhu, S. Malik, J. Kreisberg, M. Brattain, E. Sprague, J. Luo, L.' . Casillas, F. and L. Sun, "Extracellular domain of TGF-β type III receptor inhibits angiogenesis and tumor growth in human cancer cells," Oncogene, vol. 1, no. 22, pp. 3541-3551, 2002.
(280) D. C. West, W. D. Thompson, P. G. Sells and M. F. Burbridge, "Angiogenesis Assays Using Chick Chorioallantoic Membrane," Methods in Molecular Medicine, vol. 46, pp. 107-29, 2001.
(281) D. ibatti, "Chick embryo chorioallantoic membrane as a useful tool to study angiogenesis," International Review of Cell And Molecular Biology, vol. 270, pp. 181-224, 2008.
(282) A. Ozcetin, A. Aigner and U. Bakowsky, "A chorioallantoic membrane model for the determination of anti-angiogenic effects of imatinib," European Journal of Pharmaceutics and Biopharmaceutics, vol. 85, no. 3 Pt. A., pp. 711-715, 2013.
(283) J. Friedrich, R. Ebner and L. A. Kunz-Schughart, "Experimental anti-tumor therapy in 3-D:
spheroids-old hat or new challenge?," International Journal of Radiation Biology, vol. 83, no. 11- 12, pp. 849-871, 2007.
(284) S. Chintharlapalli, S. Papineni, P. Lei, S. Pathi and S. Safe, "Betulinic acid inhibits colon cancer cell and tumor growth and induces proteasome- dependent and -independent downregulation of specificity proteins (Sp) transcription factors," BMC Cancer, vol. 11, pp. 371-383, 2011.
(285) A. Rajput, I. Dominguez San Martin, R. Rose, A. Beko, C. LeVea, E. Sharratt, R. Mazurchuk, R. M.
Hoffman, M. G. Brattain and J. Wang, "Characterization of HCT116 Human Colon Cancer Cells in an Orthotopic Model," Journal of Surgical Research, vol. 147, no. 2, pp. 276-281, 2008.
(286) G. Deng, D. L. Zhao, G. C. Li, H. Yu and G. J. Teng, "Combination therapy of transcatheter arterial chemoembolization and arterial administration of antiangiogenesis on VX2 liver tumor,"
Cardiovascular and Interventional Radiology, vol. 34, no. 4, pp. 824-832, 2011.
(287) F. Yamaguchi, T. Asakura, H. Takahashi, T. Kitamura and A. Teramoto, "Low frequency
ultrasonication induced antitumor effect in 5-aminolevulinic acid treated malignant glioma," Journal of Cancer Therapy, vol. 4, no. 1, pp. 170-175, 2013.
(288) M. Ackermann, I. M. Carvajal, B. A. Morse, M. Moreta, S. O'Neil, S. Kossodo, J. D. Peterson, V.
Delventhal, H. N. Marsh, E. S. Furfine and M. A. Konerding, "Adnectin CT-322 inhibits tumor growth and affects microvascular architecture and function in Colo205 tumor xenografts," International Journal of Oncology, vol. 38, no. 1, pp. 71-80, 2011.
(289) B. Bao, K. Groves, J. Zhang, E. Handy, P. Kennedy, G. Cuneo, C. T. Supuran, W. Yared, M.
Rajopadhye and J. D. Peterson, "In vivo imaging and quantification of carbonic anhydrase IX expression as an endogenous biomarker of tumor hypoxia.," PLoS One, vol. 7, no. 11, p. e50860, 2012.
(290) X. Montet, J. L. Figueiredo, H. Alencar, V. Ntziachristos, U. Mahmood and R. Weissleder,
"Tomographic fluorescence imaging of tumor vascular volume in mice," Radiology, vol. 242, no. 3, pp. 751-758, 2007.
(291) T. Jiang, R. Mo, A. Bellotti and J. &. G. Z. Zhou, "Drug Delivery: Gel-Liposome-Mediated Co- Delivery of Anticancer Membrane-Associated Proteins and Small-Molecule Drugs for Enhanced Therapeutic Efficacy," Advanced Functional Materials, vol. 24, no. 16, p. 2258, 2014.
(292) N. Jain, B. Gupta, N. Thakur, R. Jain, J. Banweer, D. Jain and S. Jain, "Phytosome: A Novel Drug Delivery System for Herbal Medicine," International Journal of Pharmaceutical Sciences and Drug Research, vol. 2, pp. 224-228, 2010.
(293) K. Avgoustakis, A. Beletsi, Z. Panagi, P. Klepetsanis, A. Karydas and D. Ithakissios, "PLGA-mPEG nanoparticles of cisplatin: in vitro nanoparticle degradation, in vitro drug release and in vivo drug residence in blood properties," 7 Control Release, vol. 79, no. 1-3, pp. 123-135, 2002.
(294) N. Franken, H. Rodermond, J. Stap, J. Haveman and C. van Bree, "Clonogenic assay of cells in vitro," Nat. Protoc, vol. 1, no. 5, pp. 2315-2319, 2006.
(295) Y. Okuda, H. Nakamura, K. Yoshida, H. Enomoto, H. Uyama, T. Hirotani, M. Funamoto, H. Ito, A. Everett, T. Hada and I. Kawase, "Hepatoma-derived growth factor induces tumorigenesis in vivo through both direct angiogenic activity and induction of vascular endothelial growth factor," Cancer Sci., vol. 94, no. 12, pp. 1034-1041, 2003.
(296) P. Wylie and W. Bowen, "Determination of cell colony formation in a high-content screening
assay.," Clin Lab Med., vol. 27, no. 1, pp. 193-199, 2007.
(297) D. Guidolin, G. Albertin and D. Ribatti, "Exploring in vitro angiogenesis by image analysis and
mathematical modeling," Microscopy: Science, Technology, Applications and Education, vol. 2, pp. 876-884, 2010.
(298) Y. Wang, L. Huang, Y. Yang, L. Xu, J. Yang and W. Y., "Effects of autocrine vascular endothelial growth factor (VEGF) in non-small cell lung cancer cell line A549," Mol Biol Rep, vol. 40, no. 4, pp. 3093-3099, 2013.
(299) X. Liu, J. Liu, Y. Guan, H. Li, L. Huang, H. Tang and J. He, "Establishment of an orthotopic lung
cancer model in nude mice and its evaluation by spiral CT," J Thorac Dis, vol. 4, no. 2, pp. 141-145, 2012.
(300) P. Zhang, W. Gao, S. Turner and B. Ducatman, "Gleevec (STI-571) inhibits lung cancer cell growth (A549) and potentiates the cisplatin effect in vitro," Mol Cancer, vol. 2, no. 1, p. 1, 2003.
(301) M. Tomayko and C. Reynolds, "Determination of subcutaneous tumor size in athymic (nude) mice," Cancer Chemother Pharmacol., vol. 24, no. 3, pp. 148-154, 1989.
(302) O. Firuzi, A. Lacanna, R. Petrucci, G. Marrosu and L. Saso, "Evaluation of the anti-oxidant activity of flavonoids by "ferric reducing anti-oxidant power" assay and cyclic voltammetry," vol. 1721, no. 1-3, pp. 174-184, 2005.
(303) S. Benvenuti, F. Pellatil, M. Melegari and D. Bertelli, "Polyphenols, Anthocyanins, Ascorbic Acid, and Radical Scavenging Activity of Rubus, Ribes, and Aronia.," Journal of Food Science, vol. 69, no. 3, pp. FCT164-FCT169, 2004.
(304) R. Re, N. Pellegrini, A. Proteggente and C. Rive-Evans, "Antioxidant activity applying a improved ABTS radical cation assay," Free Radical Biology and Medicine, vol. 26, no. 9-10, pp. 1231-1237, 1999.
(305) A. Kara elik, M. Ku uk, Z. iskefiyeli, S. Aydemir, S. De Smet, B. Miserez and P. Sandra, "Antioxidant components of Viburnum opulus L. determined by on-line HPLC-UV-ABTS radical scavenging and LC-UV- ESI-MS methods.," Food Chemistry, vol. 175, pp. 106-114, 2015.
(306) G. Ellman, K. Courtney, V. J. Andres and R. Feather-Stone, "A new and rapid colorimetric
determination of acetylcholinesterase activity," Biochem Pharmacol, vol. 7, pp. 88-95, 1961.
(307) A. Shukia, A. Rasik and G. Patnaik, "Depletion of Reduced Glutathione, Ascorbic Acid, Vitamin E and Antioxidant Defence Enzymes in a Healing Cutaneous Wound," Free Radic. Res., vol. 26, no. 2, pp. 93-101, 1997.
(308) Y. Tabana, F. Al-Suede, M. Ahamed, S. Dahham, L. Hassan, S. Khalilpour, M. Taleb-Agha, D. Sandai, A. Majid and A. Majid, "Cat's whiskers (Orthosiphon stamineus) tea modulates arthritis pathogenesis via the angiogenesis and inflammatory cascade.," BMC Complement Altern Med., vol. 16, no. 1, pp. 480-491, 2016.
(309) B. Ahamed, V. Krishna, H. R. H. Gowrdu, H. Kumaraswamy, S. Rajeshkarappa, C. Dandin and K.
Mahadevan, "Isolation of Bactericidal Constituents from the Stem Bark Extract of Grewia tiliaefolia Vahl.," Research Journal of Medicinal Plant, vol. 1, no. 3, pp. 72-82, 2007.